Importance of glucose monitoring in diabetes management
Diabetes is a chronic disease characterized by the body’s inability to regulate blood glucose or sugar, levels. Regular and accurate glucose monitoring is a cornerstone of effective diabetes management. This is primarily because glucose levels can fluctuate significantly throughout the day due to a variety of factors such as food intake, physical activity, stress, illness, and the effects of medication.
The primary aim of diabetes management is to maintain blood glucose levels within a target range, which reduces the risk of both immediate and long-term complications. High glucose levels, or hyperglycemia, over time, can lead to severe complications such as cardiovascular disease, nerve damage, kidney damage, eye damage, and increased risk of stroke. On the other hand, low glucose levels, or hypoglycemia, can lead to symptoms such as shaking, sweating, rapid heartbeat, and even loss of consciousness.
Traditional methods of glucose monitoring require self-monitoring of blood glucose (SMBG) by the patient several times a day using a glucose meter. This typically involves pricking the finger to obtain a blood sample. While this method has been effective for many years, it only provides a snapshot of the glucose level at a particular moment in time. In recent years, technology has evolved to offer continuous glucose monitoring (CGM), which provides a more comprehensive picture of glucose trends throughout the day and night.
Introduction to Time in Range Concept
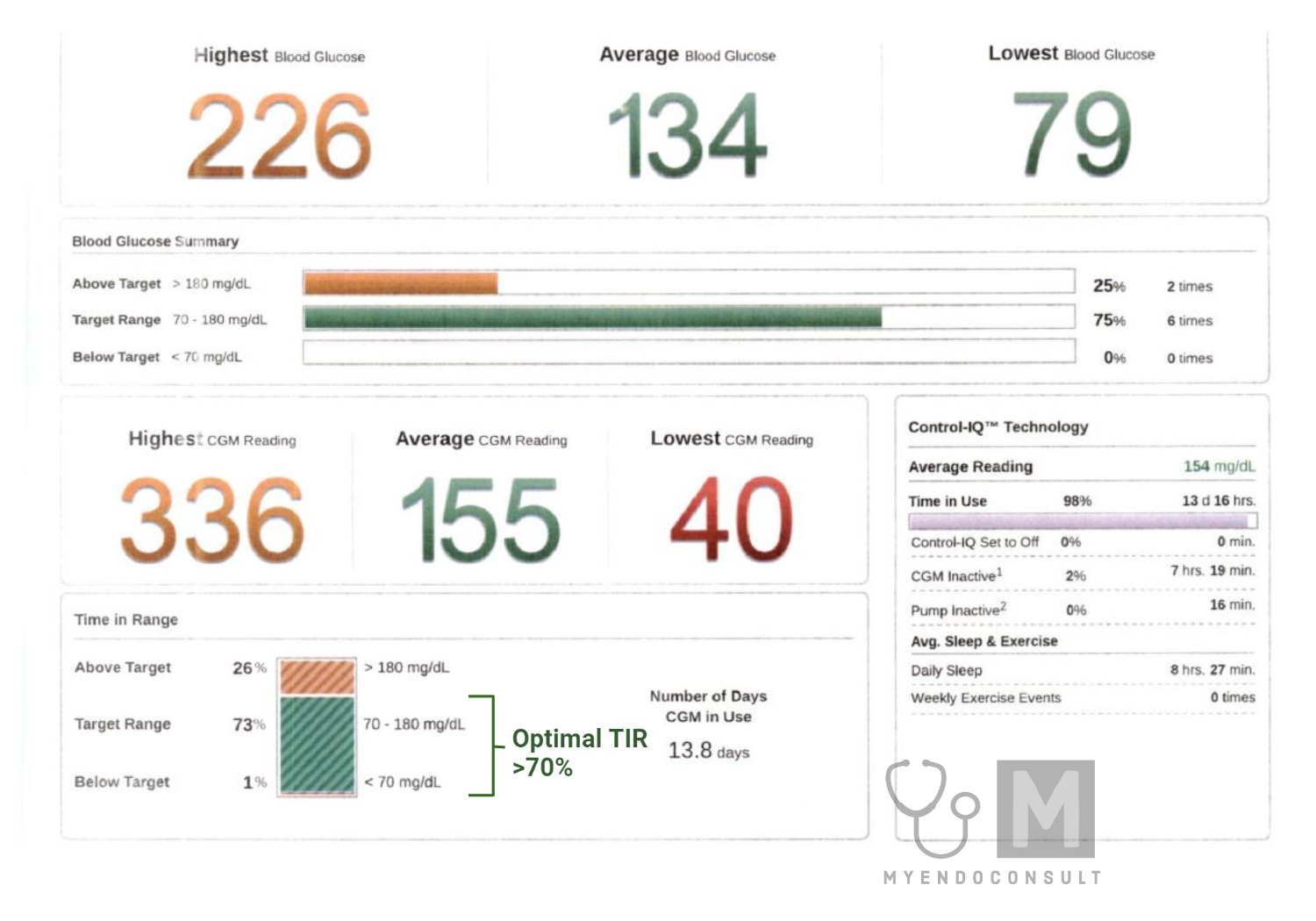
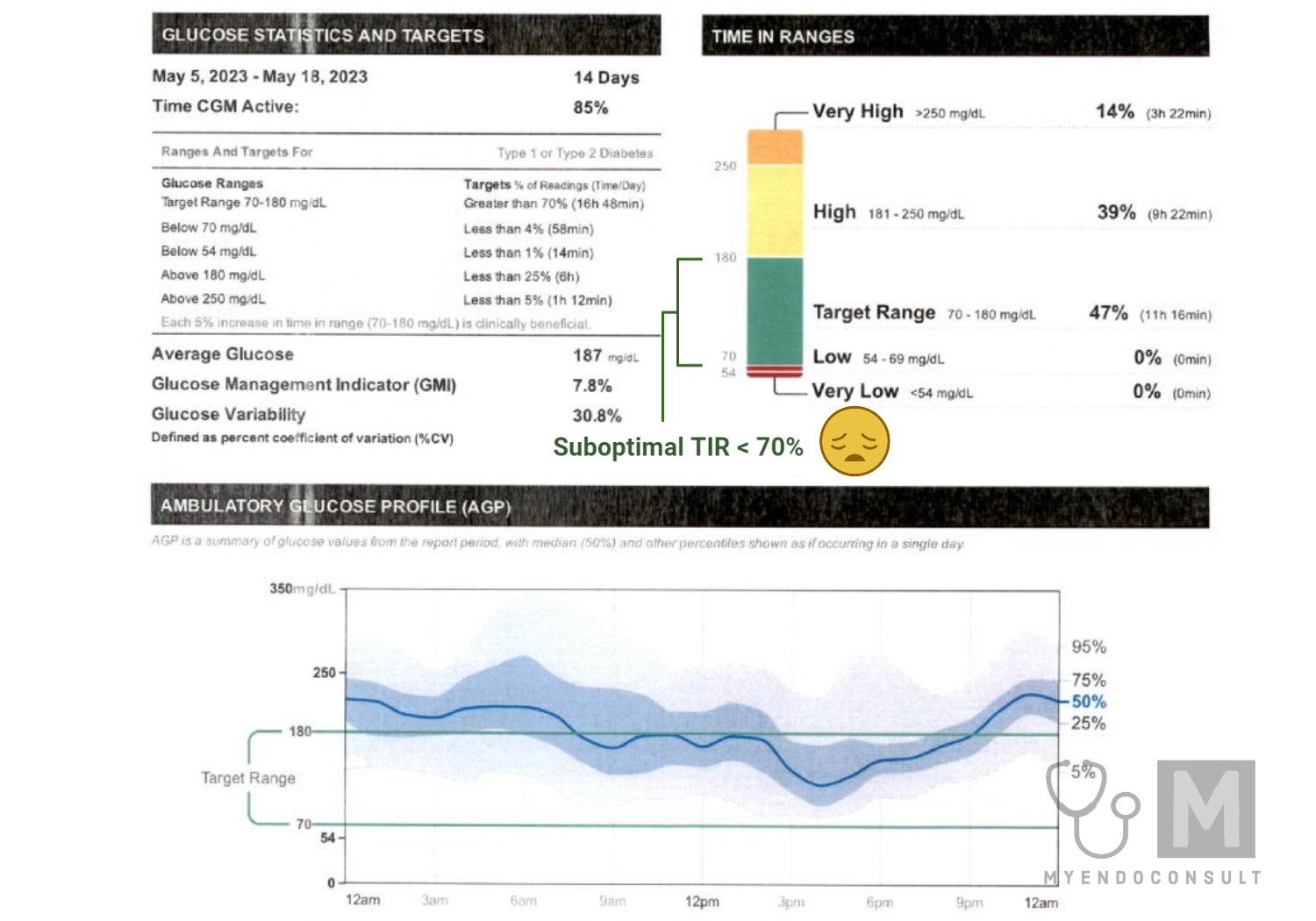
Time in Range (TIR) is a relatively new concept in diabetes management, made possible by the advent of continuous glucose monitoring. TIR refers to the percentage of time that a person’s blood glucose levels stay within a specified target range, generally between 70-180 mg/dL for most adults with diabetes.
The focus on TIR is a significant shift in diabetes care. While the traditional method of assessing glucose control has been to look at Hemoglobin A1C levels, TIR provides a much more detailed and real-time understanding of glucose control. It captures the fluctuations and variations in blood glucose levels throughout the day that A1C testing can miss.
The beauty of the TIR concept is its simplicity. The goal is to maximize the amount of time spent within the target glucose range, minimizing time spent in high or low-glucose states. The benefits of maintaining a higher TIR are profound. It can lead to a better quality of life, lower risk of complications related to diabetes, and reduced hypoglycemia unawareness.
Healthcare professionals can use TIR data to better personalize diabetes management plans. By understanding the patterns and factors affecting an individual’s blood glucose levels, they can tailor interventions around diet, exercise, medication, and lifestyle changes to increase TIR.
In conclusion, understanding and applying the TIR concept can significantly improve the management and outcome of diabetes. Its focus on individual patterns and flexibility empowers those with diabetes to have better control over their health.
Understanding Glucose Levels
Explanation of blood glucose levels and their significance in diabetes
In the human body, glucose serves as a primary source of energy. We get glucose from the foods we eat, and it is carried to cells throughout our bodies via the bloodstream. However, for our bodies to utilize glucose effectively, we require a hormone called insulin, produced by the pancreas. In people with diabetes, the production or use of insulin is impaired, leading to fluctuations in blood glucose levels.
Ideally, blood glucose levels should range between 70 and 130 mg/dL before meals and less than 180 mg/dL two hours after starting a meal for most people with diabetes. However, these ranges can vary depending on individual factors such as age, pregnancy, and comorbid conditions.
Maintaining these target glucose levels is crucial in managing diabetes. Persistent deviations from the normal range can lead to serious health complications over time, highlighting the significance of regular monitoring and effective management.
The danger of extreme glucose levels: Hyperglycemia and Hypoglycemia
In diabetes management, avoiding extreme glucose levels—both high (hyperglycemia) and low (hypoglycemia) are essential.
Hyperglycemia occurs when blood glucose levels rise above the upper limit of the target range. Symptoms include frequent urination, increased thirst, headaches, fatigue, and blurred vision. Over time, uncontrolled hyperglycemia can lead to complications such as heart disease, stroke, kidney disease, vision problems, and nerve damage.
On the other hand, hypoglycemia occurs when blood glucose levels fall below the lower limit of the target range. Symptoms can include shakiness, hunger, confusion, dizziness, and in severe cases, unconsciousness. Frequent episodes of hypoglycemia can also lead to hypoglycemia unawareness, a condition where a person does not feel or recognize the symptoms of low blood sugar.
The limitations of relying solely on A1C levels for glucose control
Hemoglobin A1C (HbA1c) testing has traditionally been the standard measure of long-term blood glucose control. It measures the percentage of hemoglobin (a protein in red blood cells that carries oxygen) that is coated with sugar, providing an average blood glucose level over the past two to three months. However, relying solely on A1C has its limitations.
Firstly, A1C is an average and does not capture fluctuations in blood glucose levels or the occurrence of hypoglycemia and hyperglycemia. For example, a person could have an A1C within the target range but still experience significant glucose highs and lows.
Secondly, A1C can be influenced by factors unrelated to blood glucose levels. Conditions like anemia, kidney disease, liver disease, or recent blood transfusion can affect A1C results.
Lastly, because A1C is an estimate of average blood glucose over several months, it might not reflect recent changes in diabetes management. It may not capture improvements or deteriorations in glucose control over shorter periods.
Consequently, while A1C remains a useful tool in diabetes management, it should be used in conjunction with other measures, such as self-monitoring of blood glucose or continuous glucose monitoring, to provide a more comprehensive view of glucose control.
Defining Time in Range
The concept of Time in Range: Definition and importance
Time in Range (TIR) is a metric used in diabetes management that refers to the percentage of time a person’s blood glucose levels stay within a specified target range over a 24-hour period. It is a concept that has emerged with the rise of continuous glucose monitoring (CGM) technology, which allows for nearly constant monitoring of glucose levels.
The significance of TIR lies in its ability to provide a more comprehensive picture of glucose control as compared to traditional metrics like A1C. While A1C provides an average of blood glucose over a period of months, TIR gives detailed insight into glucose fluctuations throughout the day and night. This information allows for more precise treatment adjustments and proactive management of blood glucose levels, reducing the likelihood of complications associated with hyperglycemia and hypoglycemia.
Ideal target ranges for people with diabetes
The ideal target range for blood glucose can vary slightly among individuals, but for most adults with diabetes, a common target range is between 70-180 mg/dL. The goal of diabetes management is to maximize the time spent within this range, thereby increasing TIR.
Specifically, guidelines suggest aiming for:
- At least 70% of the day within the target range (70-180 mg/dL)
- Less than 4% of the day in hypoglycemia (below 70 mg/dL)
- Less than 1% of the day in severe hypoglycemia (below 54 mg/dL)
- Less than 25% of the day in hyperglycemia (above 180 mg/dL)
Achieving these targets helps to minimize the risk of both short-term and long-term complications related to diabetes.
Differences in target ranges based on type of diabetes, age, pregnancy status, etc.
It’s important to note that target glucose ranges and TIR goals can vary depending on several factors. These include the type of diabetes, age of the patient, presence of comorbid conditions, and other specific situations such as pregnancy.
For example:
- Young children with type 1 diabetes might have a slightly higher target range to reduce the risk of hypoglycemia.
- Older adults or individuals with significant comorbid conditions might also have higher targets to reduce the risk of hypoglycemia, particularly if they are at risk of falls or confusion.
- Pregnant women with pre-existing diabetes or gestational diabetes are usually advised to maintain tighter control of blood glucose to reduce risks to both mother and baby. Their targets might be lower than the usual range.
In conclusion, individualizing target ranges and TIR goals is a crucial aspect of effective diabetes management. It ensures that each person’s unique circumstances and needs are taken into account, optimizing their health outcomes.
The Role of Continuous Glucose Monitoring (CGM) in Tracking Time in Range
How CGM helps in monitoring Time in Range
CGM plays a crucial role in tracking Time in Range (TIR). It provides a granular, 24/7 view of glucose levels, enabling the calculation of the percentage of time an individual spends within their target glucose range in a day.
By constantly monitoring glucose levels, CGM allows for immediate detection of fluctuations and excursions outside of the target range. This means that corrective action can be taken promptly, helping to increase TIR. Additionally, CGM systems can be set to provide alerts when glucose levels are approaching or have crossed thresholds, further supporting proactive glucose management.
With detailed, visual reports of daily and long-term TIR data, individuals and healthcare providers can better understand patterns, track progress, and make necessary adjustments to the diabetes management plan.
Benefits of using CGM for patients and healthcare providers
CGM offers numerous benefits for both patients and healthcare providers. For patients, CGM reduces the burden and inconvenience of frequent finger pricks, offers peace of mind with real-time glucose information and alerts, and empowers them to take proactive control of their glucose management. By understanding how different factors such as diet, exercise, stress, and medication affect their glucose levels, patients can make informed decisions to improve their TIR.
For healthcare providers, CGM provides rich, comprehensive data that goes beyond what A1C or periodic glucose checks can offer. This data allows for more personalized and precise treatment plans. By understanding a patient’s unique glucose patterns, healthcare providers can tailor interventions and advice to their specific needs. This personalized approach can lead to improved patient satisfaction, better adherence to treatment plans, and ultimately, better health outcomes.
Overall, the adoption of CGM technology in diabetes management is a significant step forward in achieving optimal TIR and improving the quality of life for people living with diabetes.
Understanding the Time in Range Metrics
Interpretation of Time in Range Percentages
For most adults with diabetes, the target glucose range is typically between 70-180 mg/dL. Clinical recommendations often suggest that individuals aim to spend at least 70% of their day within this target range. Conversely, spending less than 4% of the day in hypoglycemia (below 70 mg/dL) and less than 25% of the day in hyperglycemia (above 180 mg/dL) are additional goals to aim for.
Interpreting low and high Time in Range
Low TIR indicates that an individual’s blood glucose levels are frequently outside the target range. This could mean they are experiencing frequent episodes of hypoglycemia, hyperglycemia, or both. A low TIR could suggest that modifications to the diabetes management plan may be necessary, such as adjustments to medication, diet, or physical activity.
High TIR, on the other hand, signifies that an individual’s blood glucose levels are consistently within the target range. A high TIR is the goal in diabetes management as it reflects good glucose control, reducing the risk of both immediate and long-term complications.
Link between Time in Range and long-term diabetes control
The concept of TIR has significantly transformed our understanding and management of diabetes. It moves the focus from just controlling average glucose levels to actively managing glucose fluctuations and minimizing time spent in hypoglycemic or hyperglycemic states.
Studies have shown a strong link between higher TIR percentages and better long-term diabetes control. Higher TIR has been associated with lower risks of microvascular complications, such as retinopathy (eye disease), nephropathy (kidney disease), and neuropathy (nerve damage). Similarly, minimizing time spent in hyperglycemia and hypoglycemia reduces the risk of acute complications like diabetic ketoacidosis and severe hypoglycemic episodes.
Furthermore, maintaining higher TIR percentages can improve quality of life for people with diabetes. Better glucose control means fewer symptoms related to high or low blood sugars, less worry about fluctuating glucose levels, and more freedom in daily life.
In summary, focusing on TIR as a key part of diabetes management is beneficial for long-term glucose control, reducing complications, and improving quality of life. It provides a more detailed, nuanced picture of an individual’s glucose control and allows for more personalized and effective management strategies.
Practical Tips to Improve Time in Range
Dietary Considerations
Diet plays a vital role in managing diabetes and improving Time in Range (TIR). Here are a few considerations:
- Balanced Diet: A diet high in fiber, low in saturated fats and sugar, and filled with fruits, vegetables, lean proteins, and whole grains can help maintain steady glucose levels.
- Carbohydrate Counting: Understanding how carbohydrates affect blood glucose levels can help individuals plan meals and make healthier food choices.
- Consistency: Maintaining consistent meal times and avoiding skipping meals can help prevent sudden swings in blood glucose levels.
- Portion Control: Eating controlled portions can prevent overeating, which can lead to spikes in blood sugar.
Role of Regular Exercise
Physical activity is crucial in diabetes management. Regular exercise helps the body use insulin more efficiently, which can lower blood glucose levels and increase TIR.
- Consistency: Aim for at least 150 minutes of moderate to vigorous aerobic activity per week, such as brisk walking or cycling.
- Strength Training: Include strength training exercises in your routine at least twice a week.
- Monitor Glucose: Be aware that exercise can affect glucose levels, and adjust your diabetes management plan as needed. Monitor your glucose levels before, during, and after exercise.
Importance of Medication Adherence
Taking prescribed medication consistently and correctly is critical for achieving optimal TIR.
- Understand Your Medication: Know what medications you are taking, their purpose, and the correct doses and timings.
- Consistency: Take your medication as prescribed. Missing doses or not taking medication correctly can lead to fluctuations in glucose levels.
- Communicate with Healthcare Team: If side effects occur or if the medication does not seem to be working, discuss it with your healthcare provider. Never adjust or stop your medication without consulting your healthcare team.
Stress Management and Sleep’s Impact on Glucose Levels
Both stress and lack of sleep can significantly affect blood glucose levels and TIR.
- Stress Management: Chronic stress can lead to persistently elevated glucose levels. Techniques such as mindfulness, yoga, deep breathing, and other stress-reduction techniques can help manage stress levels.
- Quality Sleep: Lack of sleep or poor-quality sleep can increase insulin resistance and lead to higher glucose levels. Aim for 7-9 hours of sleep per night. Maintaining a consistent sleep schedule and creating a restful environment can improve sleep quality.
By incorporating these practical tips into your daily routine, you can significantly improve your Time in Range, leading to better diabetes control and a healthier life.
The Future of Diabetes Management: Personalized and Predictive
How Time in Range is Driving Personalized Diabetes Treatment Plans
TIR is reshaping how healthcare providers approach diabetes management. As it offers a detailed view of an individual’s glucose fluctuations throughout the day, TIR data allows healthcare providers to tailor treatment plans based on unique patterns and challenges that emerge.
For example, someone might consistently experience morning hyperglycemia due to the dawn phenomenon, while another person may struggle with post-meal spikes. By identifying these unique patterns, treatment plans can be personalized to address these specific challenges, such as adjusting the timing or dosage of medication, or providing specific dietary guidance.
Additionally, as TIR goals may vary based on factors like age, pregnancy, and presence of comorbidities, treatment plans can be further individualized to consider these factors, leading to more effective, patient-centered care.
The Potential of Machine Learning and AI in Predicting and Improving Time in Range
As we move towards a future of predictive diabetes management, machine learning and artificial intelligence (AI) hold enormous potential.
Machine learning algorithms can analyze vast amounts of data from CGM devices, along with other relevant data such as food intake, physical activity, medication use, and more. These algorithms can then predict future blood glucose levels based on this data, providing alerts for potential hypoglycemic or hyperglycemic events before they happen. This predictive capability can help individuals proactively adjust their actions, such as eating a snack to prevent a predicted hypoglycemic event or taking additional insulin to mitigate a predicted glucose spike.
Furthermore, AI can potentially suggest personalized recommendations for improving TIR, based on patterns in the individual’s data. For example, it might suggest specific dietary modifications or exercise routines that could improve TIR based on past data.
The integration of TIR, AI, and machine learning represents the future of diabetes management, aiming for a scenario where diabetes care is not just reactive but also predictive and proactive. This transition can significantly improve glucose control, reduce complications, and enhance the quality of life for individuals living with diabetes.
References
Bellido V, Pinés-Corrales PJ, Villar-Taibo R, Ampudia-Blasco FJ. Time-in-range for monitoring glucose control: Is it time for a change? Diabetes Res Clin Pract. 2021 Jul;177:108917. doi: 10.1016/j.diabres.2021.108917.
Dovc K, Battelino T. Time in range centered diabetes care. Clin Pediatr Endocrinol. 2021;30(1):1-10. doi: 10.1297/cpe.30.1. Epub 2021 Jan 5.
Bellido V, Aguilera E, Cardona-Hernandez R, Diaz-Soto G, González Pérez de Villar N, Picón-César MJ, Ampudia-Blasco FJ. Expert Recommendations for Using Time-in-Range and Other Continuous Glucose Monitoring Metrics to Achieve Patient-Centered Glycemic Control in People With Diabetes. J Diabetes Sci Technol. 2022 Apr 26:19322968221088601.
Kindly Let Us Know If This Was helpful? Thank You!


