Diabetes mellitus is an endocrine condition in which patients have elevated blood glucose levels (hyperglycemia). Insulin is a hormone produced by the pancreas.
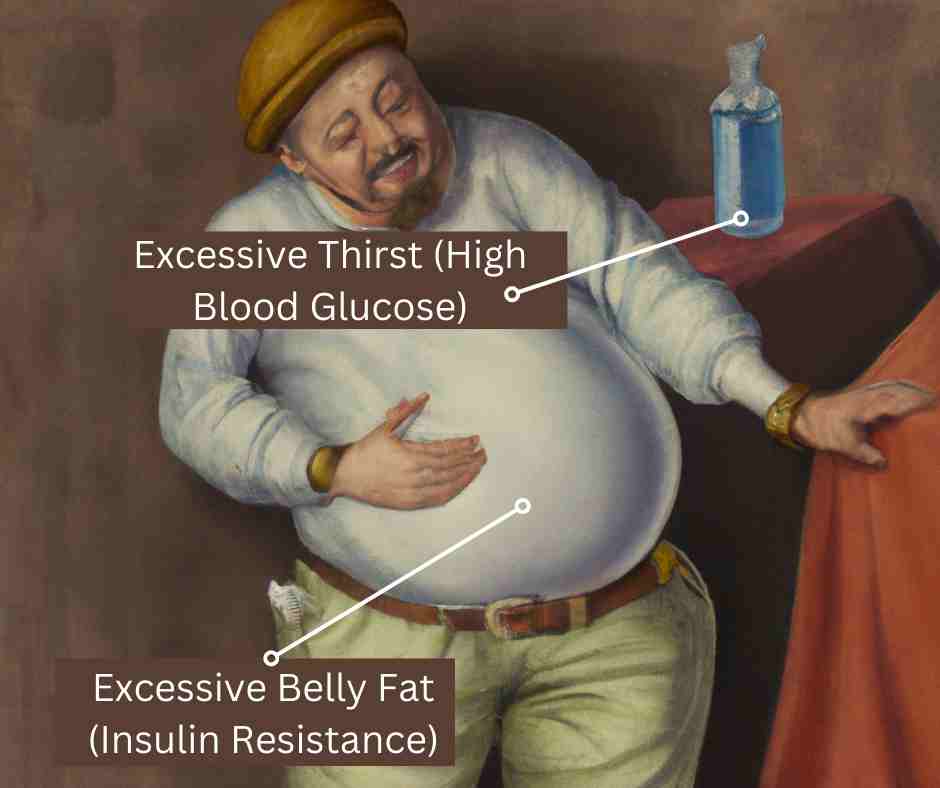
The classic symptoms of untreated or undertreated diabetes are:
- Frequent urination (polyuria),
- Polydipsia (excessive thirst), and
- Involuntary weight loss.
- There are four different classes of diabetes mellitus:
- Type 1 diabetes
- Type 2 diabetes
- Gestational diabetes
- Specific types of diabetes due to other causes
Type 1 Diabetes
- Other names: insulin dependent diabetes mellitus (IDDM), juvenile onset diabetes.
- Physiology: There is no production of insulin by the body.
- Ketosis-prone: Patients with this type of diabetes are ketosis-prone. This means that if they do not receive daily insulin shots, their bodies break down fats and produce ketones. The ketones spill into the urine and can be measured. Patients with type I diabetes are at risk for developing Diabetic KetoAcidosis (DKA), a life-threatening condition.
- Onset: It most commonly first appears in childhood or adolescence. Approximately 10% of diabetics are type 1.
- Treatment: Subcutaneous insulin is required and needs to be given a least once daily. Patients striving for tighter control of their blood glucose will take insulin more often than once a day.
- Recommended therapy for type 1 diabetes includes: 1) use of multiple-dose insulin injections (3-4 injections per day) and 2) matching of mealtime (prandial) insulin to carbohydrate intake, before meal blood glucose reading, and anticipated exercise.
Type 2 Diabetes
- Other names: Non-Insulin Dependent Diabetes Mellitus (NIDDM), Adult-Onset Diabetes
- Physiology: There is decreased insulin production and decreased sensitivity to insulin.
- Not ketosis-prone: These patients are not prone to ketosis. DKA rarely occurs.
- Onset: It more commonly develops in elderly and overweight adults.
- Treatment: The initial and most important treatments are exercise and weight loss. When these measures fail, oral medicines (e.g., metformin) can be prescribed. These medicines help the body make more insulin or use the insulin more effectively. Occasionally patients require insulin therapy.
- Diagnosis: Probably the best way to diagnose diabetes is an A1C test. A value of 6.5% or above indicates diabetes. There are two other tests that have long been used for diagnosing diabetes: a fasting plasma glucose (FPG) of 126 mg/dL (7.0 mmol/L) or above and a 2-hour oral glucose tolerance test (OGTT) with a glucose of 200 mg/dL (11.1 mmol/L) or above.
The pathophysiologic defects in type 2 diabetes mellitus has been summarised in the ominous octet and egregious eleven.
Gestational Diabetes
Gestational diabetes is diabetes that is found for the first time when a woman is pregnant.
- Other names: Pregnancy-induced diabetes
- Physiology: In gestational diabetes, the body is not making sufficient insulin to keep pace with the weight gain and other hormonal changes of pregnancy.
- Not ketosis-prone: These patients are not prone to ketosis. DKA rarely occurs.
- Onset: It occurs during pregnancy.
- Treatment: A meal plan and regular physical activity are important. If these measures fail, diabetes medicine (usually insulin) may be prescribed.
Diabetic Ketoacidosis (DKA)
- Definition: Blood glucose > 240 mg/dL (13.3 mmol/L) with acidosis and ketosis (urine ketones moderate to large; or blood ketones > 1.4 mmol/L)
- Symptoms of DKA: In addition to symptoms of hyperglycemia, fruity odor on breath, vomiting, rapid/deep breathing, confusion, and coma.
- Causes: Poor compliance or inadequate use of insulin in type 1 diabetes, infections.
Ketone Testing
- People with diabetes who take insulin should test for ketones when their blood sugar is more than 240 mg/dL (13.3 mmol/L). They should also check for ketones when they are sick or have symptoms of ketoacidosis (vomiting, fruity breath, or rapid breathing). Detecting ketosis early is important in order to help prevent life-threatening diabetes ketoacidosis.
There are now two ways patients can test for ketones at home.
- Urine Ketone Tests: Many patients test for urine ketones (urine acetoacetrate) by doing a urine ketone test. Urine ketone strips are available at local pharmacies. The results indicate the amount of urine ketones as small, moderate, or large. Moderate to large amount ketones indicate ketosis.
- Blood Ketone Tests: Some blood glucose test meters now allow the patient to also test for blood ketones (blood beta-hydroxybutyrate). The patient can often test for blood ketones and blood glucose at the same time. The blood ketone test does require a different strip made just for ketone tests. Blood ketone tests may detect ketones a bit sooner than urine ketone test. The blood ketone tests give the patient a number reading. A number below 0.6 mmol/L is considered normal. Numbers between 0.6 to 1.4 mmol/L means ketosis is developing and the patient should call their doctor for further instructions. Numbers more than 1.4 mmol/L means ketosis is concerning and patients should call their doctor or seek medical care now.
Types Of Insulin
There are different types of insulin. They vary in how quickly they start to work, when they peak, and how long they last.
- Rapid-acting (Humalog/lispro, NovoLog/aspart, Apidra/gluisine): onset 5-15 minutes; peaks 30-90 minutes; lasts 4-6 hours.
- Short-acting (Regular, Humulin R, Novolin R): onset 30-60 minutes; peaks 2-3 hours; lasts 5-8 hours.
- Intermediate-acting (NPH, Lente, Humulin N, Humulin L, Novolin N, Novolin L): onset 2-4 hours;peaks 4-12 hours; lasts 10-18 hours.
- Long-acting (Lantus/glargine, Levemir/detemir): onset 2-4 hours; no true peak; lasts 18-24 hours.
- Newer long-acting insulins (Tresiba/degludec, Basaglar/glargine, Toujeo/glargine): last more than 24 hours.
- Pre-mixed (Humulin 70/30, Humulin 50/50, Humalog mix, NovoLog mix): 2 peaks; lasts 10-16 hours;depends on mixture.
- Inhaled (Afrezza): onset 12-15 minutes; peaks 35-55 minutes; lasts 3 hours.
Insulin administration schedules
Insulin is required for all people with type 1 diabetes. It is sometimes needed for people with type 2 diabetes.
- Insulin Injections: Once daily long-acting insulin works by providing the basal (baseline) level of insulin the body needs all day long. It does not cover the extra insulin needed when a person eats meals. It may be used alone in patients with type 2 diabetes. Patients with type 1 diabetes often need a combination of insulin types (shorter and longer-acting) and may need 3 to 4 injections per day.
- Continuous subcutaneous insulin infusion
People can take insulin in different ways:
- Injection or shot (needle and syringe)
- Insulin pen
- Insulin pump
- An inhaled form of insulin (Afrezza)
Types Of Oral Medicines
There are many different types of oral medicines (pills) for treating diabetes.
- Alpha-glucosidase inhibitors: Examples include acarbose (Precose, Glucobay) and miglitol (Glyset).
- Biguanides: Examples include metformin (Glucophage, Glumetza, Fortamet, generics). Metformin is the preferred first drug to use in people with type 2 diabetes.
- DPP-4 Inhibitors: Examples include Sitagliptin (Januvia), saxagliptin (Onglyza), linagliptin (Tradjenta, recommended in advanced kidney disease), and alogliptin (Nesina).
- Meglitinides: Examples include repaglinide (Prandin; Gluconorm available in Canada) and nateglinide (Starlix).
- SGLT2 Inhibitors: Examples are canagliflozin (Invokana), dapagliflozin (Farxiga), empagliflozin (Jardiance).
- Sulfonylureas: Examples include glyburide (Micronase, DiaBeta, generics), glipizide (Glucotrol, Glucotrol XL, generics), gliclazide (Diamicron, generics), and glimepiride (Amaryl).
- Thiazolidinediones: Examples include rosiglitazone (Avandia) and pioglitazone (Actos).
- GLP1 Agonists: Types Of Non-Insulin Injected Medicines. This is a relatively new type of medicine used to treat diabetes (incretin mimetics).Examples include liraglutide (Victoza), dulaglutide (Trulicity), semaglutide (Ozempic), exenatide (Bydureon, Byetta). A new oral formulation of semaglutide (rybelsus) has been approved. A novel dual GLP-1 and GIP agonist, sometimes referred to as a twincretin has been approved for both diabetes and obesity management. Tirzepatide (Mounjaro) is a novel twincretin.
Goals For Diabetes Management
Goals of diabetes management should be individualized based upon: age/life expectancy, duration of diabetes, comorbid conditions, hypoglycemic unawareness, history of severe hypoglycemic reactions, pregnancy, and other individual considerations. Depending on the patient, the BLOOD GLUCOSE should be measured 1-3 times per day. The ADA recommends the following blood glucose goals:
- Pre-prandial (before meal): 80-130 mg/dL (4.4-7.2 mmol/L)
- Post-prandial (1-2 hours after a meal): Less than 180 mg/dL (10 mmol/L)
The Glycosylated Hemoglobin (HBA1C OR A1C) provides a good estimate of how well a patient has managed their diabetes during the past 2-3 months. The HbA1C is the primary goal for diabetes management. Depending on the patient, it should be measured 2-4 times a year. With good diabetes management, the HbA1c goes down. With poor management it goes up. In general, the higher the HbA1c, the greater the risk of the long-term diabetic complications.
What is the target level for HbA1c?
- The American Association of Clinical Endocrinologists (AACE) and the American College of Endocrinology (ACE) recommend a level of less than 6.5%.
- The American Diabetes Association (ADA) recommends a goal of less than 7.0% for non-pregnant adults.
- The Canadian Diabetes Associations also recommends a goal of less than 7.0%.
- The United Kingdom NICE guidelines recommend a level of less than 6.5%.
Less stringent HbA1c goals (less than 8%) may be appropriate for:
- Patients at risk of severe hypoglycemia, or
- Who have limited life expectancy, or
- Who already have serious complications from diabetes
Long-Term Complications Of Diabetes Mellitus
- Eye disease (e.g., retinopathy): Diabetes is the leading cause of blindness.
- Heart disease (e.g., coronary heart disease, heart attack)
- Kidney disease (e.g., renal failure, proteinuria)
- Nerve disease (e.g., peripheral and autonomic neuropathy)
- Stroke
Converting Glucose Levels: mg/dl and mmol/l
In the United States glucose is typically measured using the units mg/dl. Nearly every country in the world (including Canada) measures glucose levels using the units mmol/l.
- To convert mmol/L of glucose to mg/dL, multiply by 18.
- To convert mg/dL of glucose to mmol/L, divide by 18 or multiply by 0.055.
Screening For Diabetes
- Hemoglobin A1c: 6.4 (Type 2 Diabetes)
- Fasting Glucose mg/dl: 125 (Type 2 Diabetes)
- Fasting Glucose mmol/l: 6.9 (Type 2 Diabetes)
Hypoglycemia
- Patient with known diabetes mellitus
- Has a low blood sugar (hypoglycemia), defined as a blood glucose < 70 mg/dL (3.9 mmol/dL)
- Has symptoms of low blood sugar
Symptoms of Low Blood Sugar (Hypoglycemia) include:
- Mild hypoglycemia: dizziness, shakiness, weakness, trembling, sweating, headache, nervousness, and hunger. Some patients with mild hypoglycemia experience no symptoms.
- Severe hypoglycemia: unable to speak, confusion, seizures, and coma.
- Hypoglycemic unawareness: Some people with diabetes do not have symptoms of hypoglycemia.
- They can lose consciousness without ever knowing their blood glucose levels were dropping. This condition is mainly seen in adults with long-standing diabetes. These patients need to check their blood glucose more often.
Triage questions for patients with hypoglycemia
- SYMPTOMS: “What symptoms are you concerned about?”
- ONSET: “When did the symptoms start?”
- BLOOD GLUCOSE: “What is your blood glucose level?”
- USUAL RANGE: “What is your blood glucose level usually?” (e.g., usual fasting morning value, usual evening value)
- TYPE 1 or 2: “Do you know what type of diabetes you have?” (e.g., Type 1, Type 2, Gestational; doesn’t know)
- INSULIN: “Do you take insulin?” “What type of insulin(s) do you use? What is the mode of delivery? (syringe, pen; injection or pump) “When did you last give yourself an insulin dose?” (i.e., time or hours/minutes ago) “How much did you give?” (i.e., how many units)
- DIABETES PILLS: “Do you take any pills for your diabetes?”
- OTHER SYMPTOMS: “Do you have any symptoms?” (e.g., fever, frequent urination, difficulty breathing, vomiting)
- LOW BLOOD GLUCOSE TREATMENT: “What have you done so far to treat the low blood glucose level?”
- FOOD: “When did you last eat or drink?”
- ALONE: “Are you alone right now or is someone with you?”
- PREGNANCY: “Is there any chance you are pregnant?” “When was your last menstrual period?”
Practice Guidelines for Hypoglycemia
Types Of Hypoglycemia (Low Blood Sugar)
Hypoglycemia in diabetes can be classified into five types.
- Severe hypoglycemia: This is hypoglycemia that is severe enough that another person must provide treatment (glucose, glucagon).
- Documented symptomatic hypoglycemia: Typical symptoms of hypoglycemia occurring with a measured blood sugar of 70 mg/dL (3.9 mmol/L) or lower.
- Probable symptomatic hypoglycemia: Typical symptoms of hypoglycemia occurring without a measurement of blood sugar level.
- Asymptomatic hypoglycemia: A measured blood sugar of 70 mg/dL (3.9 mmol/L) or lower with no typical symptoms of hypoglycemia.
- Pseudo-hypoglycemia: Patient reports typical symptoms of hypoglycemia but the measured glucose is over 70 mg/dL (3.9 mmol/L).
Causes Of Hypoglycemia
Intensive (tighter) glycemic control reduces the long-term complications of diabetes. Unfortunately, it also increases the frequency of hypoglycemia. There are a number of other factors that can cause or increase the risk of hypoglycemic events.
- Alcohol ingestion
- History of other recent episodes of hypoglycemia
- Prolonged or vigorous exercise
- Renal failure
- Too little food
- Too much diabetes medicine (e.g., insulin, pills)
Treatment with an oral glucose load
if blood glucose < 70 mg/dl (3.9 mmol/l) or unknown, for a person who is conscious, able to follow commands, and able to swallow:
- Give sugar (15-20 grams glucose) by mouth.
- Each of the following has the right amount of sugar: glucose tablets (3-4 tablets; 15-20 grams); glucose gel (15-20 grams); fruit juice or non-diet soda (1/2 cup; 120 ml); milk (1 cup; 240 ml);pre-packaged juice box (1 box); Skittles candy (15); table sugar or honey (3 teaspoons; 15 ml).
- Symptoms should begin to improve within 5-10 minutes. It may take 15-20 minutes for symptoms to go away completely.
- Repeat if not better within 15-20 minutes.
Glucagon Administration
If blood glucose < 70 mg/dl (3.9 mmol/l) or unknown (pending ems arrival). Glucagon is preferred if patient is unconscious or unable to swallow:
- If family has glucagon for hypoglycemic emergencies AND the caller knows how to use it, instruct the caller to give the glucagon now. Inject it IM into the upper outer thigh.
- Adult dosage is 1 mg.
- Glucagon can be used in unconscious patients.
- Symptoms should begin to improve within 5-10 minutes. It may take 15-20 minutes for symptoms to go away completely.
Kindly Let Us Know If This Was helpful? Thank You!


