Adrenal Gland Questions
Normal Laboratory Reference values
| Laboratory Test | Normal Range in US Units | Normal Range in SI Units | To Convert U.S. to SI Units |
| ALT (Alanine aminotransferase) | F 7-30 units/L | F 0.12-0.50 µkat/L | x 0.01667 |
| M 10-55 units/L | M 0.17-0.92 µkat/L | ||
| Albumin | 3.1 – 4.3 g/dL | 31 – 43 g/L | x 10 |
| Alkaline Phosphatase | F 30-100 units/L M 45-115 units/L | F 0.5-1.67 µkat/L M 0.75-1.92 µkat/L | x 0.01667 |
| Amylase (Serum) | 53-123 units/L | 0.88-2.05 nkat/L | x 0.01667 |
| AST (Aspartate aminotransferase) | F 9-25 units/L | F 0.15-0.42 µkat/L | x 0.01667 |
| M 10-40 units/L | M 0.17-0.67 µkat/L | ||
| Basophils | 0-3% of lymphocytes | 0.0-0.03 fraction of white blood cells | x 0.01 |
| Bilirubin – Direct | 0.0-0.4 mg/dL | 0-7 µmol/L | x 17.1 |
| Bilirubin – Total | 0.0-1.0 mg/dL | 0-17 µmol/L | |
| Blood pressure | Normal: 120/70 to 120/80 millimeters of mercury (mmHg). Top number is systolic pressure, when heart is pumping. Bottom number is diastolic pressure when heart is at rest. Blood pressure can be too low (hypotension) or too high (hypertension). | No conversion | |
| C peptide | 0.5-2.0 ng/mL | 0.17-0.66 nmol/L | x 0.33 |
| Calcium, serum | 8.5-10.5 mg/dL | 2.1-2.6 mmol/L | x 0.25 |
| Calcium, urine | 0-300 mg/24hr | 0.0-7.5 mmol/24hr | x 0.025 |
| CO2 (Bicarbonate) | 20-32 mmol/L | 20-32 mmol/L | No conversion |
| Chloride | 95-108 mmol/L | 95-108 mmol/L | No conversion |
| Cholesterol, Total | <200 mg/dL | <5.17 mmol/L | x 0.02586 |
| Marginal | 200-239 mg/dL | 5.17-6.18 mmol/L | |
| High | >239 mg/dl | >6.18 mmol/L | |
| Cholesterol, LDL | <100 mg/dL | <2.59 mmol/L | |
| Marginal | 100-159 mg/dL | 2.59-4.14 mmol/L | |
| High | 160-189 mg/dL | 4.14 – 4.89 mmol/L | |
| Very High | >190 mg/dL | >4.91 mmol/L | |
| Cholesterol, HDL | >60 mg/dL | >1.55 mmol/L | |
| Moderate | 40-60 mg/dL | 1.03-1.55 mmol/L | |
| Low (heart risk) | <40 mg/dL | <1.03 mmol/L | |
| Cortisol: serum free (urine) | 0-25 µg/dL (depends on time of day) | 0-690 nmol/L | x 27.59 |
| 20-70 µg/dL | 55-193 nmol/24hr | x 2.759 | |
| Creatine kinase | F 40-150 units/L M 60-400 units/L | F 0.67-2.50 µkat/L M 1.00-6.67 µkat/L | x 0.01667 |
| Creatinine (urine) | F 0.6-1.8 g/day M 0.8-2.4 g/day | F 5.3-15.9 mmol/day M 7.1-21.2 mmol/day | x 88.4 |
| DHEA | F 130-980 ng/dL M 180-1250 ng/dL | F 4.5-34.0 nmol/L M 6.24-43.3 nmol/L | x 0.03467 |
| DHEA Sulfate | F Pre-menopause: 12-535 µg/dL | F Pre-menopause: 120-5350 µg/L | x 10 |
| F Post-menopause: 30-260 µg/dL | F Post-menopause: 300-2600 µg/L | ||
| M 10-619 µg/dL | M 100-6190 µg/L | ||
| Eosinophils | 0-8% of white blood cells | 0.0-0.8 fraction of white blood cells | x 0.01 |
| Erythrocyte sedimentation rate (Sed Rate) | F £ 30 mm/h M £ 20 mm/h | F £ 30 mm/h M £ 20 mm/h | No conversion |
| Folate | 3.1-17.5 ng/mL | 7.0-39.7 nmol/L | x 2.266 |
| Glucose, urine | <0.05 g/dl | <0.003 mmol/L | x 0.05551 |
| Glucose, plasma | 70-110 mg/dL | 3.9-6.1 mmol/L | |
| Gamma glutamyl transferase (GGT) | F £ 45 U/L M £ 65 U/L | F £ 45 U/L M £ 65 U/L | No conversion |
| Laboratory Test | Normal Range in U.S. Units | Normal Range in SI Units | To Convert US to SI Units |
| Hematocrit | F 36.0-46.0% of red blood cells | F 0.36-0.46 fraction of red blood cells | x 0.01 |
| M 37.0-49.0% of red blood cells | M 0.37-0.49 fraction of red blood cells | ||
| Hemoglobin | F 12.0-16.0 g/dL M 13.0-18.0 g/dL | F 7.4-9.9 mmol/L M 8.1-11.2 mmol/L | x 0.6206 |
| Lactate dehydrogenase (LDH) (total) | £ 270 U/L | £ 4.5 µkat/L | X 0.016667 |
| Lactic acid | 0.5-2.2 mmol/L | 0.5-2.2 mmol/L | No conversion |
| Leukocytes (WBC) | 4.5-11.0 x 103/mm3 | 4.5-11.0 x 109/liter | No conversion |
| Lymphocytes | 16-46% of white blood cells | 0.16-0.46 fraction of white blood cells | x 0.01 |
| Mean corpuscular hemoglobin (MCH) | 25.0-35.0 pg/cell | 25.0-35.0 pg/cell | No conversion |
| Mean corpuscular hemoglobin concentration (MCHC) | 31.0-37.0 g/dL | 310-370 g/L | x 10 |
| Mean corpuscular volume (MCV) | F 78-102 µm3 M 78-100 µm3 | F 78-102 fl M 78-100 fl | No conversion |
| Monocytes | 4-11% of white blood cells | 0.04-0.11 fraction of white blood cells | x 0.01 |
| Neutrophils | 45-75% of white blood cells | 0.45-0.75 fraction of white blood cells | x 0.01 |
| Phosphorus | 2.5-4.5 mg/dL | 0.81-1.45 mmol/L | X 0.323 |
| Platelets (Thrombocytes) | 130-400 x 103/µL | 130-400 x 109/L | No conversion |
| Potassium | 3.4-5.0 mmol/L | 3.4-5.0 mmol/liter | No conversion |
| Red Blood Cell Count (RBC) | F 3.9-5.2 x 106/µL M 4.4–5.8 x 106/µL | F 3.9-5.2 x 1012/L M W 4.4-5.8 x 1012/L | No conversion |
| Sodium | 135-145 mmol/liter | 135-145 mmol/liter | No conversion |
| Testosterone, total (morning sample) | F 6-86 ng/dL | F 0.21-2.98 nmol/liter | x 0.03467 |
| M 270-1070 ng/dL | M 9.36-37.10 nmol/liter | ||
| Testosterone, Age 20-40
Unbound Age 41-60
Age 61-80 | F 0.6-3.1 pg/mL M 15.0-40.0 pg/mL | F 20.8-107.5 pmol/liter M 520-1387 pmol/liter | x 34.67 |
| F 0.4-2.5 pg/mL M 13.0-35.0 pg/mL | F 13.9-86.7 pmol/liter M 451-1213 pmol/liter | ||
| F 0.2-2.0 pg/mL M 12.0-28.0 pg/mL | F 6.9-69.3 pmol/liter M 416-971 pmol/liter | ||
| Triglycerides Normal (fasting) Borderline High Very High | 40-150 mg/dL 150-200 mg/dL 200-500 mg/dL >500 mg/dL | 0.45-1.69 mmol/liter 1.69-2.26 mmol/liter 2.26-5.65 mmol/liter >5.65 mmol/liter | x 0.01129 |
| Urea, plasma (BUN) | 8-25 mg/dL | 2.9-8.9 mmol/liter | x 0.357 |
| Urinalysis: pH Specific gravity | 5.0-9.0 | 5.0-9.0 | No conversion |
| 1.001-1.035 | 1.001-1.035 | ||
| WBC (White blood cells, Leukocytes) | 4.5-11.0 x 103/mm3 | 4.5-11.0 x 109/liter | No conversion |
Quiz Summary
0 of 90 Questions completed
Questions:
Information
You have already completed this quiz. You cannot start it again.
Quiz is loading…
You must sign in or sign up to take this quiz.
You must first complete the following:
Results
Quiz complete. Results are being recorded.
Results
0 of 90 Questions answered correctly
Time has elapsed.
You have reached 0 of 0 point(s), (0)
Earned Point(s): 0 of 0, (0)
0 Essay(s) Pending (Possible Point(s): 0)
Categories
- Not categorized 0%
- Board Review Endocrinology 0%
- 1
- 2
- 3
- 4
- 5
- 6
- 7
- 8
- 9
- 10
- 11
- 12
- 13
- 14
- 15
- 16
- 17
- 18
- 19
- 20
- 21
- 22
- 23
- 24
- 25
- 26
- 27
- 28
- 29
- 30
- 31
- 32
- 33
- 34
- 35
- 36
- 37
- 38
- 39
- 40
- 41
- 42
- 43
- 44
- 45
- 46
- 47
- 48
- 49
- 50
- 51
- 52
- 53
- 54
- 55
- 56
- 57
- 58
- 59
- 60
- 61
- 62
- 63
- 64
- 65
- 66
- 67
- 68
- 69
- 70
- 71
- 72
- 73
- 74
- 75
- 76
- 77
- 78
- 79
- 80
- 81
- 82
- 83
- 84
- 85
- 86
- 87
- 88
- 89
- 90
- Current
- Review
- Answered
- Correct
- Incorrect
- 1. Question
A patient is undergoing biochemical testing for a pheochromocytoma. Which of these medications should be discontinued prior to testing?
CorrectIncorrect - 2. Question
Which of these statements regarding endogenous hypercortisolism is inaccurate?
CorrectIncorrect - 3. Question
A 30-year-old man with poorly controlled hypertension diagnosed 3 months prior is referred for evaluation of secondary hypertension, due to a unilateral adrenal tumor. The patient is on amlodipine 10mg daily, lisinopril 20mg daily and HCTZ 12.5mg daily. He has no axillary freckling or café au lait spots. He has bilateral hemangiomas. His plasma aldosterone concentration/plasma renin activity and low dose overnight dexamethasone test were both normal. Both his plasma and urine norepinephrine and normetanephrines were elevated at 5x the upper limit of normal. A dedicated adrenal CT scan showed a right-sided 4cm adrenal lesion. The lesion was about 20 Hounsfield units on the precontrast exam. What is the most likely diagnosis?
CorrectIncorrect - 4. Question
A 46-year-old woman with PCOS, T2DM presents to your office with recently diagnosed hypertension which is refractory to medical therapy. She endorses recent deepening of voice and excessive hair growth representing a marked change from her baseline. Patient has Ferriman-Gallway score of 20 and significant clitoromegaly. What is the diagnosis of this patient?
CorrectIncorrect - 5. Question
A 46-year-old morbidly obese woman is noted to have an adrenal incidentaloma. A dedicated adrenal CT scan is significant for a lipid-rich adenoma. She has no positive discriminatory clinical findings of Cushing’s disease. A 1mg overnight dexamethasone suppression test is 5.8mcg/dL (reference range <1.8mcg/dL). What should be done next?
CorrectIncorrect - 6. Question
A 47-year-old man undergoes a contrast CT scan of the chest as part of an evaluation of suspected pulmonary embolism. He is found to have a 1.2cm left adrenal nodule for which he was referred to your office. The patient has no positive discriminatory findings of hypercortisolemia. Which of these statements is inaccurate?
CorrectIncorrect - 7. Question
A 57-year-old woman presents to the emergency room with a 5-week history of progressively worsening hirsutism and weight loss. Her serum cortisol and DHEA-Sulphate levels are both 4 times the upper limit of normal. There is an 8cm right adrenal lesion measuring over 20 HU with a delayed contrast washout. An FDG PET scan shows localized disease in the right adrenal bed. What is the recommended management approach?
CorrectIncorrect - 8. Question
Which of these pathophysiologic mechanisms is incorrect, with regards to primary hyperaldosteronism?
CorrectIncorrect - 9. Question
A 45-year-old woman presents with resistant hypertension. She
developed hypokalemia while taking amlodipine and
hydrochlorothiazide. Lisinopril and potassium chloride
supplements (80 mEq daily) were added, with eventual
resolution of the hypokalemia but without normalization of blood
pressure. She has also gained 22 lb (10 kg) over the last 2 years
and now has diet-controlled diabetes mellitus.
On physical examination, she has mild dermal atrophy and three
1-cm bruises on her arms and legs from minimal trauma.
Proximal muscle strength is normal. Her blood pressure is
148/95 mm Hg, and she has no dorsocervical fat pad or striaeLaboratory test results:
• Serum sodium = 138 mEq/L (136-142 mEq/L)
(SI: 138 mmol/L [136-142 mmol/L])• Serum potassium = 3.6 mEq/L (3.5-5.0 mEq/L)
(SI: 3.6 mmol/L [3.5-5.0 mmol/L])• Serum glucose = 157 mg/dL (70-99 mg/dL)
(SI: 8.7 mmol/L [3.9-5.5 mmol/L])• Serum aldosterone = 13 ng/dL (4-21 ng/dL)
(SI: 361 pmol/L [111-583 pmol/L])• Plasma renin activity = <0.6 ng/mL per h (0.6-4.3 ng/mL per h)
• Serum creatinine = 0.8 mg/dL (0.6-1.1 mg/dL)
(SI: 70.7 μmol/L [53.0-97.2 μmol/L])• Plasma metanephrines, normal

Abdominal CT with contrast demonstrates a 3.8-cm left adrenal
mass and an atrophic right adrenal gland (see image, arrows).
The patient is referred to you for further evaluation and
recommendations.Which of the following is the best next step?CorrectIncorrect - 10. Question
Which of these clinical features is not an indication for screening for pheochromocytomas and paraganglioma syndromes (PPGLs)
CorrectIncorrect - 11. Question
A 27-year-old woman was diagnosed at birth with classic
21-hydroxylase deficiency and has been adherent to treatment
with hydrocortisone and fludrocortisone acetate her entire life.
She had vaginal reconstruction at age 19 years and has been
using dilators periodically since then. For the last 18 months, she
has been sexually active and wants to have children, but she
has not conceived despite optimally timed intercourse. She
currently takes hydrocortisone, 10 mg upon waking and 5 mg
with both lunch and her evening meal, plus fludrocortisone
acetate, 0.1 mg with breakfast. She has regular monthly menses
and shaves her upper lip and chin once a month. Home urine
testing documents monthly ovulation.On physical examination, she has no moon facies, no striae or
facial plethora, no acne, and a trace of shaved stubble.Which of the following is the key laboratory
parameter to monitor when adjusting her
glucocorticoid therapy?CorrectIncorrect - 12. Question
54-year-old man with a history of hypertension, atrial fibrillation and congestive heart failure AHA stage C, NYHA Class III. He is on carvedilol, candesartan, aspirin, 80mEq of potassium chloride and spironolactone is admitted to the heart failure service. The medicine intern orders plasma aldosterone and renin levels after noting a history of recurrent hypokalemia in this patient. The patient’s plasma aldosterone concentration is elevated at 35ng/dL with an undetectable plasma renin activity of <0.001ng/dl/hr. Which of these statements is valid?
CorrectIncorrect - 13. Question
A patient with nonmetastatic adrenal PPGL is referred to your clinic for genetic counseling and testing. He has a history of pancreatic cysts and CNS angiomas. His plasma and urinary fractionated metanephrines showed an elevated level of metanephrines, approximately 4 times above the upper limit of normal. Which of these genetic tests should be ordered first?
CorrectIncorrect - 14. Question
A patient is being evaluated for primary hyperaldosteronism, his plasma renin and aldosterone levels are however low. Which of these conditions is not a cause of pseudo primary hyperaldosteronism?
CorrectIncorrect - 15. Question
Which of these statements about testing conditions for pheochromocytomas is inaccurate?
CorrectIncorrect - 16. Question
A patient is being evaluated for a pheochromocytoma. Which of these assumptions is inaccurate?
CorrectIncorrect - 17. Question
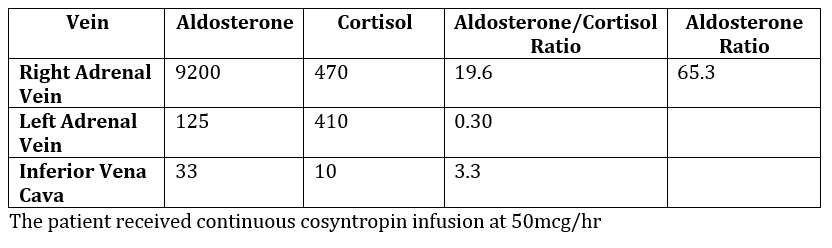
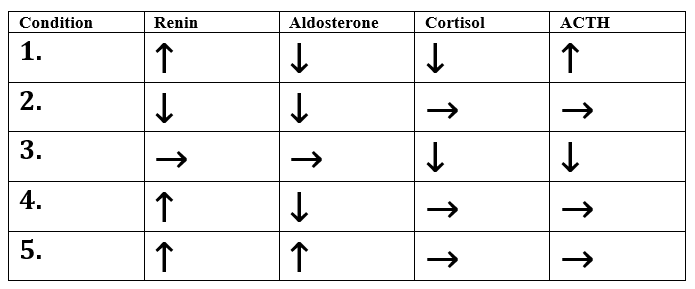
Interpret this adrenal venous sampling (AVS) report and recommend the next step in this patient’s management
CorrectIncorrect - 18. QuestionCorrectIncorrect
- 19. Question
In comparing adrenalectomy with medical therapy for primary hyperaldosteronism, which of these statements is inaccurate?
CorrectIncorrect - 20. Question
Which of these physical examination findings is not a positive discriminatory sign in Cushing’s disease?
CorrectIncorrect - 21. Question
A 46-year-old woman with no notable medical history has
developed paroxysms of nausea and hypertension over the past
6 months. During one such episode, she went to the emergency
department and was subsequently hospitalized for a blood
pressure of 200/110 mm Hg. An evaluation for a suspected
pheochromocytoma is in progress, and the patient has not yet
received adrenergic blockade.Which of the following treatments for nausea is
contraindicated in this patient?CorrectIncorrect - 22. Question
You are asked to provide consultation for a 28-year-old man with
possible adrenal insufficiency. He was seen in the emergency
department 10 days ago for unexplained hypotension following a
party, and an etiology was not identified. He recovered with fluid
resuscitation and a single dose of dexamethasone, 10 mg
intravenously. He received no further glucocorticoids and takes
no medication or nutritional supplements. Since discharge, he
has had some intermittent malaise and fatigue but no
hypotension, and his appetite is normal. He comes to a clinic
appointment today at 4 PM, and the question posed is whether
he suffers from adrenal insufficiency as the cause of his
hypotensive episode.Which laboratory test result obtained at this time will
conclusively exclude adrenal insufficiency?CorrectIncorrect - 23. Question
A 54-year-old man has a 2.2-cm mass in the left adrenal gland
incidentally noted on CT performed to evaluate hematuria. The
mass is homogeneous, the density is 30 Hounsfield units before
contrast, and there is 30% washout at 15 minutes. His blood
pressure is 122/78 mm Hg, and he reports no symptoms of
sweating, palpitations, or headache. He takes no medications,
but he has a positive family history of hypertension developing
after age 50 years.Laboratory test results:
• Plasma metanephrine = 670 pg/mL (<99 pg/mL)
(SI: 3.4 nmol/L [<0.5 nmol/L])
• Plasma normetanephrine = 641 pg/mL (<165 pg/mL)
(SI: 3.5 nmol/L [<0.9 nmol/L])
• Serum cortisol after 1 mg dexamethasone = 0.5 μg/dL (SI: 13.8 nmol/L)The CT image before contrast is shown (see image).
Which of the following is the most appropriate
next step in this patient’s management?CorrectIncorrect - 24. Question
A 32-year-old woman has a history of Cushing disease status
post surgery 3 years ago with subsequent improvement in her
diabetes mellitus and hypertension. She has noted weight gain,
poor sleep, irregular menses, and worsening glycemia for the
past 6 months. Her medications include amlodipine, 10 mg daily,
and metformin, 1500 mg daily.
On physical examination, her blood pressure is 145/85 mm Hg.
She has facial plethora and moderate supraclavicular fat pads.Laboratory test results:
• Fasting glucose = 205 mg/dL (70-99 mg/dL)
(SI: 11.4 mmol/L [3.9-5.5 mmol/L])
• Potassium = 2.7 mEq/L (3.5-5.0 mEq/L)
(SI: 2.7 mmol/L [3.5-5.0 mmol/L])
• Serum cortisol (8 AM) = 18 μg/dL (5-25 μg/dL)
(SI: 497 nmol/L [138-690 nmol/L])
• Hemoglobin A1c = 8.5% (4.0%-5.6%)
(69 mmol/mol [20-38 mmol/mol])
• Plasma ACTH = 65 pg/mL (10-60 pg/mL)
(SI: 14.3 pmol/L [2.2-13.2 pmol/L])
• Late-night salivary cortisol = 0.32 μg/dL (<0.13 μg/dL)
(SI: 8.8 nmol/L [<3.6 nmol/L])
• Urinary free cortisol = 360 μg/24 h (4-50 μg/24 h)
(SI: 994 nmol/d [11-138 nmol/d])
• Serum hCG (qualitative), negativePituitary MRI shows only postoperative changes.
After a discussion of treatment options, you plan
to begin mifepristone, 300 mg daily.Before starting mifepristone, you should first
treat her to achieve which of the following?CorrectIncorrect - 25. Question
A 68-year-old man is diagnosed with primary aldosteronism after
having difficult-to-control hypertension with intermittent
hypokalemia for at least 10 years and microalbuminuria for the
last 2 years. Adrenal venous sampling demonstrates bilateral
hyperaldosteronism, and you begin medical therapy with
eplerenone, 50 mg daily, added to amlodipine, 10 mg daily. Over
6 weeks, his blood pressure falls from 158/96 mm Hg to 135/88
mm Hg, and you increase the eplerenone dosage to 50 mg twice
daily. After another 8 weeks, his blood pressure is 125/82 mm Hg.
On the basis of these results, which of the
following changes would you make to his
blood pressure therapy?CorrectIncorrect - 26. Question
A 38-year-old woman is referred for evaluation of adrenal
nodularity. She reports weight gain of 11 lb (5 kg), poor sleep,
and easy bruising over the last 2 years.
On physical examination, her blood pressure is 144/92 mm Hg.
She has moderate facial plethora with rounding, dermal atrophy,
and disproportionate supraclavicular fat pads. She cannot rise
from a squat, and she has several 2- to 3-cm bruises on her legs.Laboratory test results:
• Serum cortisol after 1 mg dexamethasone =
4.0 μg/dL (SI: 110.4 nmol/L)
• Serum DHEA-S =
110 μg/dL (31-228 μg/dL) (SI: 3.0 μmol/L [0.8-6.8 μmol/L])
• Hemoglobin A1c =
7.3% (4.0%-5.6%) (56 mmol/mol [20-38 mmol/mol])
• Plasma ACTH =
5 pg/mL (10-60 pg/mL) (SI: 1.1 pmol/L [2.2-13.2 pmol/L])
• Urinary free cortisol =
62 μg/24 h (4-50 μg/24 h) (SI: 171 nmol/d [11-138 nmol/d])Abdominal CT shows bilateral adrenal nodularity, 4 x 3 cm on
the right side and 2 x 2 cm on the left side (see image).
Which of the following would you recommend as the
best next step in this patient’s management?CorrectIncorrect - 27. Question
After inferior petrosal sinus sampling and MRI, she undergoes
transsphenoidal surgery. The morning after surgery, her cortisol
value is 2.5 μg/dL (69.0 nmol/L). Candesartan is discontinued,
and she is discharged on a regimen of hydrocortisone, 10 mg 3
times daily with meals.
She returns today 4 weeks after surgery. She describes diffuse
muscle aches, fatigue, anorexia, and sleeping 10 to 12 hours a
day. She feels worse than before the surgery.
On physical examination, her blood pressure is 120/80 mm Hg
and pulse rate is 70 beats/min without orthostatic changes. Her
cushingoid features are beginning to resolve, and she has lost
8 lb (3.6 kg).Laboratory test results in clinic:
Serum sodium =
136 mEq/L (136-142 mEq/L) (SI: 136 mmol/L [136-142 mmol/L])
Serum potassium =
4.4 mEq/L (3.5-5.0 mEq/L) (SI: 4.4 mmol/L [3.5-5.0 mmol/L])
Fasting glucose =
80 mg/dL (70-99 mg/dL) (SI: 4.4 mmol/L [3.9-5.5 mmol/L])
Serum cortisol (8 AM) before first dose of hydrocortisone =
<0.5 μg/dL (5-25 μg/dL) (SI: <13.8 nmol/L [137.9-389.7 nmol/L])
DHEA-S =
<15 μg/dL (18-244 μg/dL) (SI: <0.4 μmol/L [0.5-6.6 μmol/L])
Basal plasma ACTH =
<4 pg/mL (10-60 pg/mL) (SI: <0.9 pmol/L [2.2-13.2 pmol/L])
Surgical pathology reveals a pituitary adenoma with Crooke hyaline
change, and immunohistochemistry for ACTH is positive.Which of the following is responsible for this
patient’s symptoms?CorrectIncorrect - 28. Question
A 21-year-old woman is referred for evaluation of unwanted
facial hair, acne, and irregular menses. She developed pubic
hair and body odor at age 5 years and was the tallest girl in her
class until she stopped growing at age 11 years. She developed
acne and facial hair at age 12 years and menarche was at age
14 years. Her menses have always been irregular, and she has
not menstruated for 8 months.
On physical examination, the patient has coarse terminal hairs
and shaved stubble on her chin, upper lip, and sides of her face.
She has acne on her forehead. Findings on pelvic examination,
including external genitalia, are normal. She has no moon
facies, dermal atrophy, myopathy, striae, or acanthosis nigricans.
Her blood pressure is 120/80 mm Hg, and BMI is 23 kg/m2.Screening laboratory test results
(sample drawn at 1 PM in the follicular phase):
• Serum cortisol =
6.0 μg/dL (2-14 μg/dL) (SI: 166 nmol/L [55-386 nmol/L])
• Serum DHEA-S =
680 μg/dL (44-332 μg/dL) (SI: 18.4 μmol/L [1.2-9.0 μmol/L])
• Serum 17-hydroxyprogesterone =
300 ng/dL (<80 ng/dL [follicular])
(SI: 9.1 nmol/L [<2.4 nmol/L])
• Serum total testosterone =
75 ng/dL (8-60 ng/dL) (SI: 2.6 nmol/L [0.3-2.1 nmol/L])
• SHBG = 1.0 μg/mL (2.2-14.6 μg/mL) (SI: 8.9 nmol/L [20-130 nmol/L])
• Serum prolactin =
10 ng/mL (4-30 ng/mL) (SI: 0.4 nmol/L [0.2-1.3 nmol/L])
• Serum glucose =
70 mg/dL (70-99 mg/dL) (SI: 3.9 mmol/L [3.9-5.5 mmol/L])Which of the following is the most appropriate
next step in this patient’s evaluation?CorrectIncorrect - 29. Question
A 57-year-old man sees you for an annual visit for management
of hypothyroidism. He has been on a stable levothyroxine dosage
for 9 years and previously had normal blood pressure at each
visit. He is not taking any other prescription medications.
On physical examination, he is a healthy-appearing, overweight,
middle-aged man. His blood pressure today, however, is 162/102
mm Hg, pulse rate is 74 beats/min, and BMI is 26.0 kg/m2. His
thyroid gland is small and firm, and other physical examination
findings are normal.Routine laboratory test results:
• Sodium = 141 mEq/L (136-142 mEq/L)
(SI: 141 mmol/L [136-142 mmol/L])
• Potassium = 2.8 mEq/L (3.5-5.0 mEq/L)
(SI: 2.8 mmol/L [3.5-5.0 mmol/L])
• TSH = 1.2 mIU/L (0.5-5.0 mIU/L)
• Serum cortisol after 1 mg dexamethasone =
<0.2 g/dL (SI: <5.5 nmol/L)After receiving these results, you take a thorough dietary history.
The patient admits that he is now taking a daily weight-loss
supplement containing extract of authentic licorice.Which of the following biochemical profiles do
you expect to find in this patient? CorrectIncorrect
CorrectIncorrect - 30. Question
After discussing options, you decide to treat her with
metyrapone, 500 mg 4 times daily, for inoperable Cushing
disease. She returns in 2 weeks with slight weight loss and feels
modestly better, but her serum cortisol level is unchanged. You
increase her metyrapone dosage to 750 mg 4 times daily. She
returns 2 weeks later complaining of severe fatigue, anorexia,
myalgias, and poor sleep.Laboratory test results while taking metyrapone
(performed on hospital autoanalyzer):
• Serum cortisol 2 hours after morning metyrapone dose =
25 g/dL (SI: 690 nmol/L)
• Serum potassium = 3.5 mEq/L (SI: 3.5 mmol/L)
• Serum glucose = 46 mg/dL (SI: 2.6 mmol/L)Which of the following tests will help you to
adjust the metyrapone dosage?CorrectIncorrect - 31. Question
A 57-year-old woman was diagnosed with a pancreatic
gastrinoma 10 years ago, when she presented with duodenal
ulcers and abdominal pain. At the time of the resection, CT
demonstrated a 1.3-cm pancreatic primary tumor and a single 4-
cm hepatic metastasis. She underwent resection of the primary
tumor and liver metastasis and was treated with depot
octreotide, 30 mg every 4 weeks. Pathology showed a welldifferentiated
neuroendocrine tumor with a Ki-67 index (reflecting
mitotic rate) of 1%. She remained well, but serial imaging
demonstrated gradual appearance of multiple liver metastases
(all <1 cm) with slight interval growth each year. In the 3 months
since her last CT, she abruptly developed hypertension and
hypokalemia, diabetes mellitus, poor sleep, muscle weakness,
and depression.On physical examination, her blood pressure is 167/96 mm Hg.
She has a flat affect with slow response to commands,
2+ bilateral pedal edema, and muscle weakness.
Laboratory test results:
• Serum potassium = 2.8 mEq/L (3.5-5.0 mEq/L)
(SI: 2.8 mmol/L [3.5-5.0 mmol/L])
• Serum cortisol (random) = 120 μg/dL (5-25 μg/dL)
(SI: 3311 nmol/L [138-390 nmol/L])
• Plasma ACTH = 750 pg/mL (10-60 pg/mL)
(SI: 165.0 pmol/L [2.2-13.2 pmol/L])
• Fasting serum gastrin = 95 pg/mL (<100 pg/mL) (SI: 95 ng/L [<100 ng/L])
• Serum albumin = 4.1 g/dL (3.5-5.0 g/dL) (SI: 41 g/L [35-50 g/L])
• Hemoglobin A1c = 8.2% (4.0%-5.6%) (66 mmol/mol [20-38 mmol/mol])On repeated CT, the liver metastases are not measurably
changed from the scan 3 months ago. The adrenal glands are
somewhat thickened but have no tumors.Which of the following is the most appropriate
next step in this patient’s management?CorrectIncorrect - 32. Question
A 27-year-old woman with a history of systemic lupus
erythematosus presents to the emergency department for
evaluation of a 4-day history of nausea, vomiting, fatigue, and
orthostasis. She was diagnosed with lupus 2 years ago when she
presented with nephritis and arthralgias. She received a 12-week
course of prednisone up to 60 mg daily. Since then, she has been
maintained on alternate-day prednisone, 5 mg daily, with control
of her arthralgias and normal renal function. She was well until 8
weeks ago, when she developed deep venous thrombosis in her
right leg and antiphospholipid syndrome was diagnosed. Warfarin
was added and titrated to achieve an INR in the target range. She
became acutely ill 4 days ago with flank pain, but no fever or
dysuria, and she has been unable to take her pills for the past
4 days.Laboratory test results:
• Sodium = 121 mEq/L (136-142 mEq/L)
(SI: 121 mmol/L [136-142 mmol/L])
• Potassium = 6.4 mEq/L (3.5-5.0 mEq/L)
(SI: 6.4 mmol/L [3.5-5.0 mmol/L])
• Plasma ACTH = 1330 pg/mL (10-60 pg/mL)
(SI: 292.6 pmol/L [2.2-13.2 pmol/L])
• Serum aldosterone = <2 ng/dL (4-21 ng/dL)
(SI: <551 pmol/L [111-583 pmol/L])
• Plasma direct renin = 350 pg/mL (4-44 pg/mL)
(SI: 8.3 pmol/L [0.1-1.0 pmol/L])
• Serum cortisol (8 AM) = <0.5 μg/dL (5-25 μg/dL)
(SI: 14 nmol/L [138-390 nmol/L])Which of the following tests will reveal the
cause of her adrenal insufficiency?CorrectIncorrect - 33. Question
A 52-year-old man with hypertension and hypokalemia is
completing evaluation for primary aldosteronism.
Screening laboratory test results:
• Sodium = 147 mEq/L (136-142 mEq/L)
(SI: 147 mmol/L [136-142 mmol/L])
• Potassium = 3.2 mEq/L (3.5-5.0 mEq/L)
(SI: 3.2 mmol/L [3.5-5.0 mmol/L])
• Serum aldosterone = 24 ng/dL (4-21 ng/dL)
(SI: 666 pmol/L [111-583 pmol/L])
(repeated measurement = 26 ng/dL [SI: 721 pmol/L])
• Plasma renin activity =
<0.6 ng/mL per h (0.6-4.3 ng/mL per h)
(repeated measurement = <0.6 ng/mL per h)CT with fine cuts of the adrenal demonstrates
normal-appearing glands.
He undergoes adrenal venous sampling with continuous infusion of
cosyntropin at 50 mcg per hour. The results are shown (see table).
How do you interpret the results of the adrenal
venous sampling study?CorrectIncorrect - 34. Question
You are asked to evaluate a 67-year-old woman with a right
adrenal mass that was incidentally discovered on an annual
surveillance CT performed for a medical history of colon cancer.
She was treated with partial colectomy and adjuvant
chemotherapy 6 years ago. The adrenal mass measures 2.2 cm
in maximal diameter with a precontrast attenuation value of 25
Hounsfield units and 30% contrast washout at 10 minutes. The
mass was not visible on CT 1 year ago.
On physical examination, her blood pressure is 123/84 mm Hg
and pulse rate is 70 beats/min. She is clinically well and has no
cushingoid features.Laboratory test results:
• Serum glucose = 90 mg/dL (70-99 mg/dL)
(SI: 5.0 mmol/L [3.9-5.5 mmol/L])
• Serum potassium = 4.0 mEq/L (3.5-5.0 mEq/L)
(SI: 4.0 mmol/L [3.5-5.0 mmol/L])
• Plasma metanephrine = <39 pg/mL (<99 pg/mL)
(SI: <0.2 nmol/L [<0.5 nmol/L])
• Plasma normetanephrine = <147 pg/mL (<165 pg/mL)
(SI: 0.8 nmol/L [<0.9 nmol/L])
• Serum cortisol after 1-mg dexamethasone = 0.8 μg/dL
(SI: 22.1 nmol/L)Which of the following is the best next step?
CorrectIncorrect - 35. Question
A 24-year-old woman is new to your practice for follow-up of
adrenal insufficiency. She had adrenal crisis at birth and has been
treated with hydrocortisone and fludrocortisone acetate her entire
life. At age 12 years, she experienced breast budding and
progressed to Tanner stage 3 breast development. She then had
spontaneous menses 3 times over the next year but not since, and
she has been given cyclic estrogen and progestin, with menstrual
bleeding occurring monthly since age 16 years. She has limited
knowledge about her adrenal insufficiency – just that her adrenal
glands were very large when she was diagnosed as an infant.On physical examination, she is a well-appearing young woman
without syndromic features. Her blood pressure is 116/72 mm
Hg, and pulse rate is 74 beats/min. She has mild hyperpigmentation
of the palmar creases, Tanner stage 5 breasts,
scant pubic hair without virilization, and a normal thyroid gland.Which of the following patterns would you
predict for her laboratory test results? CorrectIncorrect
CorrectIncorrect - 36. Question
A 26-year-old man is referred by his primary care physician for
management of classic 21-hydroxylase deficiency. The patient was
diagnosed at birth and received treatment with hydrocortisone and
fludrocortisone throughout childhood. He stopped all medications
at age 22 years until he had an adrenal crisis 6 months ago and
nearly died. At hospital discharge, he agreed to take prednisone,
7.5 mg daily, and fludrocortisone acetate, 0.1 mg daily. He has
been adherent to this regimen and states that he feels better now
than when he was untreated.On physical examination, he appears healthy and has no
cushingoid features. He is a short, muscular young man with a
blood pressure of 116/81 mm Hg and pulse rate of 66 beats/min.Laboratory test results:
• Serum sodium = 135 mEq/L (136-142 mEq/L)
(SI: 135 mmol/L [136-142 mmol/L])
• Serum potassium = 4.2 mEq/L (3.5-5.0 mEq/L)
(SI: 4.2 mmol/L [3.5-5.0 mmol/L])
• Plasma renin activity = 2.4 ng/mL per h (0.6-4.3 ng/mL per h)
• Serum androstenedione = 880 ng/dL (65-210 ng/dL)
(SI: 30.7 nmol/L [2.3-7.3 nmol/L])
• Serum total testosterone = 420 ng/dL (300-900 ng/dL)
(SI: 14.6 nmol/L [10.4-31.2 nmol/L])Which of the following is the most important
test to order next?CorrectIncorrect - 37. Question
A 28-year-old man is diagnosed with autoimmune adrenal insufficiency
and hypothyroidism. He presented with a 25-lb (11.4 kg) weight loss and
adrenal crisis during a gastrointestinal illness. He was discharged from
the hospital taking hydrocortisone, 20 mg upon waking in the morning
and 10 mg in the early afternoon, as well as levothyroxine, 125 mcg daily.
He regained most of his lost weight over the next 6 months and remained
well without additional crises. For convenience, his glucocorticoid was
changed to methylprednisolone, 6 mg upon waking. He has continued to
slowly regain his lost weight, but he now experiences a generalized
feeling of fatigue throughout the day, which does not improve shortly
after taking the methylprednisolone. He has even tried dividing his daily
dose (3 mg upon waking and 3 mg in the early afternoon), but he did not
experience relief from the fatigue following either dose.On physical examination, his blood pressure is 104/66 mm Hg
and pulse rate is 88 beats/min. He has no purple striae, facial
rounding, dermal atrophy, vitiligo, or bruises.Laboratory test results:
• Sodium = 138 mEq/L (136-142 mEq/L)
(SI: 138 mmol/L [136-142 mmol/L])
• Potassium = 4.9 mEq/L (3.5-5.0 mEq/L)
(SI: 4.9 mmol/L [3.5-5.0 mmol/L])
• Plasma ACTH = 400 pg/mL (10-60 pg/mL)
(SI: 88.0 pmol/L [2.2-13.2 pmol/L])
• Plasma renin activity = 13.4 ng/mL per h (0.6-4.3 ng/mL per h)
• Serum TSH = 2.2 mIU/L (0.5-5.0 mIU/L)Which of the following changes do you
recommend in his management?CorrectIncorrect - 38. Question
An 84-year-old man is referred by an oncologist for
evaluation of nonsuppressible testosterone. Prostate
cancer was diagnosed 3 years ago, and he received local
radiotherapy followed by degarelix (long-acting GnRH
antagonist, androgen-deprivation therapy). His PSA
concentration remained less than 1.0 ng/mL (<1.0 μg/L)
for 2 years, but over the last year it has risen to 15.0
ng/mL (15.0 μg/L).A 99Tc bone scan shows bone metastases, and subsequent CT
shows bilateral 5- to 7-cm adrenal masses.
In retrospect, the masses were present (but slightly smaller) on
baseline CT 3 years ago.Laboratory test results:
• Serum LH = <0.8 mIU/mL (1.0-9.0 mIU/mL)
(SI: <0.8 IU/L [1.0-9.0 IU/L])
• Serum FSH = <0.2 mIU/mL (1.0-13.0 mIU/mL)
(SI: <0.2 IU/L [1.0-13.0 mIU/mL])
• Serum total testosterone = 120 ng/dL (300-900 ng/dL)
(SI: 4.2 nmol/L [10.4-31.2 nmol/L])
LH, FSH, and total testosterone are measured again 1 week
later and similar values are documented.The following test results are also obtained:
• Serum androstenedione = 340 ng/dL (65-210 ng/dL)
(SI: 11.9 mmol/L [2.3-7.3 mmol/L])
• Plasma ACTH = 70 pg/mL (10-60 pg/mL) (SI: 15.4 pmol/L [2.2-13.2 pmol/L])
• Serum aldosterone = 3 ng/dL (4-21 ng/dL) (SI: 83 pmol/L [111-583 pmol/L])
• Plasma renin activity = 1.8 ng/mL per h (0.6-4.3 ng/mL per h)
• Serum DHEA-S = 90 μg/dL (25-131 μg/dL) (SI: 2.4 μmol/L [0.7-3.6 μmol/L])
• Plasma metanephrine = 39 pg/mL (<99 pg/mL)
(SI: <0.2 nmol/L [<0.5 nmol/L])
• Plasma normetanephrine = 202 pg/mL (<165 pg/mL)
(SI: 1.1 nmol/L [<0.9 nmol/L])
• Serum cortisol:
• Baseline 8 AM = 11 μg/dL (5-25 μg/dL) (SI: 303 nmol/L [138-390 nmol/L])
• After 1 mg dexamethasone = <1 μg/dL (SI: <28 nmol/L)On physical examination, he is a well-appearing elderly man
in minimal pain. His blood pressure is 106/72 mm Hg and
pulse rate is 84 beats/min. Both testes are 4 to 6 mL, firm,
and slightly irregular.Which of the following diagnostic studies
would provide a diagnosis?CorrectIncorrect - 39. Question
A 67-year-old woman presents with weakness and edema of
6 months’ duration.
On physical examination, she has large supraclavicular and mild
dorsocervical fat pads with slight facial plethora and 1+ bilateral
pitting edema. She has several ecchymoses on the arms and
legs, significant dermal atrophy, and no striae. She is alert and
conversant with moderately reduced proximal and distal muscle
strength.Laboratory test results:
• Potassium = 3.3 mEq/L (3.5-5.0 mEq/L)
(SI: 3.3 mmol/L [3.5-5.0 mmol/L])
• Plasma ACTH = values in the range of 50-80 pg/mL (10-60 pg/mL)
(SI: values in the range of 11.0-17.6 pmol/L [2.2-13.2 pmol/L])
• Urinary free cortisol = 85 μg/24 h (4-50 μg/24 h)
(SI: 235 nmol/d [11-138 nmol/d])
• Serum cortisol after dexamethasone = 17 μg/dL (SI: 469 nmol/L)MRI of the pituitary (T1-weighted image with gadolinium
contrast) is interpreted as normal (see image):
CT of the chest/abdomen/pelvis shows enlarged adrenal glands
and a 9-mm vascular mass in the pancreas, interpreted as being
consistent with a neuroendocrine tumor (see image, arrow).
Which of the following is the best next step in
this patient’s evaluation and management?CorrectIncorrect - 40. Question
A 53-year-old man is referred for evaluation of primary
aldosteronism. He developed resistant hypertension in
his late 40s and was found to be hypokalemic 6 months
ago on routine blood testing.Screening laboratory test results:
• Sodium = 147 mEq/L (136-142 mEq/L)
(SI: 147 mmol/L [136-142 mmol/L])
• Potassium = 3.2 mEq/L (3.5-5.0 mEq/L)
(SI: 3.2 mmol/L [3.5-5.0 mmol/L])
• Serum aldosterone = 33 ng/dL (4-21 ng/dL)
(SI: 915 pmol/L [111-583 pmol/L])
• Plasma renin activity = <0.6 ng/mL per h (0.6-4.3 ng/mL per h)On the third day of a high-salt diet:
• Urinary sodium = 280 mEq/24 h (280 mmol/d)
• Urinary aldosterone = 40 g/24 h (111 nmol/d)CT with fine cuts of the adrenals shows minor irregularities in
both glands but no conclusive tumors. Adrenal venous sampling
was delayed for 4 months, and his serum potassium and blood
pressure were controlled with spironolactone, 25 mg daily. He
was told to stop the spironolactone 2 weeks before adrenal
venous sampling.He undergoes adrenal venous sampling with continuous infusion
of cosyntropin at 50 mcg per h. As he is leaving the interventional
radiology suite, however, he informs the staff that he forgot to stop
the spironolactone, and he took his last dose the previous day. A
week later, you receive the laboratory results (see table).
How do you interpret the results of the adrenal venous sampling study?
CorrectIncorrect - 41. Question
A 48-year-old woman has a whole-body MRI at a wellness center
as part of an executive physical evaluation. The study found a
1.5-cm right adrenal tumor. She self-refers herself to your clinic to
ask what she should do about the tumor. You do not have the
films, but the report states that the mass has “loss of signal on
out-of-phase images and low signal on T2-weighted images.”
On physical examination, her blood pressure is normal, and she
has no cushingoid stigmata. You tell her that based on current
guidelines, you recommend screening for cortisol and
catecholamine production with a 1-mg overnight dexamethasone
suppression test and 24-hour urinary metanephrines.Which feature of this case most conclusively favors
that the mass is a benign cortical adenoma?CorrectIncorrect - 42. Question
An 18-year-old man is referred for follow-up of adrenal
insufficiency, which he developed at age 13 years. He
takes hydrocortisone, 15 mg upon waking and 5 mg in the
early afternoon, plus fludrocortisone acetate, 0.2 mg daily.
He also takes fluconazole, 150 mg once weekly, for
recurrent episodes of oral thrush since age 10 years. An
older sibling died suddenly at age 5 of unknown causes.On physical examination, his height is 64 in (162.6 cm) and
weight is 110 lb (50 kg) (BMI = 18.9 kg/m2). He has thin nails
and brown horizontal bands on his teeth without oral thrush (see
image). His blood pressure is 115/75 mm Hg, and pulse rate is
70 beats/min. He has no hyperpigmentation or vitiligo.
Laboratory test results (sample drawn at 9 AM):
• Serum sodium = 142 mEq/L (136-142 mEq/L)
(SI: 142 mmol/L [136-142 mmol/L])
• Serum potassium = 3.9 mEq/L (3.5-5.0 mEq/L)
(SI: 3.9 mmol/L [3.5-5.0 mmol/L])
• Plasma ACTH = 250 pg/mL (10-60 pg/mL)
(SI: 55.0 pmol/L [2.2-13.2 pmol/L])
• Plasma direct renin = 33 pg/mL (30-40 pg/mL)
(SI: 0.8 pmol/L [0.7-1.0 pmol/L])
• Serum 21-hydroxylase antibodies = 70 U/mL (<1 U/mL)Which of the following other endocrinopathies
is he most at risk to develop?CorrectIncorrect - 43. Question
A 51 year old female with borderline hypotension and nonspecific symptoms is on admission. You are consulted for evaluation of adrenal insufficiency. Her early morning cortisol is 8 mcg/dL. You order a random DHEA sulphate at 3pm and the level is reported as normal.
What would you recommend next?
CorrectIncorrect - 44. Question
Category: Board Review Endocrinology
Which of the following is the most common cause of corticotropin (ACTH) deficiency and consequent adrenal insufficiency?
CorrectIncorrectConsider the treatment-related cause that is most commonly associated with ACTH deficiency.
- 45. Question
Category: Board Review Endocrinology
In patients with secondary and tertiary adrenal insufficiency, which clinical manifestation is typically absent?
CorrectIncorrectConsider which clinical manifestation is related to the primary adrenal insufficiency but not to secondary and tertiary types.
- 46. Question
Category: Board Review Endocrinology
Which hormone level may be moderately elevated during the day in patients with untreated adrenal insufficiency?
CorrectIncorrectConsider the hormone that is involved in the regulation of the normal circadian rhythm.
- 47. Question
Category: Board Review Endocrinology
In the evaluation of an acutely ill patient with a possible adrenal crisis, when should therapy be started?
CorrectIncorrectConsider the urgency of treatment initiation in a patient with a possible adrenal crisis.
- 48. Question
Category: Board Review Endocrinology
Which of the following stages in the development of adrenal insufficiency is characterized by high plasma renin activity and normal or low serum aldosterone?
CorrectIncorrectConsider the earliest stage in the development of adrenal insufficiency.
- 49. Question
Category: Board Review Endocrinology
In patients with abnormalities of cortisol-binding globulin (CBG) or albumin, which diagnostic measurement should be interpreted with caution?
CorrectIncorrectConsider the diagnostic measurement that is most commonly used but may be affected by CBG or albumin abnormalities.
- 50. Question
Category: Board Review Endocrinology
What is the most crucial factor in diagnosing adrenal insufficiency of any cause?
CorrectIncorrectConsider the primary hormone affected in adrenal insufficiency.
- 51. Question
Category: Board Review Endocrinology
An early morning serum cortisol concentration less than 3 mcg/dL (80 nmol/L) is strongly suggestive of which condition?
CorrectIncorrectConsider the condition that is characterized by low cortisol levels.
- 52. Question
Category: Board Review Endocrinology
A 46-year-old male presents with fatigue, weight loss, and recurrent episodes of nausea and vomiting. The patient's blood tests show hyponatremia and hyperkalemia. Which test should be performed to confirm the diagnosis of adrenal insufficiency?
CorrectIncorrectThink about the test that involves stimulation of the adrenal gland.
- 53. Question
Category: Board Review Endocrinology
A patient has been diagnosed with adrenal insufficiency. Which of the following tests is used to determine whether the adrenal insufficiency is primary, secondary, or tertiary?
CorrectIncorrectLook for the test that measures a hormone responsible for stimulating cortisol production.
- 54. Question
Category: Board Review Endocrinology
A patient presents with a morning serum cortisol concentration of 4 mcg/dL. What can be concluded from this result?
CorrectIncorrectThink about the diagnostic value of a single low morning serum cortisol concentration.
- 55. Question
Category: Board Review Endocrinology
A patient with suspected adrenal insufficiency has a morning serum cortisol concentration of 20 mcg/dL. What can be concluded from this result?
CorrectIncorrectRecall the normal range for morning serum cortisol concentration and its predictive value for adrenal function
- 56. Question
Category: Board Review Endocrinology
A 45-year-old woman presents with fatigue, weight loss, and hypotension. Her laboratory results show a low morning serum cortisol level, and an ACTH stimulation test is planned. What is the best time to perform the ACTH stimulation test to avoid a falsely abnormal result in a healthy subject?
CorrectIncorrectCortisol responses are greatest in the morning for healthy individuals.
- 57. Question
Category: Board Review Endocrinology
A patient with suspected adrenal insufficiency is undergoing an ACTH stimulation test. What is the minimum peak serum cortisol concentration after 30 or 60 minutes to be considered a normal response to the high-dose (250 mcg) ACTH stimulation test?
CorrectIncorrectA normal response to the high-dose (250 mcg) ACTH stimulation test is a rise in serum cortisol concentration after either 30 or 60 minutes to a specific peak value.
- 58. Question
Category: Board Review Endocrinology
A patient with a history of pituitary surgery has a subnormal response to the high-dose ACTH stimulation test. How long after surgery should the test be performed to have the best diagnostic performance?
CorrectIncorrectThe adrenal glands in patients with recent-onset ACTH deficiency have not yet become completely atrophic and are still capable of responding to ACTH stimulation.
- 59. Question
Category: Board Review Endocrinology
A 35-year-old man presents with signs of adrenal insufficiency. The physician suspects secondary adrenal insufficiency and plans to perform a test to confirm the diagnosis. Which test is considered the single best (and simplest) test for confirming a diagnosis of chronic secondary adrenal insufficiency?
CorrectIncorrectThe single best (and simplest) test for confirming a diagnosis of chronic secondary adrenal insufficiency is one of the ACTH stimulation tests.
- 60. Question
Category: Board Review Endocrinology
A patient with suspected secondary adrenal insufficiency undergoes an insulin-induced hypoglycemia test. What should be the target blood glucose level to achieve during the test?
CorrectIncorrectThe target blood glucose level during an insulin-induced hypoglycemia test is quite low, aiming to achieve a specific level or less.
- 61. Question
Category: Board Review Endocrinology
A patient with tertiary adrenal insufficiency undergoes a corticotropin-releasing hormone (CRH) test. How would their ACTH response differ from a patient with secondary adrenal insufficiency?
CorrectIncorrectPatients with tertiary adrenal insufficiency due to lack of CRH from the hypothalamus have a specific type of ACTH response during a CRH test.
- 62. Question
Category: Board Review Endocrinology
A patient presents with acute adrenal insufficiency, and the physician decides to initiate treatment. What is the recommended initial treatment with hydrocortisone for a patient in adrenal crisis?
CorrectIncorrectThe recommended initial treatment with hydrocortisone for a patient in adrenal crisis involves an initial IV bolus followed by a smaller IV dose given at regular intervals.
- 63. Question
Category: Board Review Endocrinology
In patients with primary adrenal insufficiency, which two biochemical features are commonly observed during adrenal crisis?
CorrectIncorrectThe correct combination of biochemical features observed during adrenal crisis in patients with primary adrenal insufficiency involves abnormalities in both potassium and sodium levels.
- 64. Question
Category: Board Review Endocrinology
In the management of adrenal crisis, why is mineralocorticoid replacement not necessary acutely?
CorrectIncorrectMineralocorticoid replacement is not necessary acutely in the management of adrenal crisis because another intervention can achieve adequate sodium replacement.
- 65. Question
Category: Board Review Endocrinology
Which short-acting glucocorticoid is suggested for the management of chronic primary adrenal insufficiency?
CorrectIncorrectThe suggested short-acting glucocorticoid for the management of chronic primary adrenal insufficiency has a high bioavailability and can be administered in two or three divided doses.
- 66. Question
Category: Board Review Endocrinology
What is the primary goal when determining the optimal dose of glucocorticoid replacement therapy for a patient with chronic primary adrenal insufficiency?
CorrectIncorrectThe primary goal when determining the optimal dose of glucocorticoid replacement therapy for a patient with chronic primary adrenal insufficiency is to avoid a specific syndrome caused by overtreatment.
- 67. Question
Category: Board Review Endocrinology
What is the average daily secretion rate of cortisol in normal subjects?
CorrectIncorrectThe average daily secretion rate of cortisol in normal subjects is a range of values expressed in mg/m2/day.
- 68. Question
Category: Board Review Endocrinology
Which glucocorticoid is generally considered to be a better choice for a short-acting glucocorticoid regimen due to its shortcomings related to absorption and metabolism?
CorrectIncorrectThe better choice for a short-acting glucocorticoid
- 69. Question
Category: Board Review Endocrinology
What is one of the advantages of hydrocortisone therapy for patients with adrenal insufficiency?
CorrectIncorrectThe advantage of hydrocortisone therapy is related to adjusting the dose using different tablet strengths.
- 70. Question
Category: Board Review Endocrinology
Which long-acting glucocorticoids may be useful for patients who are non-compliant with multiple daily dose schedules?
CorrectIncorrectThe long-acting glucocorticoids useful for patients who are non-compliant with multiple daily dose schedules include a glucocorticoid starting with “P” and another starting with “D.”
- 71. Question
Category: Board Review Endocrinology
What is the main goal when monitoring the glucocorticoid dose in patients with adrenal insufficiency?
CorrectIncorrectThe main goal when monitoring the glucocorticoid dose in patients with adrenal insufficiency is to balance symptom relief with the avoidance of a specific syndrome caused by overtreatment.
- 72. Question
Category: Board Review Endocrinology
What is the main reason for patients with primary adrenal insufficiency to require mineralocorticoid replacement?
CorrectIncorrectThe main reason for requiring mineralocorticoid replacement in primary adrenal insufficiency is to prevent three related issues involving sodium and potassium levels.
- 73. Question
Category: Board Review Endocrinology
Which parameter can be used to monitor the adequacy of mineralocorticoid replacement in patients with adrenal insufficiency?
CorrectIncorrectThe parameter used to monitor the adequacy of mineralocorticoid replacement starts with the word “plasma” and is related to an enzyme.
- 74. Question
Category: Board Review Endocrinology
Why is mineralocorticoid replacement rarely required in patients with secondary adrenal insufficiency?
CorrectIncorrectThe reason why mineralocorticoid replacement is rarely required in patients with secondary adrenal insufficiency involves the regulation of aldosterone release.
- 75. Question
Category: Board Review Endocrinology
Which therapy has been studied to improve mood and quality of life in women with adrenal insufficiency?
CorrectIncorrect - 76. Question
Category: Board Review Endocrinology
What factors are associated with a higher risk of intraoperative hemodynamic instability during surgical resection of a pheochromocytoma?
CorrectIncorrectThe factors associated with a higher risk of intraoperative hemodynamic instability involve preoperative plasma norepinephrine concentration, tumor size, and postural blood pressure fall.
- 77. Question
Category: Board Review Endocrinology
Which medication is NOT appropriate for managing hypertensive crises during surgical resection of a pheochromocytoma?
CorrectIncorrectThe medication that is not appropriate for managing hypertensive crises during surgical resection of a pheochromocytoma is a diuretic.
- 78. Question
Category: Board Review Endocrinology
What should be monitored for the first 24 to 48 hours postoperatively in patients undergoing adrenalectomy for pheochromocytoma?
CorrectIncorrectThe parameter to be monitored postoperatively in patients undergoing adrenalectomy for pheochromocytoma is related to blood sugar levels.
- 79. Question
Category: Board Review Endocrinology
Which drug is recommended as the first-line option for preoperative alpha-adrenergic blockade in patients with pheochromocytoma?
CorrectIncorrectThe first-line drug for preoperative alpha-adrenergic blockade is an irreversible alpha-adrenergic antagonist.
- 80. Question
Category: Board Review Endocrinology
In patients with multiple endocrine neoplasia type 2 (MEN2) and evidence of bilateral disease >2 cm in diameter on imaging, what is the suggested surgical approach?
CorrectIncorrectThe surgical approach suggested for patients with MEN2 and evidence of bilateral disease >2 cm in diameter on imaging involves removing both adrenal glands completely.
- 81. Question
Category: Board Review Endocrinology
Which of the following is NOT a component of the classic triad of symptoms associated with pheochromocytoma?
CorrectIncorrectThe classic triad of symptoms associated with pheochromocytoma involves headache, sweating, and a cardiovascular symptom.
- 82. Question
Category: Board Review Endocrinology
For patients with von Hippel-Lindau (VHL) and evidence of bilateral disease on imaging, what surgical approach is generally suggested?
CorrectIncorrect - 83. Question
Category: Board Review Endocrinology
Which condition is most commonly associated with hyporeninemic hypoaldosteronism in patients aged 50 to 70 years?
CorrectIncorrectThe most common condition associated with hyporeninemic hypoaldosteronism in this age group is related to diabetes.
- 84. Question
Category: Board Review Endocrinology
What characteristic is common among patients with congenital adrenal hyperplasia and congenital isolated hypoaldosteronism regarding their serum values?
CorrectIncorrectThese two conditions share a characteristic related to low aldosterone levels.
- 85. Question
Category: Board Review Endocrinology
In patients with hyporeninemic hypoaldosteronism and hypertension or edema, what treatment approach is typically preferred over fludrocortisone?
CorrectIncorrectThe preferred treatment approach in this case involves dietary modification and a specific type of diuretics.
- 86. Question
Category: Board Review Endocrinology
Which test can help differentiate between various causes of hypoaldosteronism?
CorrectIncorrect - 87. Question
Category: Board Review Endocrinology
A 58-year-old male with a history of diabetes and chronic kidney disease presents with persistent hyperkalemia and mild metabolic acidosis. What is the most likely cause of his condition?
CorrectIncorrectConsider the patient's age, medical history, and clinical manifestations to determine the most likely cause of his condition.
- 88. Question
Category: Board Review Endocrinology
Which medication can lead to a reduction in plasma aldosterone concentrations due to its direct toxic effect on the adrenal zona glomerulosa cells?
CorrectIncorrectConsider the direct toxic effect of the medication on the adrenal zona glomerulosa cells.
- 89. Question
Category: Board Review Endocrinology
A patient with primary adrenal insufficiency requires mineralocorticoid replacement therapy. Which medication and dose should be prescribed for this patient?
CorrectIncorrectConsider the appropriate medication and dosage for mineralocorticoid replacement therapy in primary adrenal insufficiency.
- 90. Question
Category: Board Review Endocrinology
In the context of hyporeninemic hypoaldosteronism, why is fludrocortisone often not used despite its efficacy?
CorrectIncorrect