The nephron is the functional unit of the kidney, responsible for filtering and processing blood to produce urine. Each kidney contains approximately one million nephrons, which are responsible for regulating the body’s fluid and electrolyte balance. The nephron can be divided into four main regions: the renal corpuscle, the proximal tubule, the loop of Henle, and the distal tubule. Let us take a closer look at each of these regions.

Parts of the nephron
Renal Corpuscle: The renal corpuscle is the site of glomerular ultrafiltration, which is the process by which blood is filtered to produce urine. The glomerulus is a tuft of capillaries that is surrounded by the Bowman’s capsule. Blood enters the glomerulus via the afferent arteriole and exits via the efferent arteriole. The pressure gradient created by this trans arteriolar gradient and the specialized structure of the glomerular capillaries allows for the selective filtration of water, ions, and small molecules from the blood into the Bowman’s capsule. This ultrafiltrate of plasma then passes through the proximal tubule.
Proximal Tubule: The proximal tubule is the first segment of the renal tubule and is responsible for reabsorbing most of the filtered substances or load. It is worth noting that the proximal tubule is highly permeable to water and solutes and is lined by microvilli, which increases its reabsorptive surface area substantially. Indeed, the epithelial cells of the proximal tubule actively transport ions, such as sodium, chloride, and potassium, and nutrients, such as glucose and amino acids, from the tubular fluid back into the blood. The proximal tubule is also responsible for secreting various organic anions and cations, such as creatinine and uric acid, into the tubular fluid.
Loop of Henle: The loop of Henle is a U-shaped segment of the renal tubule that extends from the cortex to the medulla. The loop of Henle is divided into three segments: the descending limb, the thin ascending limb, and the thick ascending limb.
The descending limb is permeable to water but impermeable to solutes, resulting in the passive movement of water out of the tubular fluid into the surrounding interstitial fluid. Also, the thin ascending limb is permeable to solutes but impermeable to water, resulting in the passive movement of ions out of the tubular fluid and into the surrounding interstitial fluid. The thick ascending limb is the site of active transport of ions, such as sodium, potassium, and chloride, out of the tubular fluid and into the interstitial fluid. This process creates a high concentration of solutes in the interstitial fluid, which ultimately draws water out of the descending limb and collecting duct and contributes to the formation of concentrated urine.
Distal Tubule: The distal tubule is responsible for fine-tuning the electrolyte and acid-base balance of the body. The distal tubule is lined with specialized cells that actively transport ions, such as sodium, potassium, and hydrogen, from the tubular fluid into the blood or vice versa. The distal tubule is also the site of aldosterone and antidiuretic hormone (ADH) action, both critical hormones which regulate sodium and water balance.
Collecting Duct: The collecting duct is the final site which determines the final concentration and electrolyte composition of urine. The collecting duct is lined with cells that are responsive to ADH, a hormone which regulates water reabsorption.
When ADH levels are high, water is reabsorbed from the collecting duct, leading to the concentration of urine. When ADH levels are low, water is not reabsorbed adequately, leading to the production of dilute urine.
Indeed the final concentration of the urine is determined by a countercurrent multiplier system, which involves the interaction between the loop of Henle and the collecting duct. The high concentration of ions in the interstitial fluid of the medulla created by the loop of Henle allows for the passive movement of water out of the collecting duct and into the interstitial fluid, which further concentrates the urine.
In addition to the four main regions of the nephron, there are also juxtaglomerular cells, which are specialized cells located near the glomerulus that secrete renin. Renin plays a role in the regulation of blood pressure and the renin-angiotensin-aldosterone system.
Vascular supply of the nephron
The vascular supply of the nephron is crucial for the function of the kidney. The blood vessels that supply the nephron include the afferent arteriole, the glomerulus, the efferent arteriole, and the peritubular capillaries. Let’s take a closer look at each of these blood vessels.
Afferent arteriole: The afferent arteriole is a small branch of the renal artery that supplies blood to the glomerulus. The afferent arteriole is responsible for delivering blood to the glomerulus, which is the site of filtration.
Glomerulus: The glomerulus is a dense network of capillaries that is surrounded by the Bowman’s capsule. Blood enters the glomerulus via the afferent arteriole and exits via the efferent arteriole. The glomerulus is the site of filtration, where small molecules, such as water, electrolytes, and waste products, are filtered out of the blood and into the Bowman’s capsule.
Efferent arteriole: The efferent arteriole is a small branch of the renal artery that exits the glomerulus and supplies blood to the peritubular capillaries. The efferent arteriole is important for maintaining the pressure gradient within the glomerulus, which is necessary for filtration.
Peritubular capillaries: The peritubular capillaries are a network of small blood vessels that surround the renal tubule. The peritubular capillaries are responsible for reabsorbing and secreting substances from the tubular fluid. The peritubular capillaries are also responsible for the exchange of oxygen and nutrients between the blood and the renal tubule.
In addition to these blood vessels, there is another important structure in the vascular supply of the nephron called the vasa recta. The vasa recta is a network of capillaries that runs parallel to the loop of Henle. The vasa recta are responsible for maintaining the osmotic gradient in the medulla of the kidney, which is important for the concentration of urine.
The blood supply to the nephron is regulated by the renal autoregulatory mechanism. This mechanism helps to maintain a constant renal blood flow and glomerular filtration rate (GFR) despite changes in blood pressure. The autoregulatory mechanism involves the dilation or constriction of the afferent and efferent arterioles in response to changes in blood pressure, which helps to maintain a constant GFR.
Site of action of diuretics in the nephron
Diuretics are a class of drugs that increase the production of urine by the kidneys, leading to a reduction in fluid volume and sodium levels in the body. They are used to treat a variety of conditions, including hypertension, heart failure, and edema. There are several types of diuretics, each with a different mechanism of action:
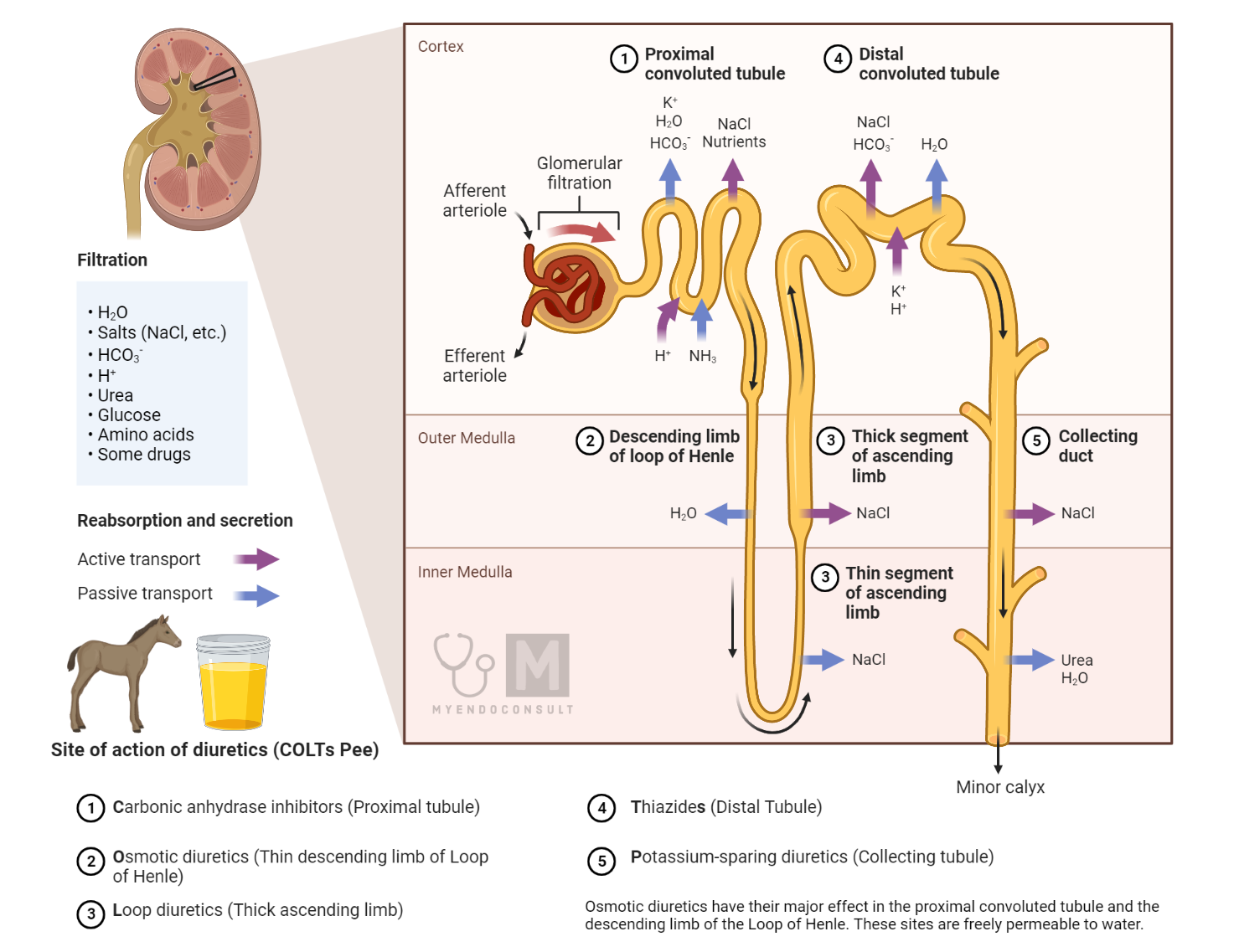
Thiazide Diuretics: Thiazide diuretics, such as hydrochlorothiazide and chlorthalidone, work by inhibiting the sodium-chloride cotransporter in the distal convoluted tubules of the kidneys. This results in the excretion of more sodium and water in the urine, leading to a reduction in fluid volume. Thiazide diuretics are commonly used to treat hypertension and mild to moderate edema.
Loop Diuretics: Loop diuretics, such as furosemide and bumetanide, work by blocking the sodium-potassium-chloride cotransporter in the ascending limb of the loop of Henle in the kidneys. This results in a significant increase in urine output and a rapid reduction in fluid volume. Loop diuretics are often used to treat severe edema, heart failure, and hypertension.
Potassium-Sparing Diuretics: Potassium-sparing diuretics, such as spironolactone and eplerenone, work by blocking the action of aldosterone, a hormone that promotes the reabsorption of sodium and the excretion of potassium in the kidneys. By blocking aldosterone, potassium-sparing diuretics cause an increase in urine output without causing significant loss of potassium. These drugs are often used in combination with other diuretics to treat hypertension and heart failure.
Carbonic Anhydrase Inhibitors: Carbonic anhydrase inhibitors, such as acetazolamide, work by inhibiting the action of the enzyme carbonic anhydrase in the proximal convoluted tubule of the kidneys. This results in a decrease in the reabsorption of bicarbonate ions and an increase in the excretion of bicarbonate and other ions in the urine. Carbonic anhydrase inhibitors are used to treat glaucoma, altitude sickness, and some types of edema.
In summary, diuretics work by different mechanisms to increase urine output and reduce the fluid volume in the body. The choice of diuretic will depend on the underlying condition being treated, the severity of the condition, and any potential side effects or drug interactions.
Frequently Asked Questions
What is the countercurrent multiplier of the kidney?
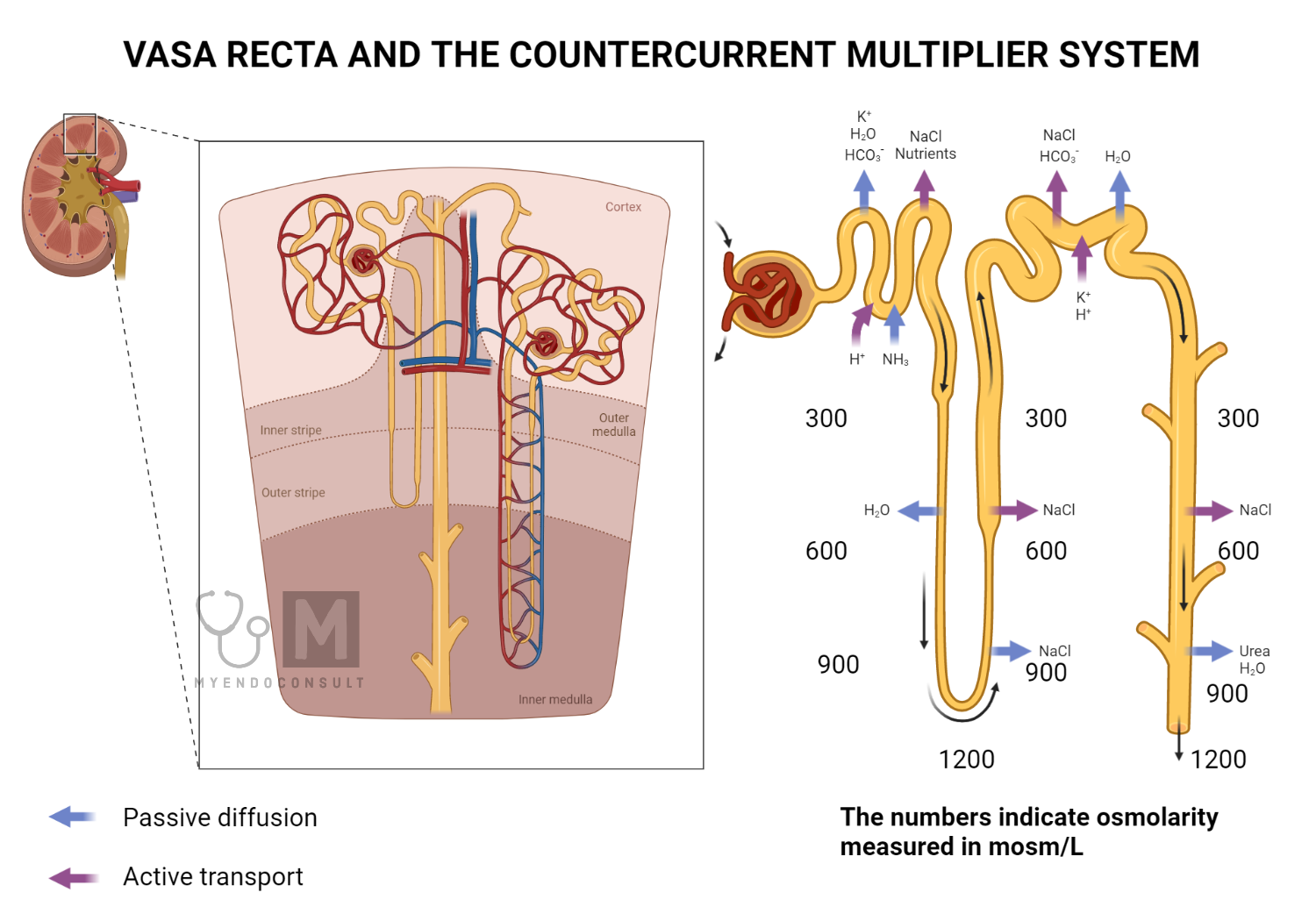
Countercurrent Multiplier: The countercurrent multiplier is a mechanism that involves the loop of Henle and the collecting duct. The loop of Henle is divided into a descending limb and an ascending limb, with the ascending limb further divided into a thin segment and a thick segment. The descending limb is permeable to water but not to solutes, while the ascending limb is permeable to solutes but not to water.
The loop of Henle establishes a concentration gradient in the medulla of the kidney by creating a high concentration of solutes in the interstitial fluid of the renal medulla. The thick ascending limb actively transports ions, such as sodium, chloride, and potassium, from the tubular fluid into the interstitial fluid. This creates a high concentration of solutes in the interstitial fluid, which draws water out of the descending limb and collecting duct, leading to the concentration of urine.
The countercurrent multiplier is called “countercurrent” because the flow of fluid in the ascending and descending limbs of the loop of Henle is in opposite directions. This countercurrent flow is essential for the establishment and maintenance of the concentration gradient in the renal medulla.
What is the vasa recta of the kidney
Vasa Recta: The vasa recta is a network of capillaries that runs parallel to the loop of Henle. The vasa recta plays an essential role in the countercurrent multiplier mechanism (previously mentioned) by providing the blood supply to the renal medulla.
The vasa recta is a countercurrent exchange system, which means that the blood flow in the capillaries is in the opposite direction to the fluid flow in Henle’s loop. This countercurrent flow allows for the exchange of solutes and water between the vasa recta and the interstitial fluid of the renal medulla.
The vasa recta also help to maintain the concentration gradient in the renal medulla by preventing the washout of solutes. As blood flows through the descending vasa recta, it picks up solutes from the interstitial fluid and becomes more concentrated. As blood flows through the ascending vasa recta, it releases solutes into the interstitial fluid, which helps to maintain the high concentration of solutes in the medulla.
In summary, the countercurrent multiplier and the vasa recta are essential mechanisms that play a crucial role in the kidney’s ability to concentrate urine. The countercurrent multiplier involves the loop of Henle and the collecting duct and establishes a concentration gradient in the renal medulla.
The vasa recta is a countercurrent exchange system that provides the blood supply to the renal medulla and helps to maintain the concentration gradient. Together, these mechanisms ensure that the kidney can effectively concentrate urine and maintain the body’s fluid and electrolyte balance.
References
- Preuss HG. Basics of renal anatomy and physiology. Clin Lab Med. 1993 Mar;13(1):1-11. PMID: 8462252.
- Sands JM, Kokko JP. Countercurrent system. Kidney Int. 1990 Oct;38(4):695-9. doi: 10.1038/ki.1990.261. PMID: 2232506.
- Pallone TL, Turner MR, Edwards A, Jamison RL. Countercurrent exchange in the renal medulla. Am J Physiol Regul Integr Comp Physiol. 2003 May;284(5):R1153-75. doi: 10.1152/ajpregu.00657.2002. PMID: 12676741.

