The prevalence of cutaneous manifestations of diabetes mellitus (both Type 1 and Type 2) ranges between 30 to 70%. The clinical features and underlying mechanism of these dermatologic features of diabetes mellitus will be described next.
Acanthosis nigricans
| Feature | Notes |
| Description | Poorly delineated plaques with a grey to dark-brown pigmentation. Typically has a velvety texture. |
| Location | Intertriginous and other flexural areas (axilla, elbows, inframammary regions, palms – known as “Tripe palms”). |
| Mechanism | • Insulin activates IGF-1 receptors present on fibroblasts and keratinocytes • Additionally, hyperinsulinemia causes a decrease in IGF binding proteins, which results in a higher level of unbound (active) IGF-1 (vicious cycle) • Androgens and growth factor receptors are present on keratinocytes and fibroblasts as well (may explain other hormonal causes of acanthosis nigricans) |
| Treatment | • Improvement in insulin resistance (metformin, dietary changes, increased physical activity, and weight reduction) |

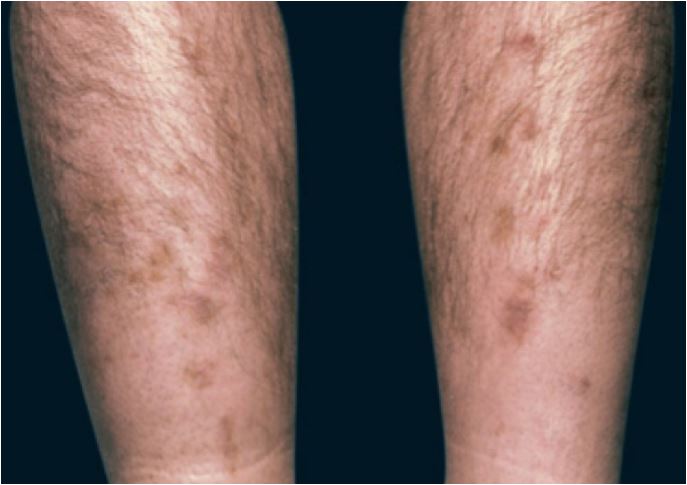
Diabetic dermopathy
| Feature | Notes |
| Description | Hyperpigmented and circumscribed red papules that change over 1-2 weeks into atrophic brown papules |
| Location | Pretibial area |
| Mechanism | Neuropathy and microangiopathy induced by uncontrolled diabetes mellitus |
| Treatment | It is self-limited and largely asymptomatic, as such treatment is not required |
Acrochordons (skin tags)
| Feature | Notes |
| Description | Pedunculated cutaneous fibromas |
| Location | Flexural areas in the neck and axilla, in a pattern akin to the distribution of acanthosis nigricans |
| Mechanism | Hyperinsulinemia promotes the activation of fibroblast bound IGF-1 receptors present in the epidermis. This is followed by the proliferation of skin fibroblasts and subsequent development of skin tags. |
| Treatment | No treatment is required |
Necrobiosis lipoidica diabeticorum (NLD)
| Feature | Notes |
| Description | A red-brown papule that progressively increases in diameter and eventually changes into the classic waxy, yellowish lesion. There is occasional central ulceration, which manifests as an atrophic center. Exhibits Koebnerization. |
| Location | Present almost always on pretibial areas of the lower extremities |
| Mechanism | There is initial tissue hypoperfusion in the skin due to microangiopathy involving skin capillaries. Microangiopathy occurs as a result of the accumulation of advanced glycated end products in the vasculature, which consequently promotes local oxidative stress. Inflammatory mediators which have accumulated in response to tissue hypoperfusion lead to a progressive breakdown in collagen |
| Treatment | Topical or intra-lesional corticosteroids |

Lipodystrophy
| Feature | Description |
| Description | Localized lipodystrophy due to insulin injections is an umbrella term that consists of the lipoatrophy (LA) and lipohypertrophy (LH) subtypes. LA tends to appear as an area of subcutaneous tissue loss, which creates a dimple in the skin. LH, however, has a firm, rubbery consistency that is palpable in the subcutaneous tissue plane. Occasionally, LH lesions may be soft, making them difficult to discern on routine physical examination. |
| Location | Sites of insulin injections |
| Mechanism | • Lipoatrophy occurs as a result of an immune-mediated reaction to insulin; it is less prevalent now due to the use of modern human insulin or human-like insulin analogs. • Lipohypertrophy is due to the growth-promoting effects of insulin on fibroblasts in the subcutaneous tissue. Insulin binds to IGF-1 receptors on fibroblasts which leads to the activation and subsequent proliferation of fibroblasts |
| Treatment | Rotation of sites of insulin injection |
Bullosis Diabeticorum
| Feature | Notes |
| Description | Sudden onset of one or more non-erythematous, firm and sterile bullae containing a clear fluid. They may range in size from 0.5cm to 5cm. |
| Location | Usually located on the lower extremities |
| Mechanism | Unknown |
| Treatment | These can be aspirated for symptomatic relief. |
Scleroderma diabeticorum
| Feature | Notes |
| Description | Thickened, waxy, or edematous indurated plaques |
| Location | Distributed over the neck and upper back. Diabetic hand syndrome, a form of scleroderma-like skin change of diabetes, may present with limited joint mobility, palmar fibromatosis (Dupuytren's contracture), or stenosing tenosynovitis (“trigger finger”) |
| Mechanism | Reduced breakdown of collagen fibers due to nonenzymatic glycosylation of dermal collagen |
| Treatment | None |
Eruptive xanthoma
| Feature | Notes |
| Description | Yellowish papules |
| Location | Located over the trunk and extensor surfaces such as the elbows and knees. |
| Mechanism | Reduced lipoprotein lipase activity due to insulin resistance or insulinopenia causes impaired storage of triglycerides in adipose tissue. As a consequence, triglycerides accumulate in the skin. |
| Treatment | Treatment of diabetes. Surgical treatment in select cases |
Download Dermatologic manifestations of diabetes mellitus ppt (powerpoint format)
References
Duff M, Demidova O, Blackburn S, Shubrook J. Cutaneous manifestations of diabetes mellitus. Clin Diabetes. 2015;33(1):40-48.
Images(s) Courtesy
Masryyy, CC BY-SA 4.0 , via Wikimedia Commons (Acanthosis nigricans)
Kindly Let Us Know If This Was helpful? Thank You!


