Adrenocortical insufficiency, more commonly referred to as Addison’s disease, is a condition that results from the inadequate production of certain hormones by the adrenal glands. This insufficiency can be attributed to damage to these glands or a congenital defect that impairs their function. Adrenal glands can be compromised for several reasons, including infections like tuberculosis, infiltration by malignant cells, or an autoimmune process where the body’s immune system mistakenly attacks the adrenal glands. Tuberculosis-induced adrenal damage remains the most prevalent cause worldwide, despite being considerably rare in countries like the United States today.
Addison’s disease, named after Thomas Addison, who first identified this condition nearly two centuries ago, refers to the acquired form of adrenocortical insufficiency.
Mechanisms Underlying Adrenal Crisis
Adrenal crisis, or Addisonian crisis, is a severe and potentially fatal condition characterized by an acute insufficiency of adrenal gland hormones, primarily cortisol and aldosterone.
Cortisol, classified as a glucocorticoid, profoundly influences multiple physiological processes. It modulates the body’s stress response, regulates metabolic pathways, and mediates anti-inflammatory responses. Aldosterone, a mineralocorticoid, plays an indispensable role in maintaining the body’s electrolyte and fluid balance, thus contributing to blood pressure regulation.
A sudden decrease in cortisol and aldosterone levels typically precipitates an adrenal crisis. The resultant cortisol deficiency compromises the body’s ability to respond appropriately to stress, interferes with metabolic processes, and impairs immunoregulatory mechanisms, specifically those related to inflammation.
Concurrent aldosterone insufficiency disrupts electrolyte homeostasis, leading to hyponatremia and hyperkalemia. This electrolyte imbalance can result in fluid depletion, hypotension, and potentially precipitate shock.
The consequences of an adrenal crisis are particularly severe in situations of increased physiological stress, such as during an injury, severe illness, or surgery, wherein the demand for adrenal hormones escalates. If the adrenal glands are unable to augment hormone production to meet this heightened demand, it can culminate in an adrenal crisis.
Precipitating Factors and Clinical Manifestations of Adrenal Crisis
Various factors can instigate an adrenal crisis, including severe physical stressors (like surgery or significant injury), systemic infections, dehydration, or abrupt discontinuation of glucocorticoid medication without appropriate dose tapering.
Adrenal crisis often presents with acute symptoms, including severe pain in the lower back, abdomen, or legs, profuse vomiting and diarrhea, hypotension, syncope, and severe dehydration. This condition necessitates immediate medical intervention, and the management approach typically involves rapid administration of hydrocortisone, fluids, and electrolytes to restore hormone levels and blood volume swiftly.
When the adrenal glands cease to produce adequate amounts of cortisol and aldosterone, it leads to significant physiological alterations. The fall in blood pressure is one of the immediate effects accompanied by changes in the concentrations of key electrolytes in the blood. The sodium levels tend to drop while potassium levels rise.
Simultaneously, a decrease in circulating cortisol disrupts the negative feedback mechanism on the hypothalamo-pituitary axis, leading to an escalation in Proopiomelanocortin (POMC) synthesis and a subsequent increase in Adrenocorticotropic hormone (ACTH). The rise in ACTH is mirrored by an increase in Melanocyte-stimulating hormone (MSH), a derivative of POMC. Over time, the increased MSH levels trigger hyperpigmentation, manifesting as a distinct tan in individuals suffering from adrenal insufficiency.
Symptoms and Diagnostic Processes
Apart from the drop in blood pressure, inadequate cortisol production can lead to vague symptoms such as persistent fatigue and a sense of exhaustion. Routine tests may show slightly decreased sodium and elevated potassium levels in the blood.
One standard diagnostic method involves drawing blood at 9:00 AM when cortisol levels are expected to be at their peak. A significantly lower cortisol value could signal adrenocortical insufficiency, warranting further evaluation by an endocrinology specialist. It’s crucial to understand that cortisol levels fluctuate throughout the day, and a lower level later in the evening might be considered normal. Shift workers, in particular, might show alterations in this diurnal rhythm.
In suspected cases, a more comprehensive dynamic investigation is recommended. The ACTH stimulation test is a widely accepted diagnostic procedure for assessing Addison’s disease.
The Process of Diagnosing Addison’s Disease
The diagnosis of Addison’s disease involves an initial collection of a blood sample for the measurement of cortisol and Adrenocorticotropic hormone (ACTH) levels. In individuals suffering from Addison’s disease, baseline cortisol levels are usually low, while ACTH levels are elevated.
The subsequent step in the diagnosis involves the administration of an injection containing 250 mcg of synthetic ACTH, also known as Synacthen. Blood samples are then collected at intervals of 30 and 60 minutes post-injection for the evaluation of cortisol levels.
In individuals with Addison’s disease, there is a minimal increase in cortisol levels, despite the large dose of ACTH. In contrast, healthy individuals display a significant surge in cortisol levels, usually increasing to a minimum of 18mcg/dL (Or >15mcg/dL with recent ultrasensitive assays). It’s important to note that these numerical values may exhibit slight variations across different healthcare facilities due to variations in the specific assay techniques employed.
Updated diagnostic tests and protocols can be accessed from our dynamic tests database.
Treatment for Addison’s Disease
Once the diagnosis of Addison’s disease is established, lifelong treatment with specific types of corticosteroids becomes necessary. Typically, hydrocortisone and fludrocortisone are the choice of drugs for replacement therapy, standing in for glucocorticoids and mineralocorticoids, respectively.
Treatment management and dosage adjustments should be handled by specialists in endocrinology to ensure the optimal control of symptoms. It’s crucial for patients to carry a steroid card, informing medical personnel of their condition in case of emergencies or unexpected medical events, signaling the need for additional steroid administration.
Many patients manage their condition with a daily dose of hydrocortisone, usually around 20mg. This dose is typically split into portions throughout the day: 10mg upon waking, 5mg around lunchtime, and a final 5mg dose in the early afternoon. Night-time dosing is not recommended as it can disrupt sleep patterns. The last dose should ideally be administered by 5:00 PM or at the latest, by 6:00 PM for those who wish to maintain normal sleep cycles. In addition to hydrocortisone, patients also require a daily intake of fludrocortisone, generally ranging between 50 and 100 mcg.
Treatment of Adrenal crisis
Individuals with Addison’s disease who are not receiving treatment with hydrocortisone and fludrocortisone, either due to an undiagnosed condition or accidental cessation of their medication, are at risk of a critical condition known as an Addisonian crisis. This life-threatening situation manifests as a salt-depleting, hypotensive crisis. If not promptly diagnosed and treated with steroids, patients may not recover from an Addisonian crisis.
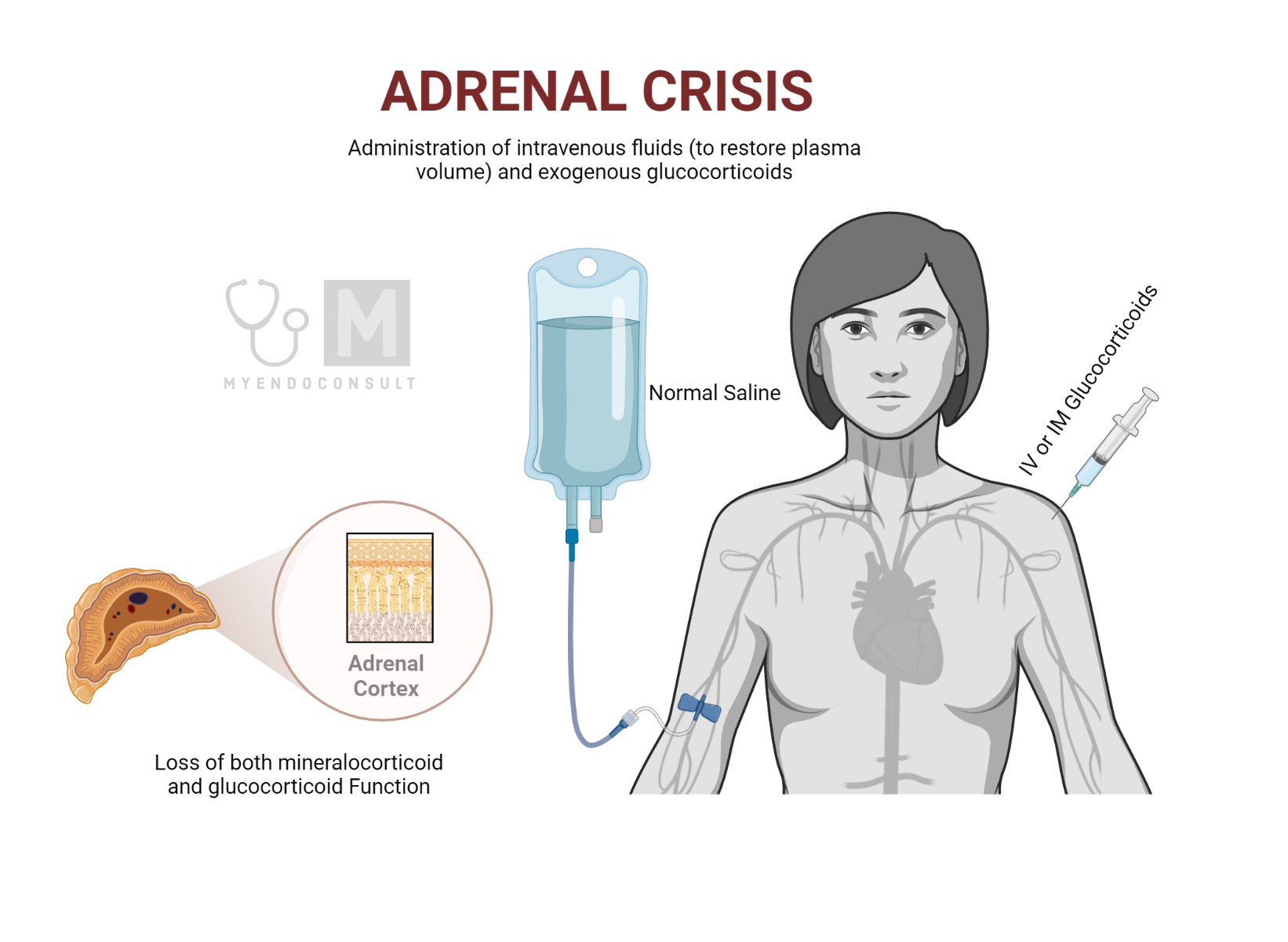
A noticeable feature of this condition includes nausea and vomiting, which can exacerbate the crisis by hindering the ingestion and retention of necessary steroids. This necessitates prompt medical attention and warrants the classification of an Addisonian crisis as a medical emergency.
In such cases, patients need to be rapidly transported to a hospital for immediate parenteral (intravenous or intramuscular) administration of hydrocortisone, typically a dose of 100mg. This prompt action serves to provide both glucocorticoid and enough mineralocorticoid activities crucial to preserving the patient’s life.
These patients are often significantly salt-depleted, a condition stemming from a combination of excessive vomiting and the loss of sodium via the kidneys due to the lack of mineralocorticoids. Thus, they also require rehydration with saline to compensate for this loss.
Once the crisis is managed, and patients’ blood pressure returns to normal, the routine administration of their regular hydrocortisone and fludrocortisone replacement medications can be resumed.
What are steroid alert precautions?
Patients with adrenal insufficiency are at risk of an adrenal crisis, which is a life-threatening condition. Hence, the following steroid alert precautions should be followed:
- Medic Alert Identification: Patients should wear a medical alert bracelet or necklace or carry a card that identifies their condition. This ensures that, in the event of an emergency, healthcare providers are immediately aware of their adrenal insufficiency.
- Always Carry Medication: Patients should always have a supply of their steroid medication on hand. This is particularly important when traveling or going to locations where access to pharmacies may be limited.
- Emergency Injection Kit: Patients should consider carrying an emergency hydrocortisone injection kit, especially for situations where oral medication cannot be taken, or immediate administration of hydrocortisone is required.
- Double Dosing During Illness or Stress: During periods of stress or illness, particularly when fever is present, patients may need to take a “stress dose” or increase their medication under their doctor’s guidance.
- Educate Close Contacts: Family members, friends, and coworkers should be aware of the patient’s condition and what to do in case of an emergency, including how to administer an emergency injection if necessary.
- Regular Medical Check-ups: Regular appointments with an endocrinologist or another healthcare provider are essential for monitoring the disease and adjusting medication if necessary.
- Proper Hydration and Salt Intake: Due to the role of aldosterone in regulating the body’s salt and water balance, patients may need to ensure they are properly hydrated and may need to increase salt intake during periods of intense physical activity or hot weather.
- Avoid Abrupt Discontinuation of Steroids: Sudden stoppage of steroid medication can trigger an adrenal crisis. Always consult with a healthcare provider before making any changes to medication regimens.
- Emergency Care Plan: Having a clear plan of action for emergencies, including knowing when to go to the emergency room, who to contact, and what medications to take, can save crucial time and improve outcomes.
Kindly Let Us Know If This Was helpful? Thank You!


