Diabetes is a chronic condition affecting the body’s ability to process glucose (the primary fuel source for cells in the human body). It can be caused by autoimmunity (where the body attacks the cells that make insulin), genetics, medications, and obesity. Diabetes medications are meant to help lower blood sugar levels by making your body more sensitive to insulin or increasing insulin production.
Because there are no cures for type 1 and type 2 diabetes yet—and because there are many different types of medications available that treat various aspects of these conditions—it’s easy to get overwhelmed by all the choices out there. And while they all work differently on an individual level, they all serve one core purpose: lowering blood sugar levels so that you can maintain proper health without experiencing symptoms (like thirstiness and frequent urination) or developing complications.
Most medications for diabetes mellitus are acceptable for treating various forms of diabetes except type 1 diabetes. For patients with type 1 diabetes (autoimmune destruction of the cells in the pancreas that make insulin), insulin is the preferred treatment choice.
Various defects result in type 2 diabetes mellitus. Our knowledge of these defects has improved significantly – see the triumvirate, ominous octet, and egregious eleven of type 2 diabetes mellitus.
How does metformin work?
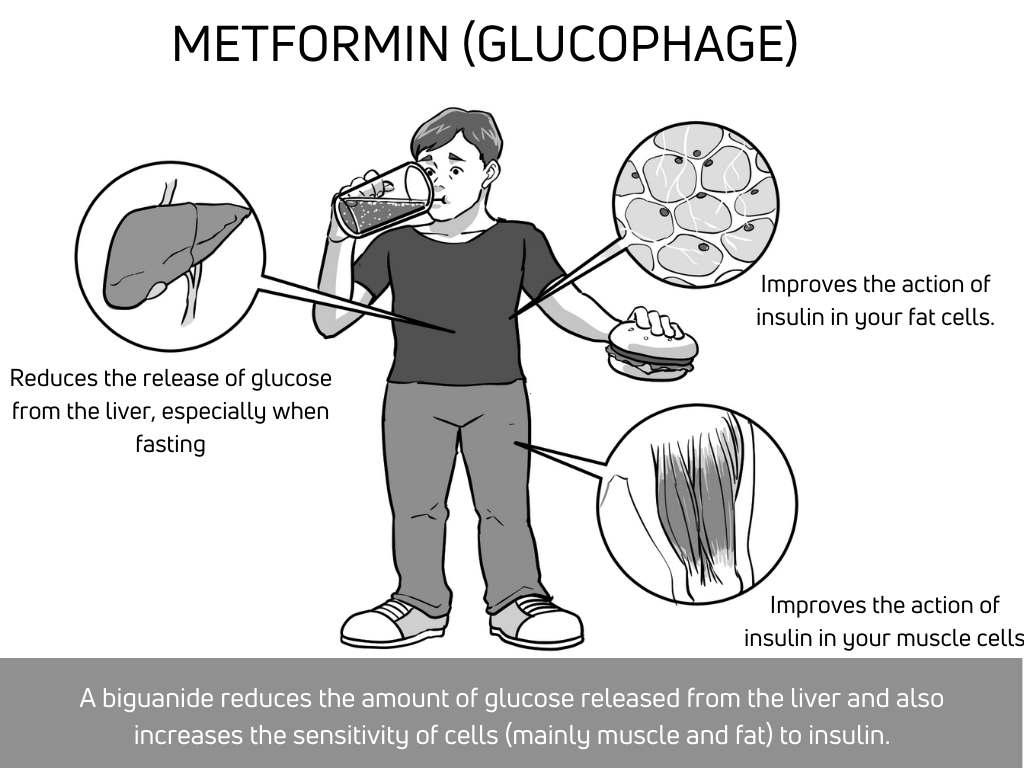
Metformin (brand name Glucophage) is a biguanide drug that reduces the amount of glucose released from the liver and increases the sensitivity of cells (mainly muscle and fat) to insulin. Metformin lowers blood sugar levels by making your body more sensitive to insulin. It also helps lower blood sugar levels by decreasing how much glucose your liver produces after eating.
Your liver makes some glucose when you eat, but more importantly, it releases even more glucose when fasting. This accounts for your blood sugars being high in the morning, even after going to bed with an acceptable glucose.
It is worth noting that a significant stress hormone (cortisol) released by your adrenal glands (pyramidal-shaped glands on top of each kidney) around 4 am. This stress hormone talks to the liver and causes it to squeeze out a lot of glucose into the blood. This is known as the “dawn phenomenon”. Insulin is a hormone that works opposite to that of cortisol. Insulin talks to the liver and prevents it from changing glycogen (a storage form of glucose) directly into glucose (a major fuel source). In patients with type 2 diabetes, there is resistance to the action of insulin at the level of the liver. As such, although insulin levels may be high, it is unable to reduce the release of glucose by the liver to an appreciable extent.
Fun Fact :
Metformin, a drug that is currently used to treat diabetes, has actually been around since the Middle Ages. People in ancient times used lilac flowers to treat people with diabetes mellitus. The plant was thought to be effective because it seemed to improve glucose levels in the blood of some patients. The French lilac plant (Syringa vulgaris) is an easy-to-grow, adaptable shrub that produces gorgeous purple flowers. The plant is a member of the lily family—in fact, it’s one of the most popular flowering plants in Europe!
How does Januvia work?
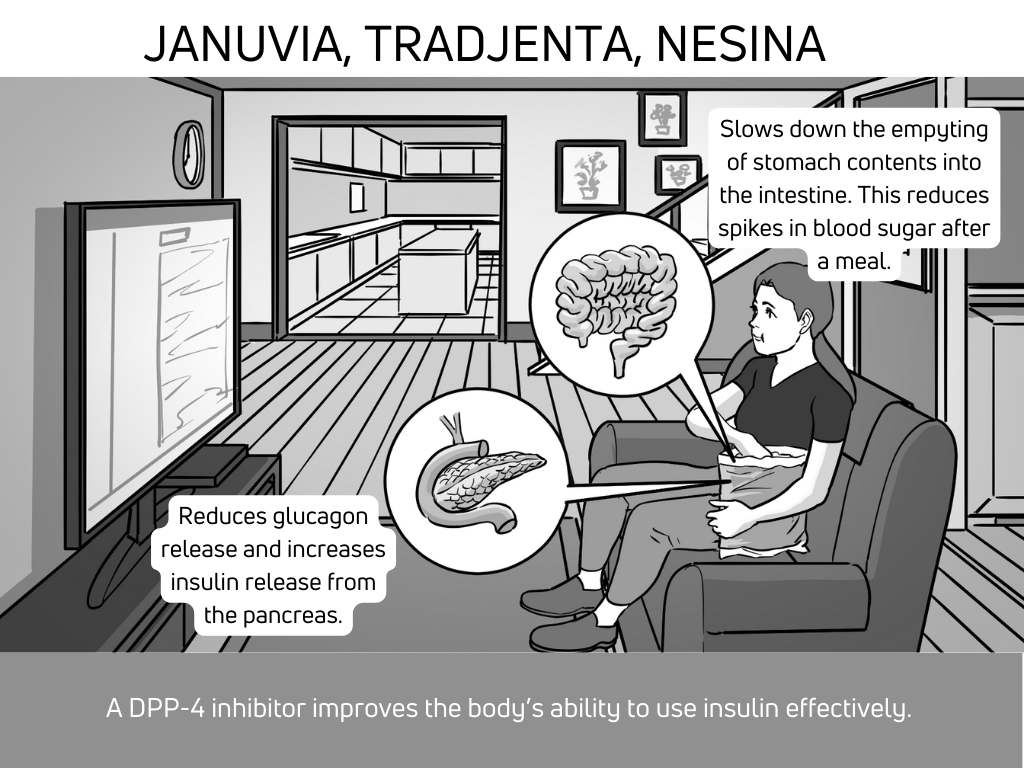
Januvia (sitagliptin) belongs to a group of diabetes medications are known as DPP4 inhibitors. Other medications in this class are Tradjenta (linagliptin), Saxagliptin, and alogliptin. It is a pill that improves the body’s ability to use insulin effectively. It also works by slowing down the absorption of food from the small intestine which helps in reducing spikes in your blood sugar after a carbohydrate meal.
How do Ozempic, Trulicity, and Victoza work?
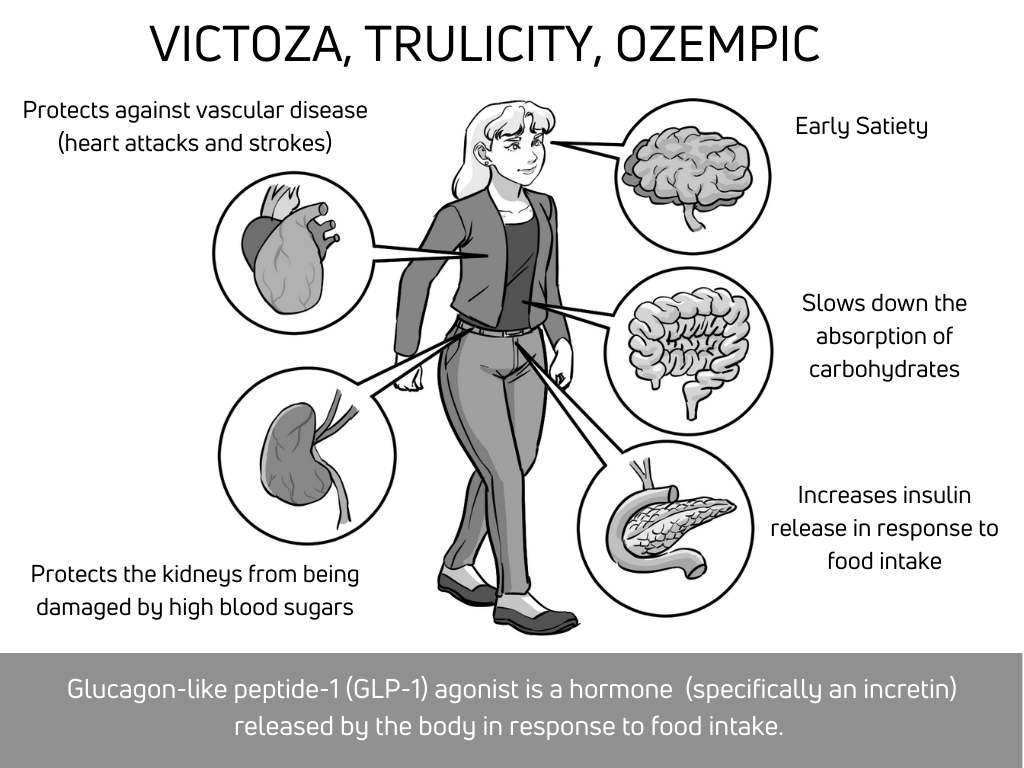
Glucagon-like peptide-1 (GLP-1) is a hormone that helps to control blood sugar levels. It’s a type of incretin, which is a hormone released by the body in response to food. There are various drugs in this class of diabetes medications known as GLP-1 agonists. These include, Ozempic (semaglutide), Trulicity (Dulaglutide), Victoza (Liraglutide), and Bydureon (Exenatide). GLP-1 agonists work by reducing blood glucose levels after eating and slowing down the rate at which food is digested.
- Stimulates the pancreas to release insulin after a meal (this is known as glucose-dependent insulin release or the incretin effect)
- It binds to a unique receptor in the brain, which makes one feel full after eating very small meals (anorexigenic effect)
- It increases the transit time (slows down the absorption) of carbohydrate-based foods, reducing spikes in blood glucose.
- There is recent evidence that various drugs in this class of medications protect against heart attacks and strokes, especially in patients with a known history of these conditions. It will be challenging to finance a clinical trial to prove that these drugs prevent strokes and heart attacks in patients without known cardiovascular disease. This is because the larger population of people living with diabetes mellitus will be unlikely to develop these complications during the follow-up of an expensive clinical trial (usually lasting between 1-3 years).
- Some of these medications have been found to be renoprotective (protects the kidneys from the effects of diabetes).
Fun fact :
During an investigation into the properties of the venom of a Gila monster, Heloderma suspectum, scientists stumbled upon a 39-amino acid peptide called exendin-4. Over 50% of this peptide looks exactly like glucagon-like peptide 1 (GLP-1). The prototype drug known as exenatide was first introduced on the market in 2005.
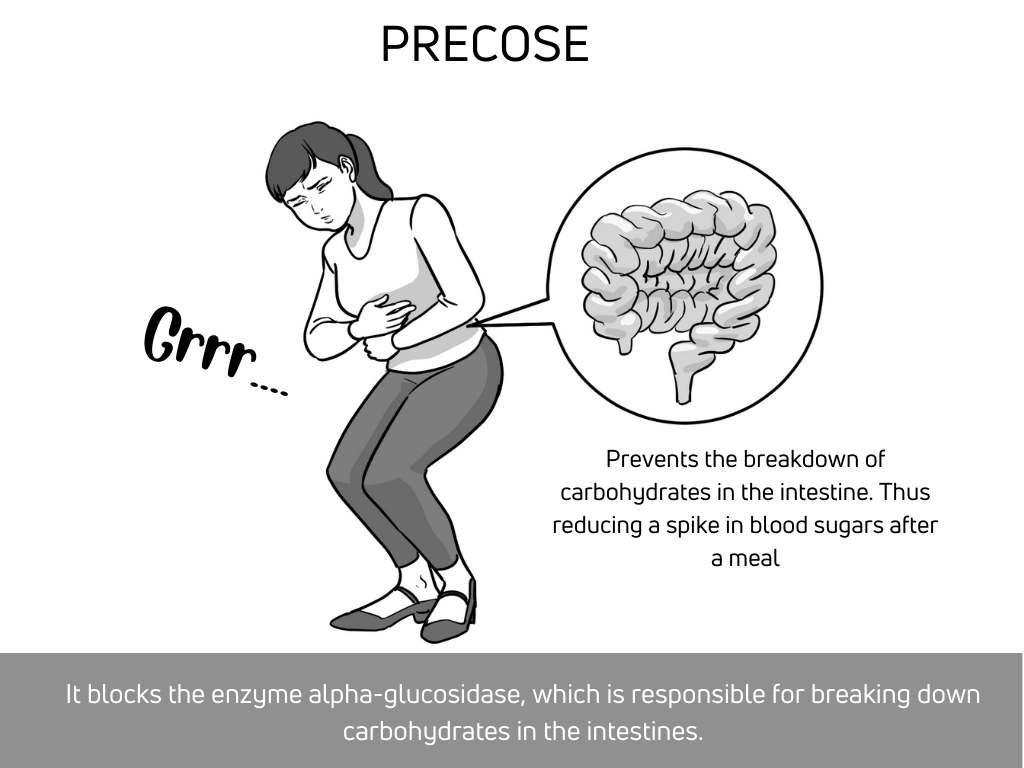
How does Acarbose work?
Acarbose is a drug that slows the digestion of carbohydrates. It works by blocking the enzyme alpha-glucosidase, which is responsible for breaking down carbohydrates. It can be used as an adjunct to other diabetes medications and can be helpful in people who have had poor control of other medications. It has a somewhat mild effect on diabetes control. Even more importantly, it has poor acceptance amongst patients due to its association with bloating, abdominal discomfort, and diarrhea.
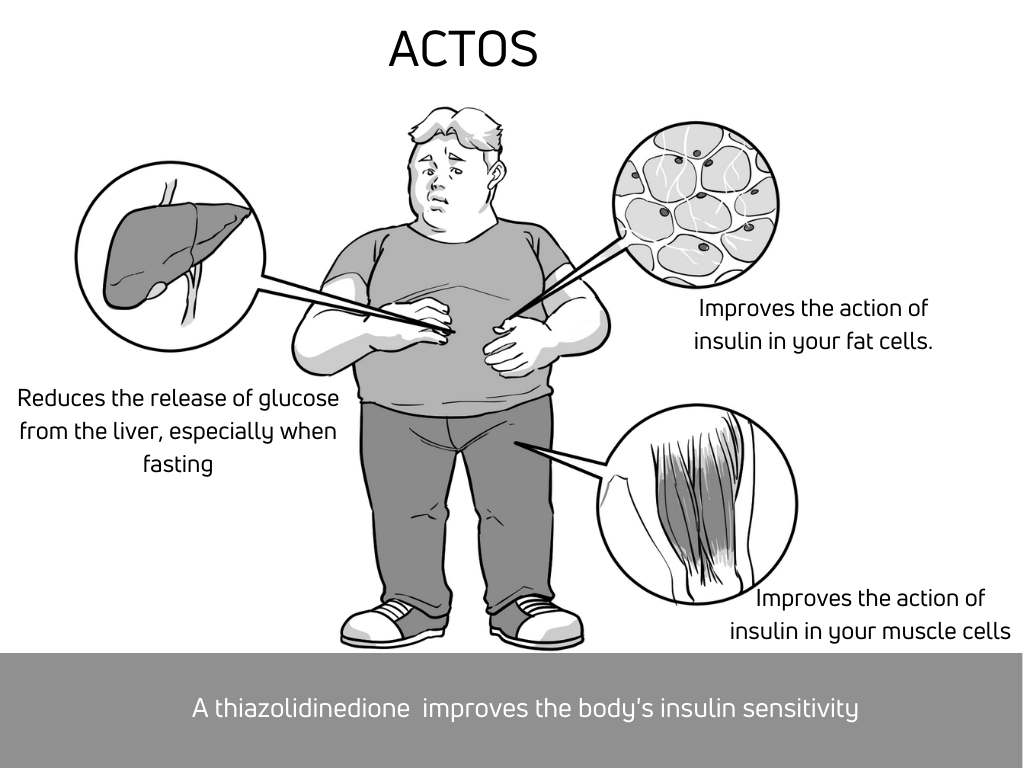
How does Actos work?
Actos (pioglitazone) belongs to a group of medications known as thiazolidinediones. Another drug in this class of medications is Avandia (rosiglitazone) which was discontinued due to cardiovascular safety effects. Actos works by helping your body use insulin more effectively. It also makes your body more sensitive to insulin action, so you need less insulin to control your blood glucose.
Actos is associated with weight gain, especially at higher doses (30 to 45mg a day). The 15mg dose of pioglitazone is less likely to cause fluid retention or significant weight gain. It is however not recommended in patients with a history of congestive heart failure.
Additional safety concerns with pioglitazone
- Causes the loss of bone mass (osteoporosis)
- Fluid retention and exacerbation of known congestive heart failure
- Slight but statistically significant increase in the risk of bladder cancer
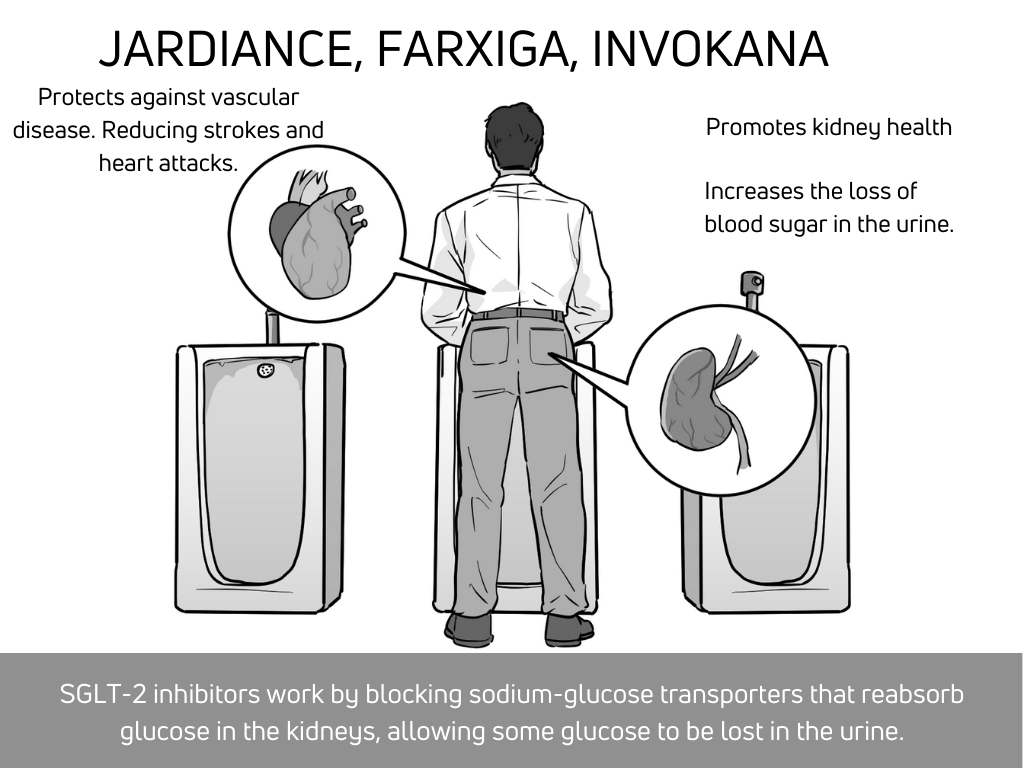
How does Jardiance work?
SGLT-2 inhibitors work by blocking a protein (sodium-glucose transporters) that reabsorbs glucose in the kidneys, allowing some glucose to be lost in the urine. Jardiance (empagliflozin), farxiga (dapagliflozin), and invokana (canagliflozin) belong to this class of medications known as SGLT-2 inhibitors.
Side effects include increased urinary tract infections, low blood pressure, and genital yeast infections. It is generally recommended that you maintain oral hydration when on this class of drugs for diabetes. Just like GLP-1 agonists, there is recent evidence that various drugs in this class of medications protect against heart attacks and strokes, especially in patients with a known history of these conditions.
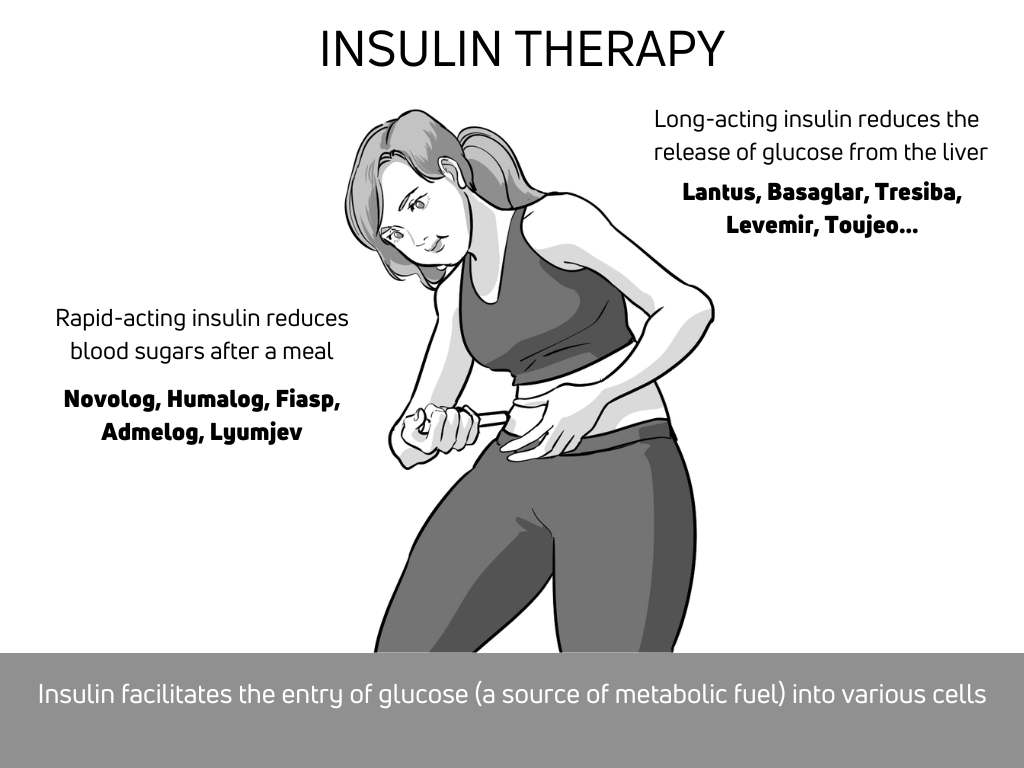
How does insulin work?
Insulin is a hormone that’s produced in the pancreas, a gland near your stomach. When you eat, insulin helps move sugar from your blood into your cells to be used as energy or stored for later use. When you have diabetes, either your body doesn’t make enough insulin (type 1 diabetes mellitus), or it can’t respond to its effects properly (a condition called insulin resistance).
How does long-lasting insulin work?
Long-acting insulin is a basal insulin, meaning it’s not given in response to meals. It’s used for type 1 diabetes and some type 2 diabetes patients who have difficulty controlling their blood glucose levels. Long-acting insulin can be injected once a day or twice a day. It lasts for 24 hours and works slowly over that period of time to control blood glucose levels as they rise during periods of fasting (basal insulin action). Long-lasting insulin prevents significant spikes in your morning blood sugar (see the dawn phenomenon described earlier in this post). It should therefore be taken even if you are not eating (the dose may sometimes be adjusted downwards if you are fasting for extended periods).
| Type of Long acting insulin | Pens per pack | Units per pen | mL per pen | Days until expiration at room temperature |
|---|---|---|---|---|
| Lantus Solostar | 5 pens | 300 units | 3mL | 30 days |
| Levemir Flextouch | 5 pens | 300 units | 3mL | 42 days |
| Toujeo Solostar – 1u increments (Up to 80 units) | 3 or 5 pens / pack | 450 units | 1.5mL | 42 days |
| Tresiba Flextouch | 5 pens for U100 | 300 units | 3mL | 56 days |
| Tresiba Flextouch (U200 pen in 2u increments up to 160units) | 3 pens for U200 | 600 units | 3mL | 56 days |
| Basaglar | 5 pens | 300 units | 3mL | 28 days |
How does rapid-acting insulin work?
- It is taken before meals to prevent blood glucose levels from rising too high after eating.
- Rapid-acting insulin starts working in 20 minutes, peaks in 1.5 hours, and lasts 3-5 hours. This means that you need to take it every day, before each meal or snack.
| Meal time insulin | Pens per pack | units per pen | ml per pen | days until expiration at room temperature |
|---|---|---|---|---|
| Apidra Solostar | 5 pens | 300 units | 3mL | 28 days |
| Humalog U100 Kwikpen | 5 pens | 300 units | 3mL | 28 days |
| Humalog U200 Kwikpen | 2 pens | 600 units | 3mL | 28 days |
| Novolog Flexpen | 5 pens | 300 units | 3mL | 28 days |
| Humulin R U500 Kwikpen (5u increments up to 300units) | 2 or 5 pens / pack | 1,500 units | 3mL | 28 days |
| FIASP Flextouch | 5 pens | 300 units | 3 mL | 28 days |
How does Symlin work?
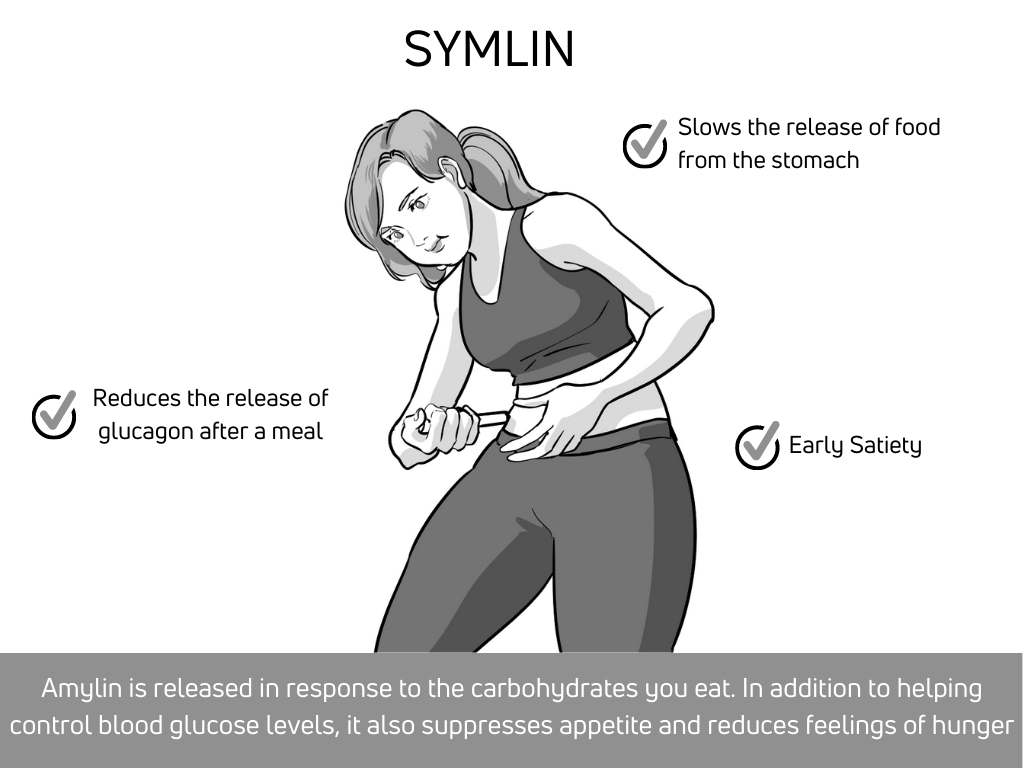
This drug works by mimicking the properties of amylin, a hormone from the pancreas that helps regulate how your body digests food. When you eat, amylin is released in response to the carbohydrates you eat. In addition to helping control blood glucose levels, it also suppresses appetite and reduces feelings of hunger
When taken as part of a diabetes treatment plan along with insulin therapy or other medications, Symlin can help improve blood glucose control by reducing spikes in blood sugar after a meal. Symlin helps to reduce significant glycemic spikes in patients with type 1 diabetes mellitus. Being a peptide hormone, amylin is only available via the subcutaneous route (skin injection). This means that the typical type 1 diabetes patient would be taking at least two separate injections at each meal. This is a significant limitation to the use of Symlin in diabetes patients.
Conclusion
You can see how there are many different types of diabetes drugs. But all these drugs work in a similar way, by either increasing the amount of insulin released by the pancreas or decreasing sugar absorption. They also all act quickly to help control blood glucose levels.
The opinions expressed here represent the views of a practicing hormone specialist (endocrinologist) and must not substitute the advice of your health care provider. This blog post is written for a non-medical audience interested in learning more about hormonal disorders. The author has no commercial conflicts of interest to declare. Also, read our privacy policy.
Kindly Let Us Know If This Was helpful? Thank You!


