There are many old and novel anti-diabetes medications due to our increasing understanding of the pathophysiologic basis of mainly type 2 diabetes mellitus. The three core pathophysiologic perturbations were first highlighted by deFronzo in the triumvirate, and this has since evolved into the ominous octet (8 defects) and, more recently, egregious eleven (11 defects). This represents are significant deviation from a insulin-centric approach to managing diabetes mellitus. There is more to the disease than insulin resistance or insulin deficiency. A simple mnemonic for recalling the groups of medications in diabetes pharmacotherapy. You first sense a bowel movement, squeeze to evacuate the bowel, and flush.
A simple mnemonic for diabetes drugs. Sense, Squeeze, and Flush! A complete list of infographics is available at the end of this article.
Sensitizing
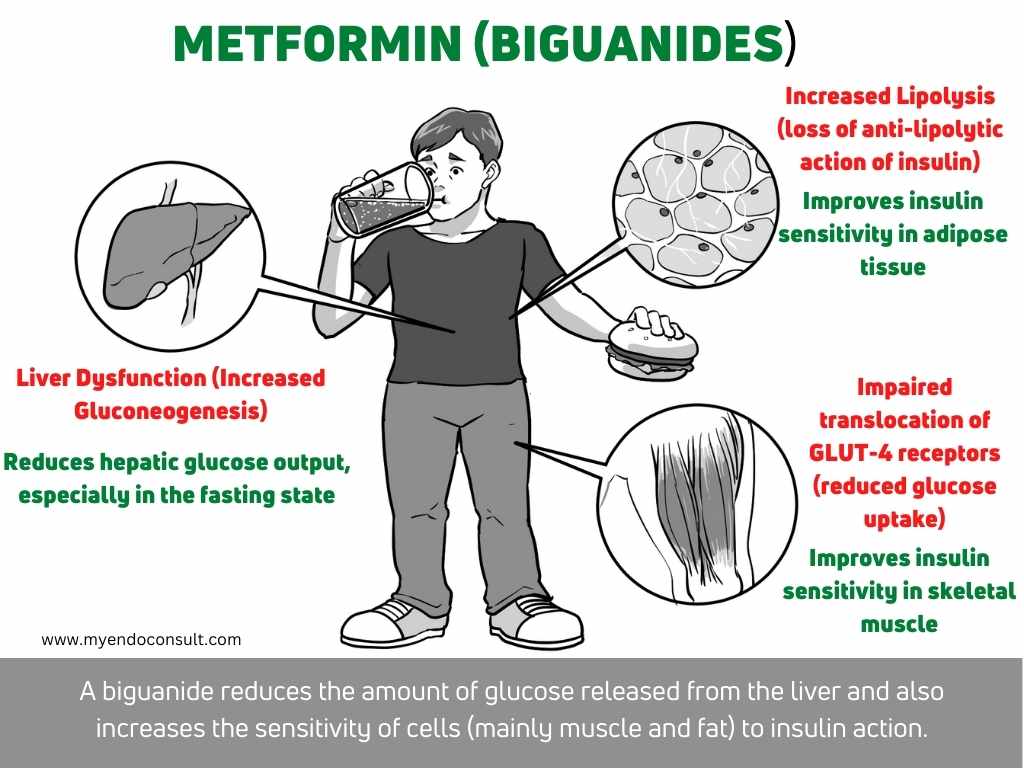
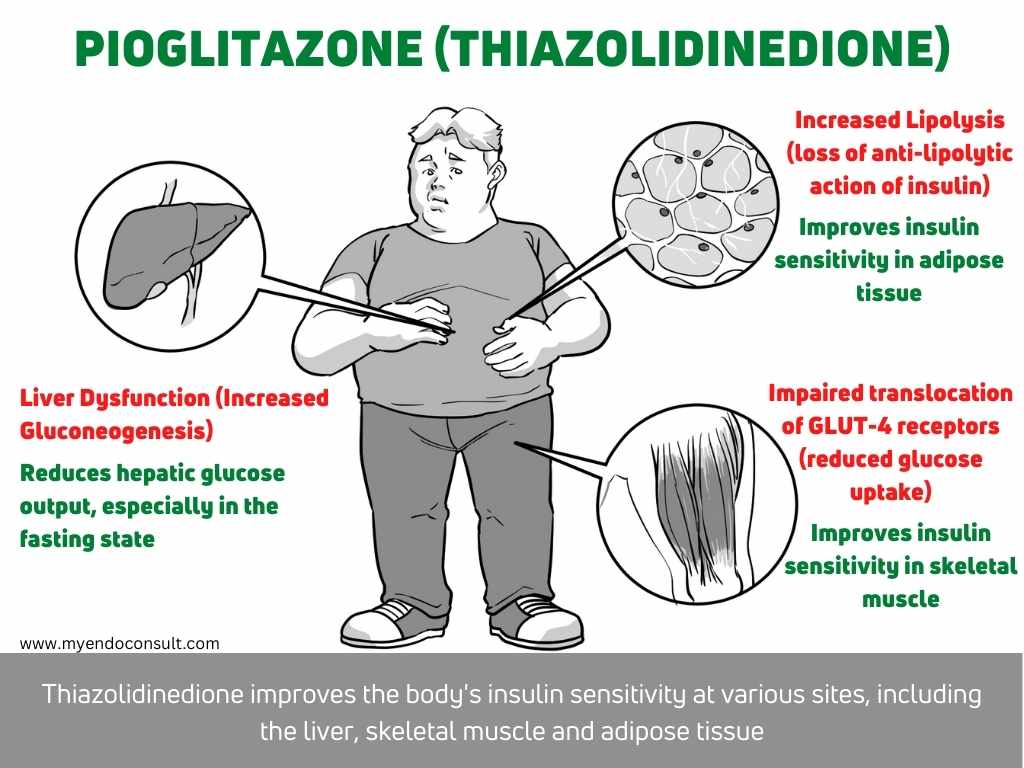
Metformin, Pioglitazone, and Dopaminergic agonist (bromocriptine)
Metformin by activating the AMP-kinase pathway, reduces hepatic glucose production. It also increases insulin sensitivity(1).
- Pioglitazone activates nuclear transcription factor PPAR-gamma and improves insulin sensitivity.
- Dopaminergic agonists (bromocriptine) improve insulin sensitivity.
Squeezing
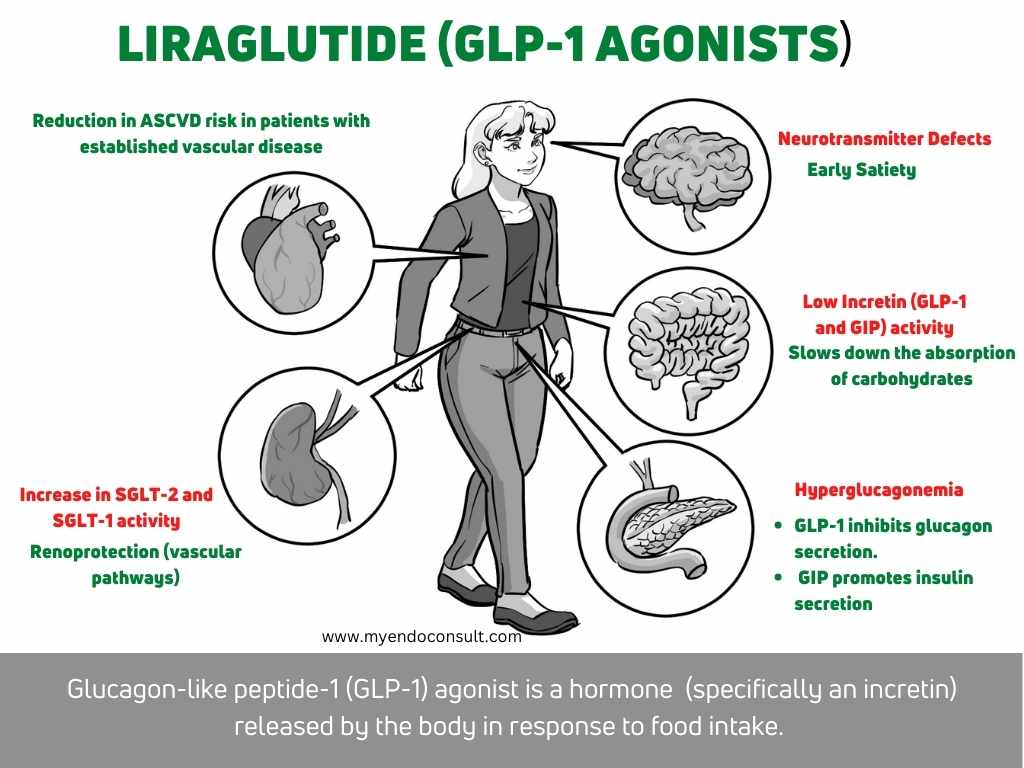
Sulfonylureas and Meglitinides (directly increase insulin secretion), GLP-1, Dual GLP-1 and DPP-4 inhibitors (incretin pathway), and Bile Acid sequestrants (increase incretin levels).
Sulfonylureas (glyburide, glipizide and glimepiride) and meglitinides (repaglinide and nateglinide) close potassium-ATP channels on the plasma membrane of beta cells, which induces the secretion of insulin (review the mechanism here).
Incretin mimetics (GLP-1 and dual GIP-GLP1 agonists) activate GLP-1 receptors and produce the following effects
- Glucose-dependent insulin secretion (insulin is released only after meal intake)
- Reduction in glucagon release (after meal intake)
- Reduces gastric emptying, reducing a rise in blood sugar after a meal.
- Increased satiety and weight loss
DPP4 inhibitors (sitagliptin, alogliptin, linagliptin, saxagliptin) inhibit the activity of dipeptidyl peptidase, thus increasing postprandial concentrations of incretins (GIP and GLP-1). These agents also reduce the release of glucagon.
The proposed mechanism of action of bile acid sequestrants (colesevelam)
- Binds bile acids in the intestine and increases hepatic bile acid release. This ultimately reduces hepatic glucose production.
- Increases incretin levels
Flushing
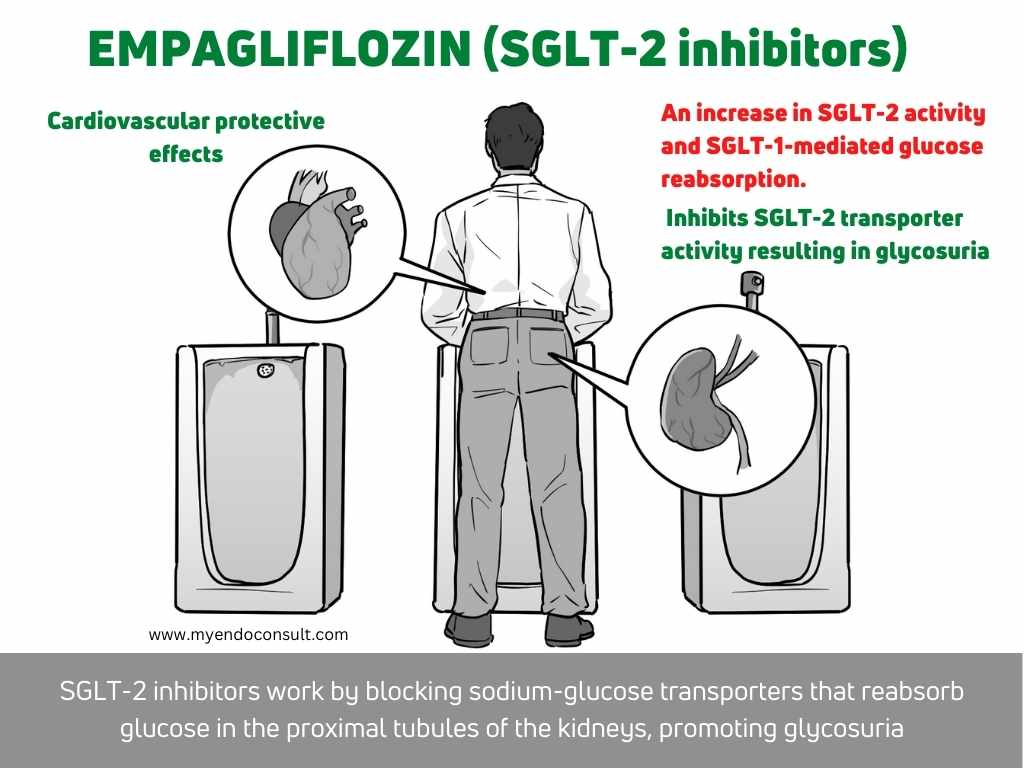
Alpha-glucosidase inhibitors and SGLT-2 inhibitors.
Flushing of glucose via the urinary system (peeing) or the gastrointestinal system (pooing). Intestinal alpha-glucosidase is required for the breakdown of gastrointestinal carbohydrates. Inhibitors of this enzyme include acarbose and miglitol.
Sodium-Glucose Transporter 2 channels in the proximal nephron are required for glucose reabsorption. SGLT-2 inhibitors (canagliflozin, dapagliflozin, and empagliflozin) promote glycosuria(2).
References
- Konopka AR, Esponda RR, Robinson MM, Johnson ML, Carter RE, Schiavon M, et al. Hyperglucagonemia Mitigates the Effect of Metformin on Glucose Production in Prediabetes. Cell Rep. 2016 May 17;15(7):1394–400.
- Marín-Peñalver JJ, Martín-Timón I, Sevillano-Collantes C, del Cañizo-Gómez FJ. Update on the treatment of type 2 diabetes mellitus. World J Diabetes. 2016 Sep 15;7(17):354–95.
Kindly Let Us Know If This Was helpful? Thank You!


