Endocrinology Board Review (Block 1 of 4)
Endocrinology Board Review (Block 1 of 4)
Quiz Summary
0 of 53 Questions completed
Questions:
Information
You have already completed this quiz. You cannot start it again.
Quiz is loading…
You must sign in or sign up to take this quiz.
You must first complete the following:
Results
Quiz complete. Results are being recorded.
Results
0 of 53 Questions answered correctly
Your Time:
Time has elapsed.
You have reached 0 of 0 point(s), (0)
Earned Point(s): 0 of 0, (0)
0 Essay(s) Pending (Possible Point(s): 0)
| Average Score | |
| Your Score |
Categories
- Not categorized 0%
- 1
- 2
- 3
- 4
- 5
- 6
- 7
- 8
- 9
- 10
- 11
- 12
- 13
- 14
- 15
- 16
- 17
- 18
- 19
- 20
- 21
- 22
- 23
- 24
- 25
- 26
- 27
- 28
- 29
- 30
- 31
- 32
- 33
- 34
- 35
- 36
- 37
- 38
- 39
- 40
- 41
- 42
- 43
- 44
- 45
- 46
- 47
- 48
- 49
- 50
- 51
- 52
- 53
- Current
- Review
- Answered
- Correct
- Incorrect
- 1. Question
Which of the following statements concerning the surgical management of prolactinomas is incorrect?
CorrectIncorrect - 2. Question
A 52-year-old postmenopausal woman presents with a 12-month history of distressing vasomotor symptoms. She has a history of total abdominal hysterectomy. Your patient has completed a recent google search regarding the risks and benefits of menopausal hormone therapy. Which of the following statements made by the patient is accurate?
CorrectIncorrect - 3. Question
A 23-year-old obese woman with polycystic ovary syndrome is referred to the reproductive endocrinology clinic. She is being scheduled for an assisted reproductive procedure. The patient requests metformin be added to her treatment regimen. Which of these statements is true regarding the role of metformin in anovulatory infertility.
CorrectIncorrect - 4. Question
A 34-year-old woman with oligomenorrhea is diagnosed with polycystic ovary syndrome. She is prescribed spironolactone and oral contraceptives due to severe acne and hirsutism. Which of these effects can be attributed to the mechanism of action of spironolactone?
CorrectIncorrect - 5. Question
How do oral contraceptive pills exert their clinical effects on polycystic ovary syndrome?
CorrectIncorrect - 6. Question
What is the physiologic effect of fibroblast growth factor 23 (FGF-23)?
CorrectIncorrect - 7. Question
Which of the following is not an indication for bisphosphonate therapy in Paget’s disease of Bone(PDB)?
CorrectIncorrect - 8. Question
A 32-year-old man with postoperative hypoparathyroidism reports for his annual check-up. His serum calcium is 6.2 (8.5-10.5 mg/dL. He is symptomatic of hypocalcemia (acral paraesthesias and muscle cramps). He endorses compliance with calcitriol 2mcg daily and calcium 6000mg daily. His 24hour urine calcium is elevated at 623mg/24hrs (normal reference <325mg per 24hours). 25-OH vitamin D is 43 (30-80). You elect to start him on recombinant human parathyroid hormone rhPTH(1-84). How is this form of exogenous parathyroid hormone different from PTH(1-34), the form utilized in the treatment of osteoporosis.
CorrectIncorrect - 9. Question
A 56-year-old man with postoperative hypoparathyroidism reports for his annual check-up. His serum calcium is 8.7 (8.5-10.5 mg/dL. He is completely asymptomatic of hypocalcemia and endorses compliance with calcitriol 0.5mcg daily and calcium 2000mg daily. His 24hour urine calcium is elevated at 623mg/24hrs (normal reference <325mg per 24hours). What is the next best step in the management of this patient
CorrectIncorrect - 10. Question
Which of the following statements regarding the physiologic role of parathyroid hormone is inaccurate?
CorrectIncorrect - 11. Question
Which of the following screening tests is the most sensitive for diagnosing a pheochromocytoma?
CorrectIncorrect - 12. Question
You perform a 1mg overnight dexamethasone suppression test in a patient with a 1cm right adrenal incidentaloma. Which of these statements regarding the interpretation of the test is NOT true?
CorrectIncorrect - 13. Question
A 55-year-old female is diagnosed with a 2cm right adrenal incidentaloma. The lesion has a low attenuation value on non-contrast CT consistent with a benign adenoma. She has no significant past medical history. Screening tests of hormonal hypersecretion returned reassuringly normal. Which of the following scenarios is not an indication for referral to surgery?
CorrectIncorrect - 14. Question
A 45-year-old female is diagnosed with a 3.5cm left adrenal incidentaloma. The lesion has a low attenuation value on non-contrast CT consistent with a benign adenoma. She has no significant past medical history. Her blood pressure is 116/62mmHg. Her serum potassium is 4.0. What is the next best step in the management of this patient?
CorrectIncorrect - 15. Question
Which of these patient scenarios during an evaluation for primary hyperaldosteronism can justifiably proceed directly to anatomical localization studies without confirmatory testing?
CorrectIncorrect - 16. Question
A 36-year-old woman with a history of difficult-to-treat hypertension is referred to the endocrinology clinic for further evaluation. Her current medications include amlodipine, metoprolol, lisinopril, and chlorthalidone. She has a BMI of 40 kg/m2 and has a supraclavicular fat pad. Her blood pressure is 154/88mmHg. Her basic metabolic panel is normal. You proceed to screen for primary hyperaldosteronism. Plasma aldosterone is 22 ng/dL with a plasma renin activity of 0.1 ng/mL/hour. Her estimated aldosterone to renin ratio is 220 ng/dL per ng/(mL x hour). A review of prior abdominal CT scans is significant for a 1.5cm right adrenal incidentaloma from three years earlier. She undergoes confirmatory testing with an oral salt challenge. Aldosterone failed to suppress appropriately. The patient opts for operative intervention, and you suggest she proceeds with adrenal vein sampling (AVS). Her AVS report is shown below.
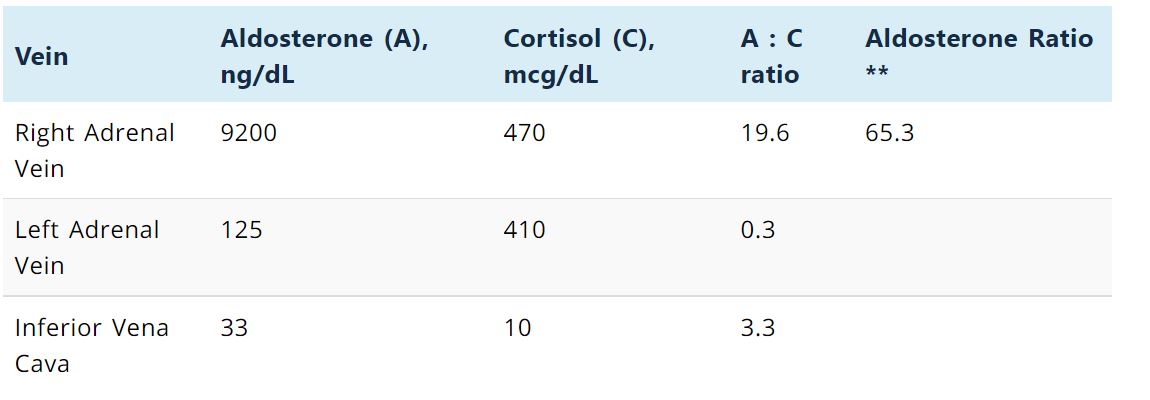
What is the next best step in the management of this patient?
CorrectIncorrect - 17. Question
A 36-year-old woman with a history of difficult-to-treat hypertension is referred to the endocrinology clinic for further evaluation. Her current medications include amlodipine, metoprolol, lisinopril, and chlorthalidone. She has a BMI of 40 kg/m2 and has a supraclavicular fat pad. Her blood pressure is 154/88mmHg. Her basic metabolic panel is normal. You proceed to screen for primary hyperaldosteronism. Plasma aldosterone is 22 ng/dL with a plasma renin activity of 0.1 ng/mL/hour. Her estimated aldosterone to renin ratio is 220 ng/dL per ng/(mL x hour). A review of prior abdominal CT scans is significant for a 1.5cm right adrenal incidentaloma from three years earlier. What is the next best step in the evaluation of this patient?
CorrectIncorrect - 18. Question
A 43-year-old man presents with an 8-month history of fatigue, lack of libido, and increasing central belly fat. He has a remote history of brain radiotherapy 15 years earlier. Physical examination was significant for truncated eyebrows, dry, doughy skin, and delayed relaxation phase of his deep tendon reflexes at the ankles. Serum testosterone (measured at 9 am, fasting) was 50 ng/dL (250-800 ng/dL), low LH, low FSH, TSH of 1.2 (reference range 0.5—4.1 mIU/L), normal prolactin and low IGF-1 (age and gender-matched). You performed a random cortrosyn stimulation test after his early morning cortisol returned borderline low. His post-stimulation cortisol level was, however, appropriate after 30 minutes. What is the next best step in the evaluation of this patient?
CorrectIncorrect - 19. Question
A 26-year-old female with Graves disease, well-controlled on thionamide therapy. Which of the following is not a good predictor of long-term remission after a drug holiday?
CorrectIncorrect - 20. Question
Which of the following results of a fine-needle biopsy of a thyroid nodule is not an indication for mutational analysis (multigene expression classifier)?
CorrectIncorrect - 21. Question
Which of the following thyroid function tests is usually monitored during the treatment of patients with central hypothyroidism?
CorrectIncorrect - 22. Question
A patient presents with recent onset fatigue and general malaise. She is noted to have a normal TSH, low free T3 and a low free T4. Her reverse T3 level is high. What is her most likely diagnosis?
CorrectIncorrect - 23. Question
A 47-year-old woman with a history of celiac disease and post-traumatic stress disorder presents with a six-month history of persistent hyperthyroidism of unclear etiology. She has a small and non-tender thyroid gland on physical examination. Which of the following investigations will be most helpful in distinguishing subacute lymphocytic (painless) thyroiditis from factitious consumption of thyroid hormone by the patient?
CorrectIncorrect - 24. Question
A 23-year-old female with celiac disease presents with a 10-pound unintentional weight loss over four weeks, palpitations, and diarrhea. She reports anterior neck pain. She is noted to have anterior neck pain on the physical exam. An I-123 radioactive iodine scan was low. ESR was elevated at 120mm/hr. Her TSH was suppressed at <0.01 (reference range 0.5—4.1 mIU/L) with a free T4 of 3.7 (reference range 0.7-1.5 ng/dL) and free T3 of 12.4 (reference range 2.0-4.1 ng/dL. Which of the following regarding the patient’s prognosis is accurate?
CorrectIncorrect - 25. Question
Which of the following tests is the most appropriate for distinguishing between endogenous thyroid hormone production and exogenous thyroid ingestion?
CorrectIncorrect - 26. Question
A 54-year-old woman with hypertension, atrial fibrillation, coronary artery disease (status post two coronary stent placements), diabetes mellitus, and a recent distal radial fracture presents to your office on account of elevated serum TSH in the setting of elevated free T4 and free T3. A pituitary MRI was normal with an elevated serum alpha subunit of pituitary glycoprotein. What is the best next step in the evaluation of this patient?
CorrectIncorrect - 27. Question
A 62-year-old woman presented with diaphoresis, palpitations, and persistent diarrhea. Physical examination was significant for a pulse rate of 132bpm, lid retraction, and diffuse goiter. Her TSH was suppressed at 0.3 (reference range 0.5—4.1 mIU/L) with a free T4 of 3.7 (reference range 0.7-1.5 ng/dL) and free T3 of 8(reference range 2.0-4.1 ng/dL). She underwent total thyroidectomy and was started on levothyroxine replacement therapy. The patient had persistent TSH elevation despite progressively increasing doses of levothyroxine after surgery. A TRH stimulation test resulted in a high post-stimulation TSH level. What is the most likely diagnosis of this patient?
CorrectIncorrect - 28. Question
A 38-year-old man with a history of Graves disease underwent total thyroidectomy and was started on levothyroxine replacement therapy. The patient had persistent TSH elevation despite progressively increasing doses of levothyroxine. His TSH was elevated at 8.9 (reference range 0.5—4.1 mIU/L). A T3 loading test failed to suppress serum TSH. Serum CTX (a marker of bone resorption that increases with osteoclastic activity) and serum alpha subunit of pituitary glycoprotein were both elevated above the upper limit of normal.
What is his diagnosis?
CorrectIncorrect - 29. Question
Which of the following is not a glycemic effect of growth hormone?
CorrectIncorrect - 30. Question
A 35-year-old female presented with polyuria and polydipsia three months after an uneventful pregnancy and was diagnosed with central diabetes insipidus. Her pituitary MRI was significant for pituitary stalk thickening. Fluid losses resolved after initiation of Desmopressin (DDAVP) by her treating endocrinologist.
What is the most likely diagnosis?
CorrectIncorrect - 31. Question
A 32-year-old female with a 6-month history of amenorrhea is noted to have a diagnostic Cushingoid body habitus during her physical examination. Her urine pregnancy test is negative. A 1 mg overnight dexamethasone suppression test is significant for a post-suppression cortisol level of 4 mcg/dL. 24-hour urinary free cortisol and late-night salivary cortisol levels were 2 and 3 times above the upper limit of normal, respectively. Plasma ACTH is elevated at baseline. A dedicated pituitary MRI showed a 3mm sellar lesion. What is the best next step in the evaluation of this patient?
CorrectIncorrect - 32. Question
A 46-year-old man presented with an 8-year history of poor libido and a 1-year history of migraine headaches with visual symptoms. He also reported increased fatigue and profuse sweating. A “photograph biopsy” was significant for a marked change in his facial features over the past ten years. Physical examination was significant for increased interdental distance. He had significant acanthosis nigricans and multiple acrochordons involving flexural areas. Visual field testing suggested bitemporal hemianopsia. A contrast-enhanced T1 weighted MRI showed a pituitary adenoma measuring 2x3x2.5cm with suprasellar extension and chiasmal optic impingement.
Serum IGF-1 1256 ng/mL (Upper limit of normal for age and gender being <315 ng/Ml). A mid-morning random growth hormone level of 45 ng/mL (normal <4 ng/mL. A 75gram oral glucose tolerance test was significant for GH levels of 35, 28.9, 23.4, 22.1, and 20.7 ng/mL at baseline, 30,60,90, and 120 minutes, respectively. His other pituitary hormonal axes were intact during preoperative workup. He subsequently underwent transsphenoidal surgery. The pathology report reported a cytokeratin staining pattern in round perinuclear structures (fibrous bodies) consistent with a sparsely granulated somatotroph adenoma.
A 75-gram oral glucose tolerance test was repeated a week after surgery. Post suppression growth hormone levels were 2.1, 1.1, 1, 0.9, 0.8 and 0.9 at baseline, 30, 60, 90 and 120 minutes respectively. The detection limit of the growth hormone assay for this laboratory is 0.01 ng/mL.
Which of the following statements is true
CorrectIncorrect - 33. Question
A 46-year-old Caucasian woman presents with a six-month history of progressive weight gain. Her physical examination is significant for moderate hirsutism, facial plethora, and multiple violaceous striae involving the abdomen. She is also noted to have significant hyperpigmentation of her palmar creases. A 1mg overnight dexamethasone suppression test was significant for a post suppression cortisol level of 8 mcg/dL. Pituitary MRI showed a 1.6 cm adenoma on the right side of the pituitary gland. Inferior petrosal sinus sampling (IPSS) confirmed the diagnosis of an ACTH-dependent cause of hypercortisolemia originating from the pituitary gland. The patient underwent an unsuccessful transsphenoidal surgery and subsequently required medical therapy (mifepristone) to control her symptoms.
She reports to your clinic with new-onset fatigue, nausea, and colicky abdominal pain. She is hypotensive, and further workup reveals a random serum cortisol level of 43 (5-15 mcg/dL). What is the likely cause of her presentation?
CorrectIncorrect - 34. Question
Which of the following pairings of medications utilized in Cushing’s syndrome and their primary site of action is inaccurate.
CorrectIncorrect - 35. Question
A 23-year-old Caucasian woman presents with a six-month history of progressive weight gain and amenorrhea. Her physical examination is significant for moderate hirsutism, facial plethora, and multiple violaceous striae involving the abdomen. She is noted to have significant hyperpigmentation of her palmar creases. A 1mg overnight dexamethasone suppression test was significant for a post suppression cortisol level of 3 mcg/dL. Pituitary MRI showed a 1.2 cm adenoma on the right side of the pituitary gland. Inferior petrosal sinus sampling (IPSS) confirmed the diagnosis of an ACTH-dependent cause of hypercortisolemia originating from the pituitary gland. The patient underwent an unsuccessful transsphenoidal surgery and subsequently required medical therapy (ketoconazole) to control her hypercortisolemia.
She reports to your clinic with new-onset headaches and muscle weakness. Her workup reveals severe hypertension and hypokalemia. A further increase in the dose of ketoconazole results in worsening hypertension and hypokalemia. What is the likely cause of her presentation?
CorrectIncorrect - 36. Question
Which of the following statements regarding the use of dopaminergic agonists (DAs) in the management of Cushing’s disease is inaccurate?
CorrectIncorrect - 37. Question
Pasireotide, a somatostatin receptor analog, has demonstrable efficacy in the Treatment of Cushing’s syndrome. Which receptor subtype modulates this function of pasireotide?
CorrectIncorrect - 38. Question
Which of the following is a cause of a false positive dexamethasone suppression test conducted on account of clinical suspicion for Cushing’s syndrome?
CorrectIncorrect - 39. Question
A 64-year-old, otherwise healthy woman presents with a 3-week history of progressive weight gain. Her physical examination is significant for a BMI of 38 kg/m2, blood pressure of 198/102mmHg, and severe hirsutism. She has a low baseline ACTH. A 1mg overnight dexamethasone suppression test was significant for a post suppression cortisol level of 5.2 mcg/dL. What is the most likely diagnosis?
CorrectIncorrect - 40. Question
A 52-year-old woman presents with a 2-year history of progressive weight gain. Her physical examination for a BMI of 38 kg/m2 and a supraclavicular fat pad. She has a low baseline DHEA sulfate and ACTH. A 1mg overnight dexamethasone suppression test was significant for a post suppression cortisol level of 5.2 mcg/dL. What is the most likely diagnosis?
CorrectIncorrect - 41. Question
A 23-year-old Caucasian woman presents with a six-month history of progressive weight gain and amenorrhea. Her physical examination is significant for moderate hirsutism, facial plethora, and multiple violaceous striae involving the abdomen. She is noted to have significant hyperpigmentation of her palmar creases. A 1mg overnight dexamethasone suppression test was significant for a post suppression cortisol level of 3 mcg/dL. What is the most likely diagnosis?
CorrectIncorrect - 42. Question
A 23-year-old Caucasian woman presents with a six-month history of progressive weight gain and amenorrhea. Her physical examination is significant for moderate hirsutism, facial plethora, and multiple violaceous striae involving the abdomen. She is noted to have significant hyperpigmentation of her palmar creases. A 1mg overnight dexamethasone suppression test was significant for a post suppression cortisol level of 7 mcg/dL. Which of the following interpretations of the dexamethasone suppression test in the evaluation of endogenous hypercortisolemia is true?
CorrectIncorrect - 43. Question
Which of the following physical examination signs is not a positive discriminatory for diagnosing Cushings disease with a significant specificity?
CorrectIncorrect - 44. Question
A 45-year-old man presents with a 5-year history of poor libido. He is noted to have significant acral enlargement, prognathism, and bilateral carpal tunnel syndrome. IGF-1 is noted to be elevated up to 2 times the upper limit of normal. You perform an oral glucose tolerance test with 75grams of anhydrous glucose. His nadir serum growth hormone is inappropriately elevated at 2.3 ng/dL after two hours. The patient is diagnosed with a 12mm growth hormone-secreting macroadenoma and undergoes transsphenoidal surgery. He, unfortunately, has progressive persistent disease post-surgery and is started on appropriate medical therapy. The patient, however, develops significant elevation in serum transaminases within a few weeks of treatment. Which of the following medications is associated with this side effect?
CorrectIncorrect - 45. Question
A 69-year-old man presents with a 5-year history of poor libido. He is noted to have significant acral enlargement, prognathism, and bilateral carpal tunnel syndrome. IGF-1 is noted to be elevated up to 2 times the upper limit of normal. You perform an oral glucose tolerance test with 75grams of anhydrous glucose. His nadir serum growth hormone is inappropriately elevated at 2.3 ng/dL after two hours. The patient is diagnosed with a 12mm growth hormone-secreting macroadenoma and undergoes transsphenoidal surgery. He, unfortunately, has progressive persistent disease post-surgery and is started on appropriate medical therapy. The patient, however, develops severe hyperglycemia within a few weeks of treatment. Which of the following medications is the most likely cause?
CorrectIncorrect - 46. Question
Which of the following statements regarding medical therapies for acromegaly and their mechanism of action is inaccurate?
CorrectIncorrect - 47. Question
In patients with acromegaly, which of the following laboratory tests regarding treatment goals is inaccurate?
CorrectIncorrect - 48. Question
A 57-year-old man presents with an 8-year history of poor libido, lack of early tumescence, and intermittent headaches. He is noted to have significant acral enlargement and an increase in interdental distance on physical examination. IGF-1 is noted to be elevated up to 4 times the upper limit of normal. You perform an oral glucose tolerance test with 75grams of anhydrous glucose. His nadir serum growth hormone is inappropriately elevated at 4 ng/dL after two hours. The patient is diagnosed with a 2cm growth hormone-secreting macroadenoma and undergoes transsphenoidal surgery. He, unfortunately, has progressive persistent disease post-surgery. He was deemed a nonresponder to somatostatin analog therapy and is started on pegvisomant. Which of the following laboratory results will be expected?
CorrectIncorrect - 49. Question
A 45-year-old is diagnosed with an invasive macroprolactinoma and is started on medical treatment. He is subsequently diagnosed with compulsive gambling and sexual inappropriateness. What is the most likely cause?
CorrectIncorrect - 50. Question
Which of the following is not a predictor of inadequate response to dopaminergic agonist therapy?
CorrectIncorrect - 51. Question
A 24-year-old woman presents with new-onset galactorrhea and a 3-month history of amenorrhea. Her urine pregnancy screen is negative. Serum prolactin level of 98 ng/mL (4-30 ng/mL), normal serum IGF-1, normal ACTH and 8 AM cortisol, normal free T4. A dedicated pituitary MRI showed a 4 mm adenoma. Which of the following management timelines is incorrect?
CorrectIncorrect - 52. Question
A 62-year-old postmenopausal woman is found to have a 5mm pituitary incidentaloma during a CT scan of the head. She was subsequently diagnosed with a microprolactinoma after her serum prolactin level returned elevated at 126 ng/mL (reference range 4-30 ng/mL). Which of the following is the best next step in managing this patient?
CorrectIncorrect - 53. Question
Which of the following statements concerning the management of prolactinomas in pregnancy is correct?
CorrectIncorrect