Adrenal vein sampling (AVS) plays a pivotal role in differentiating between unilateral and bilateral adrenal disease among patients diagnosed with primary aldosteronism. This article offers a concise review of the preparation, precautions and interpretation of AVS results to ensure accurate diagnosis and optimal patient outcomes.
Optimal preparation for adrenal vein sampling
To obtain reliable AVS results, patients must follow these guidelines:
- Patients should refrain from eating before the test to reduce potential confounding variables and ensure consistent physiological conditions.
- AVS should be scheduled in the morning, with the patient lying supine for at least one hour prior to the procedure. This helps stabilize hormonal levels and minimize fluctuations.
- Also, patients must achieve normokalemia prior to the procedure to avoid skewed results and ensure safety during AVS.
Precautions and Complication Rates
The centers performing AVS report a complication rate of 2.5% or less. Proper techniques, thorough preparation, and appropriate patient selection are essential to maintain low complication rates. Furthermore, the accuracy of the results is very much dependent on the expertise of the clinician performing the test. For these reasons, clinicians should refer all patients to high volume centers, typically large tertiary or quartenary health facilities for AVS.
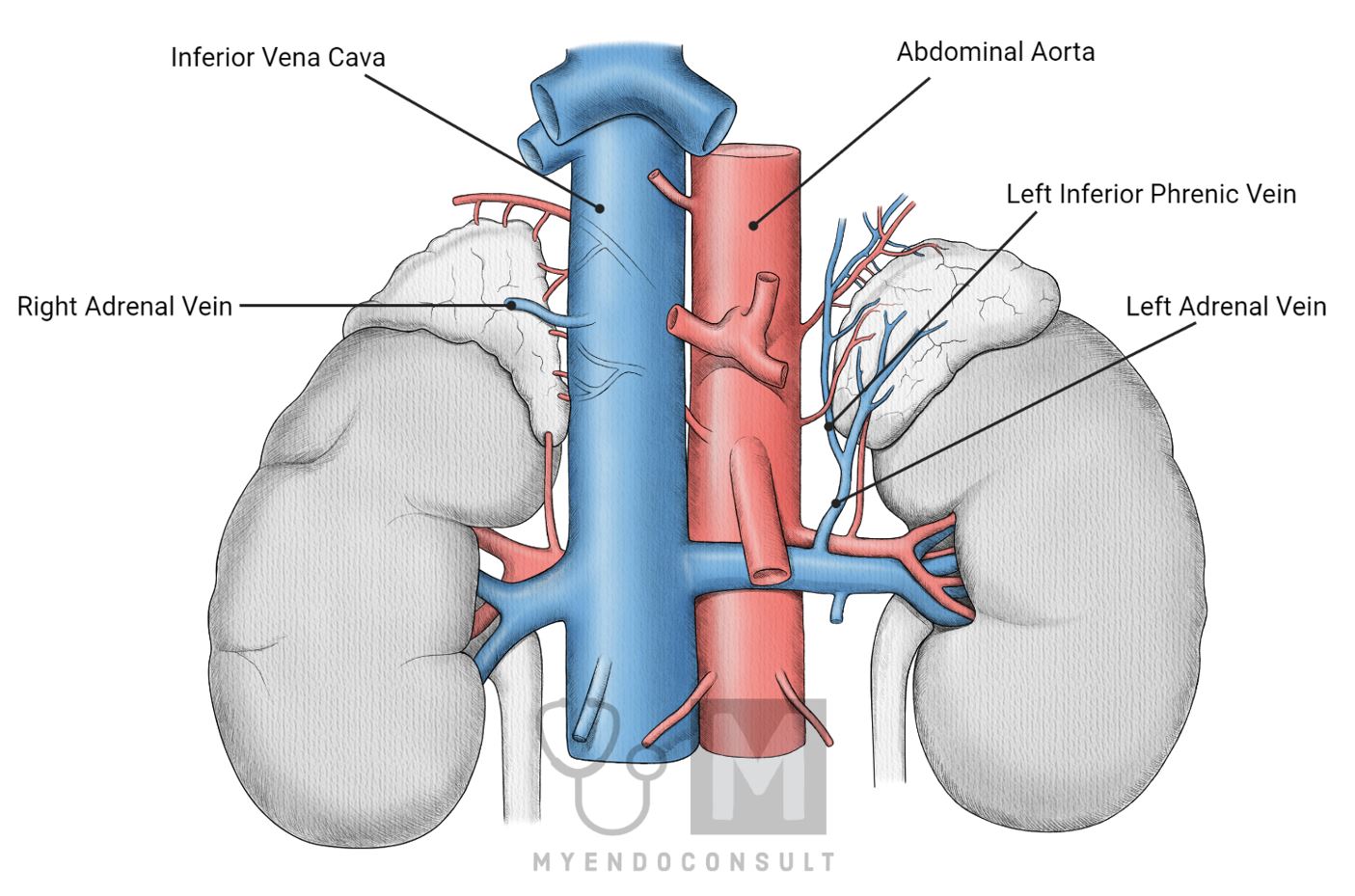
Vascular supply of the adrenal glands
Knowledge of venous drainage patterns helps radiologists and interventionalists navigate complex vascular structures and safely access adrenal veins.
During AVS, simultaneous blood samples are collected from both adrenal veins and the inferior vena cava (IVC) to measure aldosterone and cortisol concentrations. Furthermore, proper catheterization and sample collection are crucial for interpreting the AVS results and determining the source of excess aldosterone. Awareness of the potential dilutional effect on the left adrenal vein is essential for accurately calculating cortisol-corrected aldosterone ratios (A/C ratios) and guiding clinical decision-making.
Arterial Supply of Adrenal Glands
The arterial supply to the adrenal glands is relatively constant and each gland receives blood from three main sources.
- Superior Adrenal Arteries: These arteries originate from the inferior phrenic arteries of the abdominal aorta.
- Middle adrenal arteries: These arteries originate directly from the abdominal aorta and supply the lateral aspect of the adrenal glands.
- Inferior Adrenal Arteries: These arteries branch from the renal arteries, which also arise from the abdominal aorta.
The rich arterial supply to the adrenal glands ensures adequate blood flow for hormone production and secretion.
Venous Drainage of Adrenal Glands
Venous drainage of the adrenal glands is asymmetric and more variable than its arterial supply, particularly relevant for AVS procedures.
Right adrenal gland: The right adrenal gland typically has a single adrenal vein that drains directly into the inferior vena cava (IVC). The short and direct route to the IVC can make catheterization of the right adrenal vein more challenging during AVS.
Left Adrenal Gland: The left adrenal gland usually has a single adrenal vein that drains into the left renal vein or the left inferior phrenic vein. Due to the more indirect drainage route, the left adrenal vein may be more accessible for catheterization during AVS. However, the flow of the dilutional effect of the inferior phrenic vein to the left adrenal vein must be considered when interpreting the AVS results.
Procedure
- The patient may be asked to stop certain medications, such as aldosterone antagonists, ACE inhibitors, or diuretics, for a period before the procedure to ensure accurate results. As was mentioned previously, they may also be advised to fast for a few hours before the test.
- The patient is positioned comfortably, typically lying on their back. The skin at the catheter insertion site (usually the groin area) is cleaned and sterilized, and local anesthesia is administered to numb the area.
- A small incision is made at the insertion site, and a radiologist inserts a thin, flexible catheter into a large vein, typically the femoral vein in the groin.
- The catheter is carefully advanced through the venous system under fluoroscopic guidance (real-time X-ray imaging) to reach the adrenal veins. The correct positioning of the catheter is crucial for obtaining accurate blood samples.
- Blood samples are collected from both adrenal veins and a peripheral vein (often from the arm or groin). The samples are typically drawn simultaneously or sequentially, depending on the preference of the interventional radiologist and the patient's anatomy.
- Once the blood samples have been collected, the catheter is carefully removed, and pressure is applied to the insertion site to prevent bleeding. The incision is then closed with a bandage.
- The blood samples are sent to a laboratory for analysis of aldosterone and cortisol levels.
Interpretation of AVS Results
Confirming Successful Catheterization
Cosyntropin infusion is commonly used to ensure successful catheterization of the right and left adrenal veins. A cortisol ratio of at least 3:1 (adrenal vein to IVC) is necessary for confidence in successful catheterization. In the absence of cosyntropin infusion, a cortisol gradient greater than 2:1 is recommended. Most institutions prefer AVS with cosyntropin stimulation because of its superior accuracy.
Correcting Aldosterone Levels and Interpreting A/C Ratios
To calculate cortisol-corrected aldosterone ratios (A/C ratios), divide the plasma aldosterone concentrations of the right and left adrenal veins by their corresponding cortisol concentrations. This process compensates for the dilutional effect caused by the flow of the inferior phrenic vein into the left adrenal vein.
When cosyntropin infusion, a cutoff A/C ratio greater than 4:1 from the high side to the low side indicates unilateral excess aldosterone, with a true positive rate of 88%. An A/C ratio below 3.0 implies bilateral aldosterone hypersecretion, while ratios between 3 and 4 signify a zone of overlap.
If the A/C ratio on the low side is less than the IVC A/C ratio, the tumor is on the contralateral side in most patients with surgically confirmed APA. This criterion is particularly valuable in patients who have only undergone successful adrenal vein catheterization on one side.
Read this article if you are interested in learning more about AVS interpretation (attempt questions and learn a simple method for interpreting this test on the board exam).
Caveats and Recommendations
• Performing AVS without cosyntropin stimulation is not recommended due to elevated false positive rates.
• Medications known to increase renin secretion (for example, mineralocorticoid receptor (MR) antagonists [spironolactone and eplerenone], high-dose amiloride [i.e., > 5 mg/day], ACE inhibitors, ARB and renin inhibitors [eg, aliskiren]) must be discontinued for a minimum of 4 weeks before AVS.
• Control of blood pressure before AVS should preferably be managed using extended-release verapamil, peripheral alpha-adrenergic receptor antagonists (eg, doxazosin, terazosin, and prazosin), and hydralazine. These medications are less likely to interfere with AVS results and help maintain stable blood pressure during the procedure.
Additional Considerations
• Imaging Techniques: Noninvasive imaging techniques, such as CT (CT) or magnetic resonance imaging (MRI), may provide valuable information about adrenal anatomy and help guide the AVS procedure. However, they should not be solely relied upon for lateralizing aldosterone secretion, as their sensitivity and specificity can be limited.
• The development of new catheter designs, imaging modalities, and radiological techniques may further improve the success and safety of AVS procedures in the future. Ongoing research and clinical trials are essential to refine and optimize AVS methods.
• Patients should receive thorough preprocedure counseling to understand AVS's risks, benefits, and potential outcomes. Open communication and shared decision-making between healthcare providers and patients are critical to ensure optimal results and patient satisfaction.
• After successful AVS and unilateral or bilateral identification of adrenal disease, appropriate management strategies should be implemented. This may include surgical intervention, such as adrenalectomy for unilateral disease or medical therapy for bilateral disease. Close follow-up and monitoring are essential to evaluate the effectiveness of treatment and identify potential complications.
Conclusion
Adrenal vein sampling is a vital diagnostic tool to differentiate between unilateral and bilateral adrenal disease in patients with primary aldosteronism. By adhering to the recommended preparation guidelines, taking the necessary precautions, and accurately interpreting AVS results, healthcare professionals can optimize patient outcomes and improve overall quality of care. Continuing research and advancements in technology hold promise for enhancing the precision and safety of AVS procedures in the future.
References
Webb, R., Mathur, A., Chang, R., Baid, S., Nilubol, N., Libutti, SK, Stratakis, CA, Kebebew, E. What is the best criterion for the interpretation of adrenal vein sample results in patients with primary hyperaldosteronism? Ann Surg Oncol. 2012 Jun;19(6):1881-6.
Fingeret, A.L., Lee, J.A. Adrenal Venous Sampling in Primary Hyperaldosteronism. Curr Surg Rep 2, 38 (2014).
Kindly Let Us Know If This Was helpful? Thank You!


