Thyroid Gland Questions
Normal Laboratory Reference values
| Laboratory Test | Normal Range in US Units | Normal Range in SI Units | To Convert U.S. to SI Units |
| ALT (Alanine aminotransferase) | F 7-30 units/L | F 0.12-0.50 µkat/L | x 0.01667 |
| M 10-55 units/L | M 0.17-0.92 µkat/L | ||
| Albumin | 3.1 – 4.3 g/dL | 31 – 43 g/L | x 10 |
| Alkaline Phosphatase | F 30-100 units/L M 45-115 units/L | F 0.5-1.67 µkat/L M 0.75-1.92 µkat/L | x 0.01667 |
| Amylase (Serum) | 53-123 units/L | 0.88-2.05 nkat/L | x 0.01667 |
| AST (Aspartate aminotransferase) | F 9-25 units/L | F 0.15-0.42 µkat/L | x 0.01667 |
| M 10-40 units/L | M 0.17-0.67 µkat/L | ||
| Basophils | 0-3% of lymphocytes | 0.0-0.03 fraction of white blood cells | x 0.01 |
| Bilirubin – Direct | 0.0-0.4 mg/dL | 0-7 µmol/L | x 17.1 |
| Bilirubin – Total | 0.0-1.0 mg/dL | 0-17 µmol/L | |
| Blood pressure | Normal: 120/70 to 120/80 millimeters of mercury (mmHg). Top number is systolic pressure, when heart is pumping. Bottom number is diastolic pressure when heart is at rest. Blood pressure can be too low (hypotension) or too high (hypertension). | No conversion | |
| C peptide | 0.5-2.0 ng/mL | 0.17-0.66 nmol/L | x 0.33 |
| Calcium, serum | 8.5-10.5 mg/dL | 2.1-2.6 mmol/L | x 0.25 |
| Calcium, urine | 0-300 mg/24hr | 0.0-7.5 mmol/24hr | x 0.025 |
| CO2 (Bicarbonate) | 20-32 mmol/L | 20-32 mmol/L | No conversion |
| Chloride | 95-108 mmol/L | 95-108 mmol/L | No conversion |
| Cholesterol, Total | <200 mg/dL | <5.17 mmol/L | x 0.02586 |
| Marginal | 200-239 mg/dL | 5.17-6.18 mmol/L | |
| High | >239 mg/dl | >6.18 mmol/L | |
| Cholesterol, LDL | <100 mg/dL | <2.59 mmol/L | |
| Marginal | 100-159 mg/dL | 2.59-4.14 mmol/L | |
| High | 160-189 mg/dL | 4.14 – 4.89 mmol/L | |
| Very High | >190 mg/dL | >4.91 mmol/L | |
| Cholesterol, HDL | >60 mg/dL | >1.55 mmol/L | |
| Moderate | 40-60 mg/dL | 1.03-1.55 mmol/L | |
| Low (heart risk) | <40 mg/dL | <1.03 mmol/L | |
| Cortisol: serum free (urine) | 0-25 µg/dL (depends on time of day) | 0-690 nmol/L | x 27.59 |
| 20-70 µg/dL | 55-193 nmol/24hr | x 2.759 | |
| Creatine kinase | F 40-150 units/L M 60-400 units/L | F 0.67-2.50 µkat/L M 1.00-6.67 µkat/L | x 0.01667 |
| Creatinine (urine) | F 0.6-1.8 g/day M 0.8-2.4 g/day | F 5.3-15.9 mmol/day M 7.1-21.2 mmol/day | x 88.4 |
| DHEA | F 130-980 ng/dL M 180-1250 ng/dL | F 4.5-34.0 nmol/L M 6.24-43.3 nmol/L | x 0.03467 |
| DHEA Sulfate | F Pre-menopause: 12-535 µg/dL | F Pre-menopause: 120-5350 µg/L | x 10 |
| F Post-menopause: 30-260 µg/dL | F Post-menopause: 300-2600 µg/L | ||
| M 10-619 µg/dL | M 100-6190 µg/L | ||
| Eosinophils | 0-8% of white blood cells | 0.0-0.8 fraction of white blood cells | x 0.01 |
| Erythrocyte sedimentation rate (Sed Rate) | F £ 30 mm/h M £ 20 mm/h | F £ 30 mm/h M £ 20 mm/h | No conversion |
| Folate | 3.1-17.5 ng/mL | 7.0-39.7 nmol/L | x 2.266 |
| Glucose, urine | <0.05 g/dl | <0.003 mmol/L | x 0.05551 |
| Glucose, plasma | 70-110 mg/dL | 3.9-6.1 mmol/L | |
| Gamma glutamyl transferase (GGT) | F £ 45 U/L M £ 65 U/L | F £ 45 U/L M £ 65 U/L | No conversion |
| Laboratory Test | Normal Range in U.S. Units | Normal Range in SI Units | To Convert US to SI Units |
| Hematocrit | F 36.0-46.0% of red blood cells | F 0.36-0.46 fraction of red blood cells | x 0.01 |
| M 37.0-49.0% of red blood cells | M 0.37-0.49 fraction of red blood cells | ||
| Hemoglobin | F 12.0-16.0 g/dL M 13.0-18.0 g/dL | F 7.4-9.9 mmol/L M 8.1-11.2 mmol/L | x 0.6206 |
| Lactate dehydrogenase (LDH) (total) | £ 270 U/L | £ 4.5 µkat/L | X 0.016667 |
| Lactic acid | 0.5-2.2 mmol/L | 0.5-2.2 mmol/L | No conversion |
| Leukocytes (WBC) | 4.5-11.0 x 103/mm3 | 4.5-11.0 x 109/liter | No conversion |
| Lymphocytes | 16-46% of white blood cells | 0.16-0.46 fraction of white blood cells | x 0.01 |
| Mean corpuscular hemoglobin (MCH) | 25.0-35.0 pg/cell | 25.0-35.0 pg/cell | No conversion |
| Mean corpuscular hemoglobin concentration (MCHC) | 31.0-37.0 g/dL | 310-370 g/L | x 10 |
| Mean corpuscular volume (MCV) | F 78-102 µm3 M 78-100 µm3 | F 78-102 fl M 78-100 fl | No conversion |
| Monocytes | 4-11% of white blood cells | 0.04-0.11 fraction of white blood cells | x 0.01 |
| Neutrophils | 45-75% of white blood cells | 0.45-0.75 fraction of white blood cells | x 0.01 |
| Phosphorus | 2.5-4.5 mg/dL | 0.81-1.45 mmol/L | X 0.323 |
| Platelets (Thrombocytes) | 130-400 x 103/µL | 130-400 x 109/L | No conversion |
| Potassium | 3.4-5.0 mmol/L | 3.4-5.0 mmol/liter | No conversion |
| Red Blood Cell Count (RBC) | F 3.9-5.2 x 106/µL M 4.4–5.8 x 106/µL | F 3.9-5.2 x 1012/L M W 4.4-5.8 x 1012/L | No conversion |
| Sodium | 135-145 mmol/liter | 135-145 mmol/liter | No conversion |
| Testosterone, total (morning sample) | F 6-86 ng/dL | F 0.21-2.98 nmol/liter | x 0.03467 |
| M 270-1070 ng/dL | M 9.36-37.10 nmol/liter | ||
| Testosterone, Age 20-40
Unbound Age 41-60
Age 61-80 | F 0.6-3.1 pg/mL M 15.0-40.0 pg/mL | F 20.8-107.5 pmol/liter M 520-1387 pmol/liter | x 34.67 |
| F 0.4-2.5 pg/mL M 13.0-35.0 pg/mL | F 13.9-86.7 pmol/liter M 451-1213 pmol/liter | ||
| F 0.2-2.0 pg/mL M 12.0-28.0 pg/mL | F 6.9-69.3 pmol/liter M 416-971 pmol/liter | ||
| Triglycerides Normal (fasting) Borderline High Very High | 40-150 mg/dL 150-200 mg/dL 200-500 mg/dL >500 mg/dL | 0.45-1.69 mmol/liter 1.69-2.26 mmol/liter 2.26-5.65 mmol/liter >5.65 mmol/liter | x 0.01129 |
| Urea, plasma (BUN) | 8-25 mg/dL | 2.9-8.9 mmol/liter | x 0.357 |
| Urinalysis: pH Specific gravity | 5.0-9.0 | 5.0-9.0 | No conversion |
| 1.001-1.035 | 1.001-1.035 | ||
| WBC (White blood cells, Leukocytes) | 4.5-11.0 x 103/mm3 | 4.5-11.0 x 109/liter | No conversion |
Quiz Summary
0 of 123 Questions completed
Questions:
Information
You have already completed this quiz. You cannot start it again.
Quiz is loading…
You must sign in or sign up to take this quiz.
You must first complete the following:
Results
Quiz complete. Results are being recorded.
Results
0 of 123 Questions answered correctly
Time has elapsed.
You have reached 0 of 0 point(s), (0)
Earned Point(s): 0 of 0, (0)
0 Essay(s) Pending (Possible Point(s): 0)
Categories
- Not categorized 0%
- Board Review Endocrinology 0%
- 1
- 2
- 3
- 4
- 5
- 6
- 7
- 8
- 9
- 10
- 11
- 12
- 13
- 14
- 15
- 16
- 17
- 18
- 19
- 20
- 21
- 22
- 23
- 24
- 25
- 26
- 27
- 28
- 29
- 30
- 31
- 32
- 33
- 34
- 35
- 36
- 37
- 38
- 39
- 40
- 41
- 42
- 43
- 44
- 45
- 46
- 47
- 48
- 49
- 50
- 51
- 52
- 53
- 54
- 55
- 56
- 57
- 58
- 59
- 60
- 61
- 62
- 63
- 64
- 65
- 66
- 67
- 68
- 69
- 70
- 71
- 72
- 73
- 74
- 75
- 76
- 77
- 78
- 79
- 80
- 81
- 82
- 83
- 84
- 85
- 86
- 87
- 88
- 89
- 90
- 91
- 92
- 93
- 94
- 95
- 96
- 97
- 98
- 99
- 100
- 101
- 102
- 103
- 104
- 105
- 106
- 107
- 108
- 109
- 110
- 111
- 112
- 113
- 114
- 115
- 116
- 117
- 118
- 119
- 120
- 121
- 122
- 123
- Current
- Review
- Answered
- Correct
- Incorrect
- 1. Question
Which of these causes of thyrotoxicosis does not result in normal or elevated radioactive iodine uptake in the neck on 1-123 scintigraphy?
CorrectIncorrect - 2. Question
Which of these medications does not reduce the conversion of circulating levels of free T4 into free T3?
CorrectIncorrect - 3. Question
Which of these is not an expected side effect of methimazole
CorrectIncorrect - 4. Question
Which of these statements about the natural history of Graves ophthalmopathy is incorrect.
CorrectIncorrect - 5. Question
A 47-year-old man with nonischemic cardiomyopathy complicated by atrial fibrillation is admitted to the heart failure service due to refractory atrial fibrillation. He is currently on metoprolol, amiodarone, lisinopril, spironolactone and soluble aspirin. His thyroid function test is remarkable for elevated free T3 and T4 levels, 4x above the upper limit of normal, with a suppressed TSH <0.01. The consulting endocrinologist is concerned about amiodarone-induced thyrotoxicosis. What is the best next step in elucidating the cause of amiodarone-induced thyrotoxicosis (AIT)?
CorrectIncorrect - 6. Question
A 32-year-old woman with a two-year history primary hypothyroidism in the setting of Hashimoto’s thyroiditis, presents to her primary care doctors office with chronic fatigue, hair loss, and weight gain. Her TSH is elevated at 53 (0.5-4.2). Her current dose of levothyroxine is 112mcg daily. Patient endorses compliance with therapy. She has no other medical comorbidities and is not any medications which might interfere with thyroid hormone absorption.
CorrectIncorrect - 7. Question
A 28-year-old female with Gestational diabetes mellitus presented with palpitations and insomnia during her six-week postpartum visit. She has no known history of thyroid disease. These were the results of her thyroid function tests.
TSH <0.01 (0.30 - 4.20) Free T3 5.2 pg/mL (2.0 - 4.4) Free T4 1.53 ng/dL (0.9 – 1.7)
The consulting endocrinologist is concerned about postpartum thyroiditis. What should be the next step in the evaluation of this patient?
CorrectIncorrect - 8. Question
45-year-old woman with an incidental 1.6cm thyroid nodule involving the isthmus. She has no history of thyroid disease, neck irradiation or a family history of thyroid cancer. She has no compressive neck symptoms or symptoms suggestive of thyroid dysfunction. There is a palpable firm isthmic nodule on physical examination but no cervical lymphadenopathy.
TSH is 2.4 mIU/L (0.5 to 5.0). Thyroid ultrasound shows a 1.6cm mixed cystic nodule. What should be done next?
CorrectIncorrect - 9. Question
Which of these is not a biochemical feature of the sick euthyroid syndrome?
CorrectIncorrect - 10. Question
A 62-year-old man with sporadic metastatic medullary thyroid carcinoma is referred to you for further management. He had a complete thyroidectomy 4 years prior and has since then been on active surveillance. His calcitonin levels have progressively increased over the past 2 years. There is evidence of pulmonary metastasis and locally aggressive disease in the neck threatening the airway. He is started on treatment and monitored based on the RECIST Response Evaluation Criteria in Solid Tumors criteria. What therapy was recently started due to this patient’s extensive disease?
CorrectIncorrect - 11. Question
Based on the American Thyroid Association guidelines which of these does not represent a low-risk thyroid nodule on thyroid ultrasound?
CorrectIncorrect - 12. Question
61-year-old Hispanic man with a known history of hypertension, obstructive sleep apnea and type 1 diabetes mellitus, is found to have an incidental thyroid nodule noted during a carotid ultrasound. He has a left thyroid lobe 0.8cm hypoechoic nodule with high-risk sonographic features. FNAB was suspicious for papillary thyroid cancer. He has no sonographic evidence of cervical lymphadenopathy. There is no family history of thyroid cancer. What would you recommend?
CorrectIncorrect - 13. Question
67-year-old Caucasian female is diagnosed with medullary thyroid cancer and undergoes total thyroidectomy and extensive neck dissection due to involved cervical lymph nodes. He has no family history of MTC and no personal history of primary hyperparathyroidism or pheochromocytoma. Which of these options is the next best step?
CorrectIncorrect - 14. Question
Which of these is not a cause of an inappropriately normal serum TSH in the setting of thyroid hormone excess (i.e elevated free T4)?
CorrectIncorrect - 15. Question
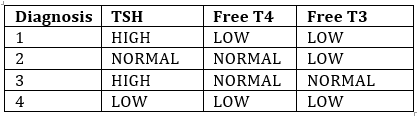
Which of these patterns of TSH and free thyroid hormone levels is consistent with acute nonthyroidal illness?
CorrectIncorrect - 16. Question
A 55-year-old woman presents with a rapid onset of dysphagia, dyspnea and progressive hoarseness of voice. Physical examination is consistent with a hard-thyroid gland and a positive Trousseau’s sign. The patient undergoes a total thyroidectomy. Histopathology of the parathyroid gland is consistent with extensive plasma cell infiltration. What is the recommended therapy of this patient’s primary diagnosis?
CorrectIncorrect - 17. Question
Which of these is not a recommended screen for patients on tyrosine kinase inhibitor therapy for progressive differentiated thyroid cancer.
CorrectIncorrect - 18. Question
A 72-year-old man with a huge nontoxic goiter presents with exertional dyspnea and a choking sensation of 4 weeks duration. Pemberton’s sign was positive. What is the most likely mechanism for this clinical sign?
CorrectIncorrect - 19. Question
A patient with Grade III Graves ophthalmopathy is evaluated in the endocrine clinic. Which of these is NOT a reason for unilateral eyelid retraction?
CorrectIncorrect - 20. Question
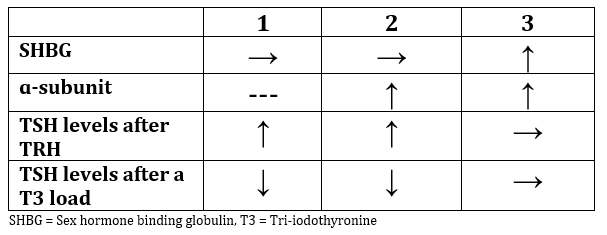
A patient is evaluated for an elevated serum free T4 and an inappropriately normal serum TSH. Which of these additional biochemical tests is consistent with a TSH secreting pituitary adenoma?
CorrectIncorrect - 21. Question
Which of these is not a reason why a patient with primary hypothyroidism may develop galactorrhea?
CorrectIncorrect - 22. Question
A 39-year-old female with class III obesity, celiac disease, and severe obstructive sleep apnea. Which of these is not an indication for treatment of subclinical hypothyroidism in this patient?
CorrectIncorrect - 23. Question
Category: Board Review Endocrinology
Which of the following effects does amiodarone have on thyroid function due to its intrinsic properties?
CorrectIncorrectThink about the effect of amiodarone on T4 metabolism.
- 24. Question
Category: Board Review Endocrinology
What is the Wolff-Chaikoff effect?
CorrectIncorrectConsider the effect of high intrathyroidal iodine concentrations on thyroid hormone synthesis.
- 25. Question
Category: Board Review Endocrinology
In iodine-sufficient areas, which type of amiodarone-induced thyroid dysfunction is more common?
CorrectIncorrectThink about the relationship between iodine intake and amiodarone-induced thyroid dysfunction.
- 26. Question
Category: Board Review Endocrinology
Amiodarone-induced hyperthyroidism is classified into two types. Which type is characterized by a destructive thyroiditis?
CorrectIncorrectConsider the two types of amiodarone-induced hyperthyroidism and their distinct characteristics.
- 27. Question
Category: Board Review Endocrinology
Patients with which underlying thyroid condition are more likely to develop amiodarone-induced hypothyroidism?
CorrectIncorrect - 28. Question
Category: Board Review Endocrinology
A 55-year-old male with a history of ventricular arrhythmias is on amiodarone therapy and presents with symptoms of hyperthyroidism. Lab results show a decrease in TSH and an increase in free T4 levels. What is the most likely cause of his hyperthyroidism?
CorrectIncorrectConsider the patient's medication history.
- 29. Question
Category: Board Review Endocrinology
In patients with amiodarone-induced thyrotoxicosis (AIT) type I, which of the following treatments is usually effective?
CorrectIncorrectConsider the mechanism of AIT type I.
- 30. Question
Category: Board Review Endocrinology
In patients with amiodarone-induced thyrotoxicosis (AIT) type II, which of the following treatments is usually effective?
CorrectIncorrectConsider the mechanism of AIT type II.
- 31. Question
Category: Board Review Endocrinology
In a patient with AIT type I who does not respond to thionamides and requires further intervention, which of the following treatments may be considered?
CorrectIncorrectConsider the available treatment options for refractory AIT type I.
- 32. Question
Category: Board Review Endocrinology
A patient with AIT type II is not responding to glucocorticoid therapy. What is the recommended next step in management?
CorrectIncorrectConsider the available treatment options for refractory AIT type II.
- 33. Question
Category: Board Review Endocrinology
A 45-year-old patient presents with fatigue and weight gain. They have been on amiodarone therapy for the past 6 months for atrial fibrillation. What is the most likely cause of their symptoms?
CorrectIncorrectConsider the side effects of amiodarone on thyroid function.
- 34. Question
Category: Board Review Endocrinology
Which type of amiodarone-induced thyrotoxicosis (AIT) is characterized by increased synthesis of thyroid hormone due to excess iodine from the amiodarone?
CorrectIncorrectReview the different types of AIT and their underlying mechanisms.
- 35. Question
Category: Board Review Endocrinology
In a patient with amiodarone-induced thyrotoxicosis who is also on warfarin, what should be monitored closely?
CorrectIncorrectConsider the effect of thyroid dysfunction on warfarin response.
- 36. Question
Category: Board Review Endocrinology
What is the first-line drug therapy for type II amiodarone-induced thyrotoxicosis?
CorrectIncorrectReview the treatment options for the different types of AIT.
- 37. Question
Category: Board Review Endocrinology
In a patient who develops amiodarone-induced hypothyroidism for which amiodarone was prescribed for life-threatening ventricular arrhythmias and is effective, what is the suggested course of action?
CorrectIncorrect - 38. Question
Category: Board Review Endocrinology
Which symptom is NOT associated with increased beta-adrenergic tone in hyperthyroidism?
CorrectIncorrectThink about the symptoms that result from increased beta-adrenergic activity.
- 39. Question
Category: Board Review Endocrinology
Which beta blocker has the ability to slowly decrease serum T3 concentrations by inhibiting the 5'-monodeiodinase?
CorrectIncorrectConsider the beta blocker that is highly lipid soluble.
- 40. Question
Category: Board Review Endocrinology
Which of the following conditions is NOT a contraindication for using beta blockers in hyperthyroid patients?
CorrectIncorrectLook for a condition that may actually benefit from beta blocker use.
- 41. Question
Category: Board Review Endocrinology
Which beta-1-selective drug is often used when patients have relative contraindications to beta blockade?
CorrectIncorrectConsider a beta-1-selective drug with single-daily dosing.
- 42. Question
Category: Board Review Endocrinology
In pregnant women with hyperthyroidism, which beta blocker is recommended for use at the lowest dose and shortest duration?
CorrectIncorrectChoose a beta blocker that has a lower risk of side effects during pregnancy.
- 43. Question
Category: Board Review Endocrinology
Which of the following is the primary receptor mediating the action of thyroid hormone on bone?
CorrectIncorrectThe primary receptor is found in rat and human osteoblast cell lines and osteoclasts derived from an osteoclastoma.
- 44. Question
Category: Board Review Endocrinology
Which of the following is a risk factor for fracture in patients with overt hyperthyroidism?
CorrectIncorrectOvert hyperthyroidism is associated with reduced bone density, osteoporosis, and increased fracture rate.
- 45. Question
Category: Board Review Endocrinology
In patients with overt hyperthyroidism, what is the effect of increased calcium release into the circulation on parathyroid hormone (PTH)?
CorrectIncorrectHypercalcemia in hyperthyroid patients suppresses the secretion of PTH, leading to hypercalciuria and negative calcium balance.
- 46. Question
Category: Board Review Endocrinology
What is the primary cause of negative calcium balance in patients with hyperthyroidism?
CorrectIncorrectHypercalcemia in hyperthyroid patients suppresses the secretion of PTH, leading to hypercalciuria and negative calcium balance.
- 47. Question
Category: Board Review Endocrinology
A common cause of endogenous subclinical hyperthyroidism is:
CorrectIncorrectThink about the common causes of subclinical hyperthyroidism.
- 48. Question
Category: Board Review Endocrinology
In postmenopausal women with subclinical hyperthyroidism, which of the following is associated with reduced bone density?
CorrectIncorrectConsider the relationship between TSH levels and bone density.
- 49. Question
Category: Board Review Endocrinology
Which of the following is a risk factor for osteoporosis in patients with subclinical hyperthyroidism?
CorrectIncorrectThink about the factors that increase the risk of osteoporosis in subclinical hyperthyroidism.
- 50. Question
Category: Board Review Endocrinology
In a patient with subclinical hyperthyroidism, which of the following treatments is appropriate for reducing the risk of skeletal complications?
CorrectIncorrectConsider the best approach to manage subclinical hyperthyroidism and its complications.
- 51. Question
Category: Board Review Endocrinology
Exogenous subclinical hyperthyroidism can result from:
CorrectIncorrectThink about the causes of exogenous subclinical hyperthyroidism.
- 52. Question
Category: Board Review Endocrinology
A patient with subclinical hyperthyroidism is most likely to show which of the following changes in bone and mineral metabolism?
CorrectIncorrectConsider the effect of subclinical hyperthyroidism on bone resorption markers.
- 53. Question
Category: Board Review Endocrinology
Which treatment has been shown to improve bone density in postmenopausal women with low BMD taking long-term thyroid hormone suppressive therapy for thyroid cancer?
CorrectIncorrectConsider the use of inhibitors of bone resorption.
- 54. Question
Category: Board Review Endocrinology
What are the main cardiovascular changes seen in hyperthyroidism?
CorrectIncorrectHyperthyroidism leads to increased cardiovascular activity.
- 55. Question
Category: Board Review Endocrinology
How do thyroid hormones mainly exert their cellular effects?
CorrectIncorrectThe cellular actions of thyroid hormone involve triiodothyronine (T3).
- 56. Question
Category: Board Review Endocrinology
Which of the following is a common cardiovascular symptom in patients with hyperthyroidism?
CorrectIncorrectHyperthyroidism often leads to increased heart rate.
- 57. Question
Category: Board Review Endocrinology
What is the most common arrhythmia associated with hyperthyroidism?
CorrectIncorrectThis arrhythmia is especially common in patients aged 60 or older.
- 58. Question
Category: Board Review Endocrinology
What is the primary treatment for heart failure caused by hyperthyroidism without underlying cardiac disease or arrhythmia?
CorrectIncorrect - 59. Question
Category: Board Review Endocrinology
Which of the following is the main autoantigen in Graves' disease?
CorrectIncorrectThis autoantigen is primarily expressed in the thyroid but is also expressed in other sites such as adipocytes and fibroblasts.
- 60. Question
Category: Board Review Endocrinology
What causes an increase in volume of both the extraocular muscles and orbital connective tissue in thyroid eye disease?
CorrectIncorrectThis increase in volume is associated with the displacement of the eyeball forward, leading to extraocular muscle dysfunction and impaired venous drainage causing periorbital swelling.
- 61. Question
Category: Board Review Endocrinology
Which cells play a crucial role in the pathogenesis of thyroid eye disease by activating orbital fibroblast and adipocyte TSHRs and IGF-1 receptors?
CorrectIncorrectThese cells initiate cellular expansion and orbital inflammation.
- 62. Question
Category: Board Review Endocrinology
What is the basis for the therapeutic use of teprotumumab in the treatment of thyroid eye disease?
CorrectIncorrectThis therapeutic agent targets a receptor that has significant crosstalk with the TSH receptor in orbital fibroblasts.
- 63. Question
Category: Board Review Endocrinology
Which of the following is NOT a risk factor for thyroid eye disease in patients with Graves' disease?
CorrectIncorrectnone
- 64. Question
Category: Board Review Endocrinology
Which symptom is NOT commonly associated with thyroid eye disease?
CorrectIncorrectnone
- 65. Question
Category: Board Review Endocrinology
What percentage of patients with thyroid eye disease have hyperthyroidism absent?
CorrectIncorrectnone
- 66. Question
Category: Board Review Endocrinology
Which of the following conditions does NOT present with eye signs simulating thyroid eye disease?
CorrectIncorrectReview the conditions listed in the differential diagnosis section.
- 67. Question
Category: Board Review Endocrinology
In which of the following timeframes does eye involvement most commonly appear relative to the onset of hyperthyroidism in patients with thyroid eye disease?
CorrectIncorrectnone
- 68. Question
Category: Board Review Endocrinology
Which of the following is the main autoantigen in thyroid eye disease?
CorrectIncorrectThe main autoantigen is expressed in orbital fibroblasts and forms a functional complex with another receptor.
- 69. Question
Category: Board Review Endocrinology
Which factor is NOT considered a risk factor for the development of thyroid eye disease?
CorrectIncorrectConsider lifestyle factors and medical treatments.
- 70. Question
Category: Board Review Endocrinology
Which of the following is NOT a typical sign of thyroid eye disease?
CorrectIncorrectThink about the signs related to the eyes and the surrounding tissue.
- 71. Question
Category: Board Review Endocrinology
What is the clinical activity score (CAS) used for in thyroid eye disease?
CorrectIncorrectConsider the purpose of CAS in relation to treatment.
- 72. Question
Category: Board Review Endocrinology
In moderate to severe thyroid eye disease, which imaging modality is preferred for assessment of the risk of future optic nerve compression and better bone visualization?
CorrectIncorrectConsider the benefits of each imaging modality and the use of contrast agents.
- 73. Question
Category: Board Review Endocrinology
A 35-year-old woman presents with weight loss, increased appetite, anxiety, and tremors. She also reports heat intolerance and increased perspiration. Based on these symptoms, which condition is most likely?
CorrectIncorrectConsider conditions that can cause weight loss, increased appetite, and heat intolerance.
- 74. Question
Category: Board Review Endocrinology
Which of the following symptoms is NOT typically associated with hyperthyroidism?
CorrectIncorrectThink about symptoms that are opposite to the typical symptoms of hyperthyroidism.
- 75. Question
Category: Board Review Endocrinology
In older patients with hyperthyroidism, which symptom is more likely to predominate?
CorrectIncorrectFocus on symptoms that are more common in older patients with hyperthyroidism.
- 76. Question
Category: Board Review Endocrinology
What is the best initial test to order for a patient in whom you suspect hyperthyroidism?
CorrectIncorrectThink about the most sensitive test for detecting primary hyperthyroidism.
- 77. Question
Category: Board Review Endocrinology
A patient with suspected hyperthyroidism has a low TSH and high free T4, but normal T3 concentrations. This pattern is known as:
CorrectIncorrectFocus on the pattern of thyroid hormone levels in the patient.
- 78. Question
Category: Board Review Endocrinology
A 48-year-old woman is admitted to the ICU with severe pneumonia. She has a history of hypertension and anxiety. Upon reviewing her laboratory results, you notice her TSH level is less than 0.01 mU/L, and her serum total T4 and T3 concentrations are within the normal range. What is the most appropriate next step in her management?
CorrectIncorrectConsider the effects of nonthyroidal illness on thyroid function tests in critically ill patients.
- 79. Question
Category: Board Review Endocrinology
A 35-year-old man presents with symptoms suggestive of hyperthyroidism. Laboratory results show elevated serum total T4 and T3 concentrations and a normal TSH concentration. What is the most likely cause of this patient's euthyroid hyperthyroxinemia?
CorrectIncorrectConsider the role of thyroid hormone-binding proteins in thyroid function tests.
- 80. Question
Category: Board Review Endocrinology
Which of the following factors can cause interference with thyroid test assays using biotin-streptavidin affinity systems?
CorrectIncorrectConsider the impact of dietary supplements on thyroid test assays.
- 81. Question
Category: Board Review Endocrinology
A pregnant woman presents with symptoms of hyperthyroidism. Radioactive iodine uptake is contraindicated in her case. What is the most appropriate diagnostic test to determine the etiology of her hyperthyroidism?
CorrectIncorrect - 82. Question
Category: Board Review Endocrinology
A 32-year-old woman presents with palpitations, weight loss, and tremors. Physical examination reveals a nodular thyroid. Which of the following tests should be performed initially to determine the etiology of her hyperthyroidism?
CorrectIncorrectConsider the patient's pregnancy status and the presence of nodular thyroid disease.
- 83. Question
Category: Board Review Endocrinology
A pregnant woman presents with hyperthyroidism and no nodular goiter. Which test should be performed initially to determine the etiology of her hyperthyroidism?
CorrectIncorrectConsider the patient's pregnancy status and the absence of nodular goiter.
- 84. Question
Category: Board Review Endocrinology
Hyperthyroidism with a high (or normal) radioiodine uptake indicates:
CorrectIncorrectConsider the relationship between radioiodine uptake and the synthesis of thyroid hormone.
- 85. Question
Category: Board Review Endocrinology
Hyperthyroidism with a low (nearly absent) radioiodine uptake indicates:
CorrectIncorrectConsider the relationship between radioiodine uptake and inflammation or extrathyroidal sources of thyroid hormone.
- 86. Question
Category: Board Review Endocrinology
Which of the following measurements can help differentiate Graves' hyperthyroidism from destruction-induced hyperthyroidism when a radioiodine uptake is contraindicated?
CorrectIncorrectConsider the serum T3/T4 ratio and the serum free T3/free T4 ratio as potential measurements to differentiate between Graves' hyperthyroidism and destruction-induced hyperthyroidism.
- 87. Question
Category: Board Review Endocrinology
What is the most common cause of hyperthyroidism?
CorrectIncorrectConsider the autoimmune disorder that results from thyroid-stimulating hormone (TSH)-receptor antibodies.
- 88. Question
Category: Board Review Endocrinology
What condition can cause hyperthyroidism in women with a hydatidiform mole or choriocarcinoma, or in men with testicular germ cell tumors?
CorrectIncorrectLook for the condition that involves high levels of isoforms of human chorionic gonadotropin (hCG) with more thyrotropic activity.
- 89. Question
Category: Board Review Endocrinology
Which of the following medications has been implicated in the onset of Graves' disease?
CorrectIncorrectConsider a medication often used in the treatment of bipolar disorder.
- 90. Question
Category: Board Review Endocrinology
Which rare form of hyperthyroidism results from an activating mutation in the TSH receptor?
CorrectIncorrectThink about a form of hyperthyroidism that is transmitted as an autosomal dominant trait.
- 91. Question
Category: Board Review Endocrinology
Which medication can cause hyperthyroidism with an elevated radioiodine uptake in patients with pulmonary arterial hypertension?
CorrectIncorrectConsider a medication that is a form of prostaglandin I2.
- 92. Question
Category: Board Review Endocrinology
A 35-year-old female presents with palpitations, weight loss, and anxiety. Her radioiodine uptake test shows a normal to high uptake. What is the most likely cause of her hyperthyroidism?
CorrectIncorrectConsider the most common cause of hyperthyroidism with a normal to high radioiodine uptake.
- 93. Question
Category: Board Review Endocrinology
A 29-year-old woman presents with a painful, tender goiter and fever. Her radioiodine uptake test shows a near-absent uptake. What is the most likely diagnosis?
CorrectIncorrectConsider a diagnosis associated with a painful, tender goiter, fever, and a near-absent radioiodine uptake.
- 94. Question
Category: Board Review Endocrinology
A 45-year-old male with a history of pulmonary arterial hypertension presents with hyperthyroidism and an elevated radioiodine uptake. Which medication is most likely responsible for his hyperthyroidism?
CorrectIncorrectConsider a medication used for pulmonary arterial hypertension associated with hyperthyroidism and an elevated radioiodine uptake.
- 95. Question
Category: Board Review Endocrinology
A 32-year-old female presents with hyperthyroidism and a near-absent radioiodine uptake three months after giving birth. What is the most likely diagnosis?
CorrectIncorrectConsider a diagnosis related to the postpartum period and a near-absent radioiodine uptake.
- 96. Question
Category: Board Review Endocrinology
A newborn infant is found to have symptoms of hyperthyroidism, elevated free thyroxine (T4), total triiodothyronine (T3), and low thyroid-stimulating hormone (TSH). What is the most likely diagnosis?
CorrectIncorrectThis condition is related to maternal thyroid disease.
- 97. Question
Category: Board Review Endocrinology
Which of the following is a risk factor for neonatal Graves disease?
CorrectIncorrectThis risk factor is related to the transplacental passage of certain antibodies.
- 98. Question
Category: Board Review Endocrinology
What is the typical timing of symptom onset for neonatal Graves disease in infants born to mothers taking an antithyroid drug?
CorrectIncorrectConsider when the antithyroid drug is metabolized and excreted in the infant.
- 99. Question
Category: Board Review Endocrinology
Which of the following clinical manifestations is unique to neonatal Graves disease?
CorrectIncorrectThis manifestation is related to the appearance of the infant's head and face.
- 100. Question
Category: Board Review Endocrinology
What is a possible reason for an infant to come to medical attention after birth in the context of neonatal Graves disease?
CorrectIncorrectThis situation can happen when the mother has not been previously diagnosed or her diagnosis was not known during labor and delivery.
- 101. Question
Category: Board Review Endocrinology
Which thyroid function tests should be performed in an infant suspected of having neonatal Graves disease?
CorrectIncorrectThese tests help confirm the diagnosis of neonatal Graves disease and can be used as a baseline when monitoring treatment.
- 102. Question
Category: Board Review Endocrinology
What is the preferred first-line treatment for neonatal Graves disease?
CorrectIncorrectThis combination helps control hyperthyroidism and its associated symptoms.
- 103. Question
Category: Board Review Endocrinology
What is a rare cause of neonatal hyperthyroidism not associated with maternal Graves disease?
CorrectIncorrectThis condition is inherited as an autosomal dominant trait and may have a family history of hyperthyroidism.
- 104. Question
Category: Board Review Endocrinology
What is the typical duration of neonatal Graves hyperthyroidism?
CorrectIncorrectAlthough it can persist for six months or even longer, most cases resolve within this timeframe.
- 105. Question
Category: Board Review Endocrinology
What is the therapeutic approach for Graves' hyperthyroidism?
CorrectIncorrectBeta blockers should be started in most patients as soon as the diagnosis of hyperthyroidism is made.
- 106. Question
Category: Board Review Endocrinology
What is the preferred beta blocker in the treatment of Graves' hyperthyroidism?
CorrectIncorrectAtenolol has the advantages of single daily dosing and beta-1 selectivity.
- 107. Question
Category: Board Review Endocrinology
What are the three treatment options for Graves' disease?
CorrectIncorrectAntithyroid drugs (thionamides), radioiodine, or surgery are the three treatment options for Graves' disease.
- 108. Question
Category: Board Review Endocrinology
Which treatment option is contraindicated during pregnancy and lactation?
CorrectIncorrectRadioiodine is contraindicated during pregnancy and lactation.
- 109. Question
Category: Board Review Endocrinology
Which treatment option may be preferred in older adult patients with contraindications to surgery and radioiodine or in patients who want to avoid definitive therapy?
CorrectIncorrectAntithyroid drugs may be preferred in patients who want to avoid definitive therapy.
- 110. Question
Category: Board Review Endocrinology
What is the primary drug used to treat Graves' hyperthyroidism?
CorrectIncorrectMethimazole is almost exclusively used because of its longer duration of action, allowing for once-daily dosing, more rapid efficacy, and lower incidence of side effects.
- 111. Question
Category: Board Review Endocrinology
Which antithyroid drug is preferred during the first trimester of pregnancy?
CorrectIncorrectPropylthiouracil (PTU) is preferred during the first trimester of pregnancy, and in patients who have minor drug reactions to methimazole who refuse radioiodine or surgery.
- 112. Question
Category: Board Review Endocrinology
What baseline blood tests are obtained prior to initiating thionamides?
CorrectIncorrectPrior to initiating thionamides, we obtain baseline blood tests, including a complete blood count (white count with differential) and a liver profile (bilirubin and transaminases).
- 113. Question
Category: Board Review Endocrinology
What is the starting dose of methimazole for patients with small goiters and mild hyperthyroidism?
CorrectIncorrectThe starting dose of methimazole varies according to the severity of the hyperthyroidism. Patients with small goiters and mild hyperthyroidism can be started on 5 to 10 mg once daily.
- 114. Question
Category: Board Review Endocrinology
What is the prevalence of permanent remission after cessation of antithyroid drug therapy?
CorrectIncorrect - 115. Question
Category: Board Review Endocrinology
What is the primary indication for surgery in patients with Graves' hyperthyroidism?
CorrectIncorrect - 116. Question
Category: Board Review Endocrinology
Which adjunctive therapy is rarely used in patients with severe hyperthyroidism or are allergic to thionamides?
CorrectIncorrect - 117. Question
Category: Board Review Endocrinology
Which medication may be useful adjunctive therapy in selected patients who require rapid amelioration of hyperthyroid symptoms?
CorrectIncorrect - 118. Question
Category: Board Review Endocrinology
What medication is preferred during the first trimester of pregnancy for the treatment of hyperthyroidism?
CorrectIncorrect - 119. Question
Category: Board Review Endocrinology
What is the recommended daily intake of elemental calcium for patients with Graves' hyperthyroidism?
CorrectIncorrect - 120. Question
Category: Board Review Endocrinology
What is the initial monitoring recommended for patients receiving treatment for hyperthyroidism?A:) Periodic clinical assessment and measurements of serum free T4 and often total T3 levels.B:) Regular monitoring of serum TSH concentrations.C:) Monthly thyroid function tests for the first six months.D:) None of the above.:Correct: A:MsgCorrect: Initial monitoring of patients receiving treatment for hyperthyroidism should consist of periodic clinical assessment and measurements of serum free T4 and often total T3 levels.:MsgIncorrect: Incorrect. Initial monitoring of patients receiving treatment for hyperthyroidism should consist of periodic clinical assessment and measurements of serum free T4 and often total T3 levels.:hint: none
CorrectIncorrect - 121. Question
Category: Board Review Endocrinology
How often should patients on maintenance thionamide therapy have their thyroid function assessed?A:) At four- to six-week intervals until stabilized, then at three- to six-month intervals.B:) Monthly.C:) Every six months.D:) Annually.:Correct: A:MsgCorrect: Patients on maintenance thionamide therapy should have their thyroid function assessed at four- to six-week intervals until stabilized, then at three- to six-month intervals.:MsgIncorrect: Incorrect. Patients on maintenance thionamide therapy should have their thyroid function assessed at four- to six-week intervals until stabilized, then at three- to six-month intervals.:hint: none
CorrectIncorrect - 122. Question
Category: Board Review Endocrinology
What should be done if patients on thionamide therapy have persistently low serum TSH concentrations after more than six months of therapy?A:) Patients are unlikely to have a remission when the drug is stopped.B:) They should be advised about the likelihood of weight gain.C:) Patients should have their thyroid function assessed monthly.D:) None of the above.:Correct: A:MsgCorrect: If patients on thionamide therapy have persistently low serum TSH concentrations after more than six months of therapy, they are unlikely to have a remission when the drug is stopped.:MsgIncorrect: Incorrect. If patients on thionamide therapy have persistently low serum TSH concentrations after more than six months of therapy, they are unlikely to have a remission when the drug is stopped.:hint: none
CorrectIncorrect - 123. Question
Category: Board Review Endocrinology
What thyroid function tests should be performed on patients treated with radioiodine?A:) Free T4, total T3, and TSH four to six weeks after treatment, and then free T4 and TSH at four- to six-week intervals for up to six months.B:) Free T4 and TSH only.C:) Total T3 and TSH only.D:) None of the above.:Correct: A:MsgCorrect: For patients treated with radioiodine, free T4, total T3, and TSH should be measured four to six weeks after treatment, and then free T4 and TSH (and total T3 if still hyperthyroid) should be measured at four- to six-week intervals for up to six months.:MsgIncorrect: Incorrect. For patients treated with radioiodine, free T4, total T3, and TSH should be measured four to six weeks after treatment, and then free T4 and TSH (and total T3 if still hyperthyroid) should be measured at four- to six-week intervals for up to six months.:hint: none
CorrectIncorrect