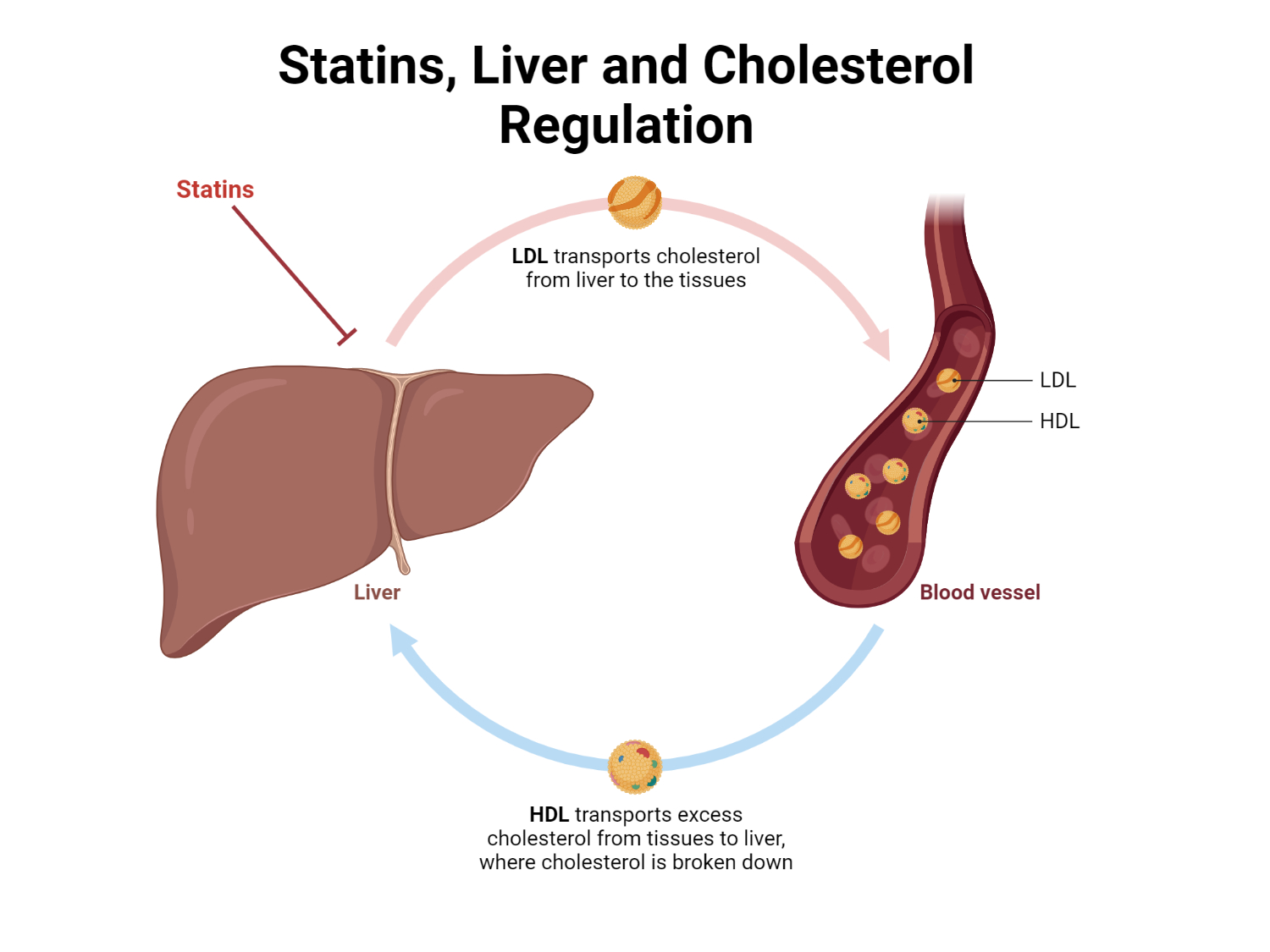
Hydroxymethylglutaryl coenzyme A (HMG-CoA) reductase inhibitors, or statins, are first-line agents in reducing low-density lipoprotein cholesterol (LDL-C). Cholesterol is essential for normal cellular function; however, excess LDL-C leads to atherogenesis, causing coronary artery disease (CAD), heart attack, and stroke. Statin therapy has demonstrated morbidity and mortality benefits by reducing LDL-C levels. Thus, patients must take statins in a manner that maximizes their effectiveness. This article explores the importance of statin timing, focusing on circadian rhythms, half-lives, and patient compliance.
Circadian Rhythm and Cholesterol Production
It was initially hypothesized that human cholesterol production might have a cyclical nature, similar to the pattern observed in animals. Human trials confirmed this fluctuation, with the highest cholesterol production occurring in the liver during fasting. Indeed, this circadian rhythm of cholesterol production prompted the recommendation that statins be dosed at bedtime to provide the highest medication concentration when endogenous cholesterol production is at its peak.
Pharmacokinetic Properties of Individual Statins
Investigations into the pharmacokinetic properties of individual statins revealed that not all agents need to be dosed at bedtime. Although all statins undergo hepatic metabolism, their elimination half-lives vary. Simvastatin, fluvastatin, and lovastatin have shorter elimination half-lives compared to other drugs within the class.
These agents require bedtime dosing to maximize efficacy, allowing the highest statin concentration to be present during peak endogenous cholesterol synthesis. In contrast, the longer half-lives of rosuvastatin, atorvastatin, pitavastatin, and pravastatin enable these agents to maintain a therapeutic drug concentration over 24 hours, allowing for more flexible administration times.
Patient Compliance and Statin Timing
It is worth noting that proper counseling regarding statin timing is crucial for maximizing efficacy. However, some patients may not comply with bedtime dosing recommendations for agents with shorter half-lives, resulting in decreased efficacy. Agents with longer half-lives offer greater flexibility in administration time, potentially improving compliance and ultimately leading to greater LDL-C reduction and the ability to achieve cholesterol goals.
Conclusion
Understanding the circadian rhythm of cholesterol production and the pharmacokinetic properties of individual statins is essential for optimizing statin therapy. While some statins require bedtime dosing due to their short half-lives, others can maintain therapeutic drug concentrations over a 24-hour period, allowing for more flexible administration times. Considering patient compliance is vital, as agents with longer half-lives may improve treatment adherence, resulting in better LDL-C reduction and achievement of cholesterol goals.
Kindly Let Us Know If This Was helpful? Thank You!


