The cortisol to cortisone shunt requires 2 isoforms of the 11beta-hydroxysteroid dehydrogenase enzyme. The liver and kidneys play a significant role in the physiologic regulation of cortisol action.
The concept of physiologic “cortisol resistance”
Cortisol can bind both glucocorticoid and mineralocorticoid receptors, and indeed under normal physiological conditions, plasma levels of cortisol are up to 1,000-fold higher than that of aldosterone. 11beta-hydroxysteroid dehydrogenase type 2 (11β-HSD2) inactivates physiological concentrations of cortisol and thus protects the mineralocorticoid receptor from direct activation by cortisol[1].
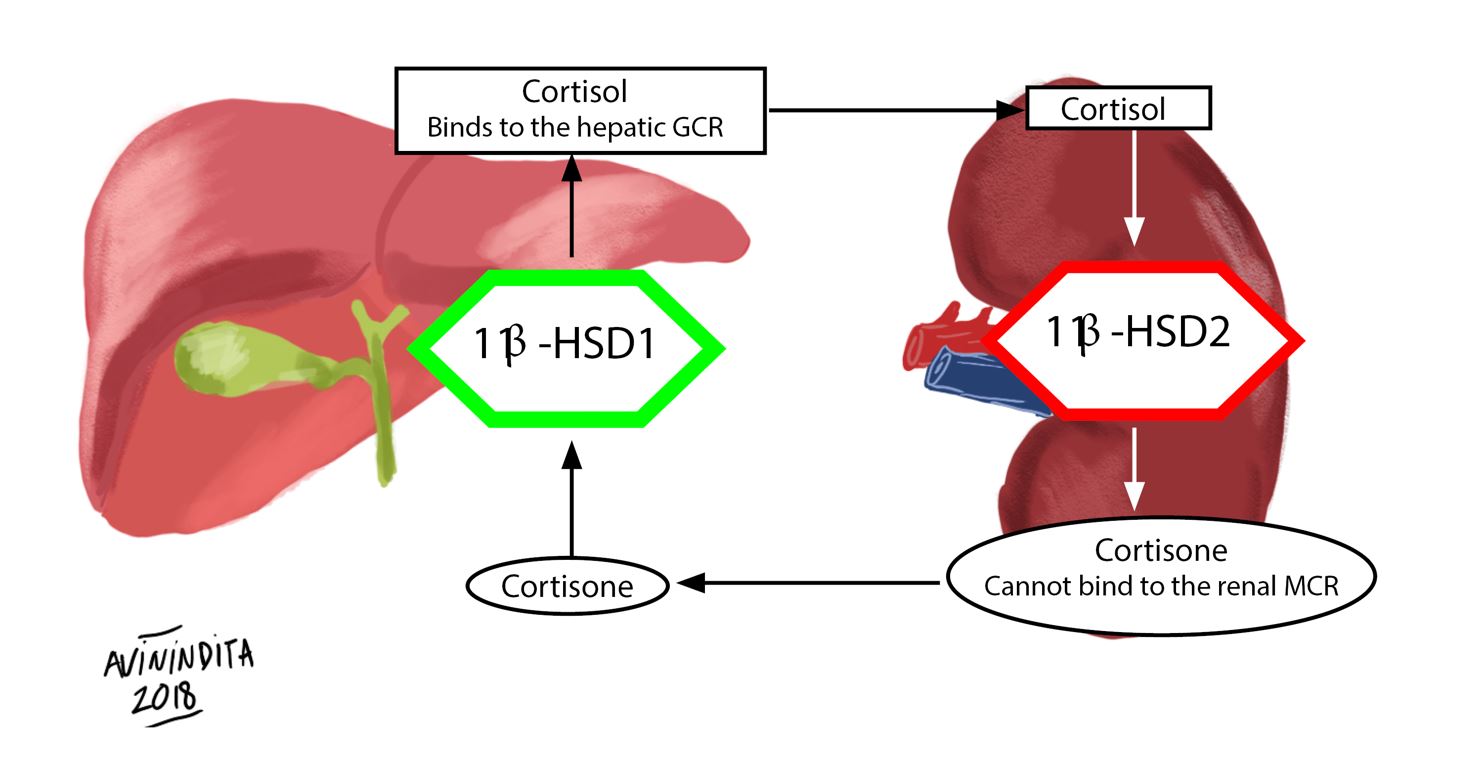
Fig. 1 The Cortisol-to-Cortisone Shunt
The two isoforms of 11beta-hydroxysteroid dehydrogenase play essential roles in the cortisol-to-cortisone shunt. 11beta-hydroxysteroid dehydrogenase type 1 (11β HSD1) converts inactive cortisone to active cortisol in the liver, which subsequently binds its cognate hepatic glucocorticoid receptor (GCR)(dark arrows). 11beta-hydroxysteroid dehydrogenase type 2 (11β HSD2) converts active cortisol to inactive cortisone at the level of the kidney, thus protecting the mineralocorticoid receptor (MCR) from activation by cortisol(white arrows)[2].
Comparison of the isoforms of 11β HSD
| 11β HSD1 | 11β HSD2 |
| Increases circulating levels of cortisol | Promotes physiological cortisol resistance |
| Absent from the kidney | Present in the kidney |
| Absent from sweat and salivary glands | Present in sweat and salivary glands |
| Present in the liver | Absent from the liver |
| Present in osteoblasts and osteocytes | Absent from bone |
| Present in adipose tissue | Absent from adipose tissue |
Data derived from references[3–5]
Clinical Pearl
Treatment of adrenal crises
Patients with adrenal crises because of Addison’s disease do not require concomitant fludrocortisone (mineralocorticoid) administration if their total daily dose of steroids is greater than or equal to 50mg of hydrocortisone, or steroid equivalent. Supraphysiologic doses of hydrocortisone, given during an emergency, will activate the mineralocorticoid receptor and thus provide additional “mineralocorticoid coverage.” Patients managed with methylprednisolone may, and those taking dexamethasone will require mineralocorticoid due to limited binding of the former and zero binding of the latter to mineralocorticoid receptors [6].
https://youtu.be/x38_iiSoc98
References
- Gomez-Sanchez E, Gomez-Sanchez CE (2014) The Multifaceted Mineralocorticoid Receptor. Compr Physiol 4:965–994
- Stewart PM, Murry BA, Mason JI (1994) Human kidney 11 beta-hydroxysteroid dehydrogenase is a high affinity nicotinamide adenine dinucleotide-dependent enzyme and differs from the cloned type I isoform. J Clin Endocrinol Metab 79:480–484
- Tomlinson JW, Stewart PM (2001) Cortisol metabolism and the role of 11β-hydroxysteroid dehydrogenase. Best Practice & Research Clinical Endocrinology & Metabolism 15:61–78
- Loerz C, Maser E (2017) The cortisol-activating enzyme 11β-hydroxysteroid dehydrogenase type 1 in skeletal muscle in the pathogenesis of the metabolic syndrome. The Journal of Steroid Biochemistry and Molecular Biology 174:65–71
- Draper N, Stewart PM (2005) 11beta-hydroxysteroid dehydrogenase and the pre-receptor regulation of corticosteroid hormone action. J Endocrinol 186:251–271
- Arlt W (2009) The Approach to the Adult with Newly Diagnosed Adrenal Insufficiency. J Clin Endocrinol Metab 94:1059–1067
Kindly Let Us Know If This Was helpful? Thank You!


