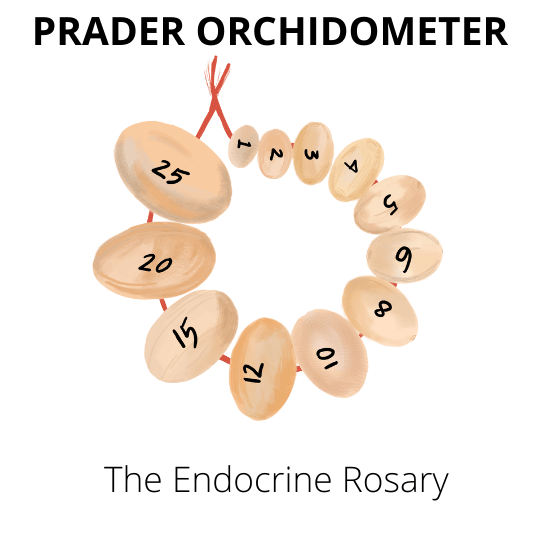
A Prader orchidometer (sometimes referred to as the endocrine rosary) is a medical instrument used to measure the size of an individual’s testicles.
It is named after Swiss physician Adolf Prader, who developed the device in the 1960s. It consists of a series of ellipsoid beads graduated according to close estimates of testicular volume.
Introduction
The testes are primarily responsible for the production of testosterone and spermatozoa, with most of their volume being germ cells and seminiferous tubules. Studies in males with infertility have shown that testicular volume measured either by ultrasonography or an orchidometer (low cost tool) correlates with testosterone levels and optimal seminal fluid parameters.
The hypothalamic-Pituitary-Testicular axis
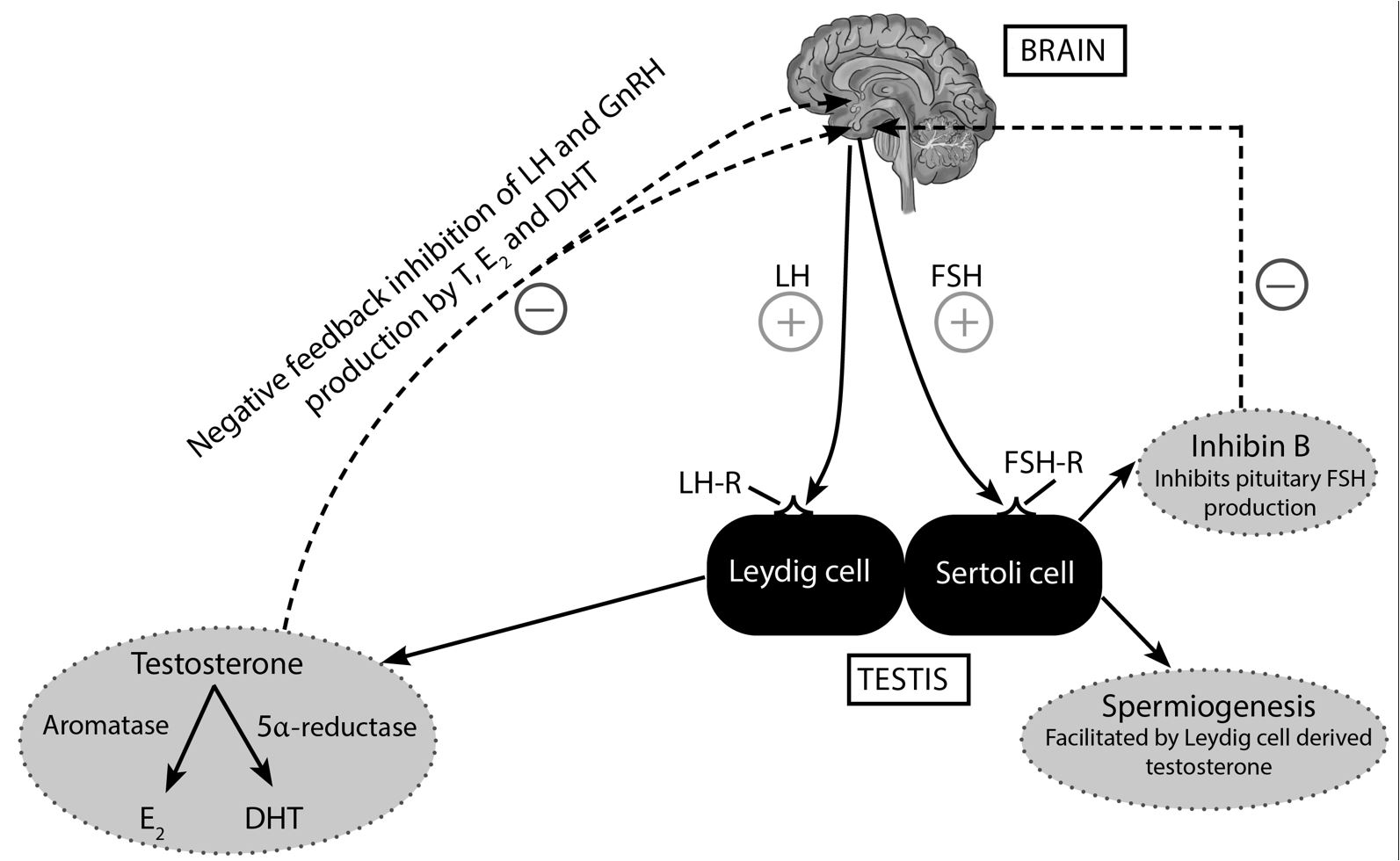
Gonadotropin-releasing hormone (GnRH) produced from the hypothalamus stimulates pituitary gonadotrophs to produce gonadotropins (FSH and LH).
Luteinizing hormone (LH) binds to its cognate G-protein coupled LH receptor (LH-R) on the Leydig cell and subsequently stimulates the production of testosterone [1].
Subsequently, testosterone (T) is converted to estradiol and dihydrotestosterone (DHT) by peripheral aromatase (enzyme) and 5ɑ reductase enzymes, respectively (solid lines) [2]. Also, negative feedback inhibition of both pituitary gonadotrophs and hypothalamic GnRH neurons is mediated by testosterone and estradiol (E2) (broken lines) [3].
Also, Follicle-stimulating hormone (FSH) binds to its corresponding G-protein coupled FSH receptor (FSH-R) on the Sertoli cell of the testis. This action promotes the formation of spermatozoa (spermatogenesis), androgen-binding proteins (ABPs), and inhibin B (solid lines).
It is worth noting; however, that sustained spermatogenesis in the Sertoli cell requires the presence of intratesticular testosterone (Leydig cell-derived testosterone) [4]. Finally, inhibin B suppresses FSH release via a negative feedback loop (broken lines) [5].
Testicular volume measurement
The orchidometer consists of a series of 12 graduated beads that range in size from 1 to 25 milliliters (ml). Testicular volume assessment using an orchidometer allows objective measurement of testicular size. The beads are graded by volume, starting at 1 to 3ml for prepubertal testicles, 4 to 12 ml for puberty, and 15 to 25ml for adult-sized testicles.
The examiner places the largest-sized bead next to each testicle. Scrotal skin should be taut over the testicle being measured. If the testicle does not match, the next largest sphere is placed until a fit is found. The sizes of the two testicles are then compared and recorded.
Considerable tact and excellent reassurance skills and bedside manners are important during testicular volume measurement. Ultimately, the patient should never be made to feel inadequate as a man during this physical examination.
The orchidometer is used in a variety of settings, including clinical examinations, research studies, and fertility evaluations. While the Prader orchidometer is a simple and effective tool, it is essential to note that testicular size can vary significantly from individual to individual. As such, the orchidometer should not be used as the sole means of assessing testicular health.
Orchidometer versus ultrasound
What is the best tool for assessing true testicular volume? There is no definitive answer to this question as both methods have advantages and disadvantages. Ultrasounds are generally considered to be more accurate, but they can be more expensive and require special training to use correctly.
Orchidometers may be less accurate, but it is less expensive and easier to use. Ultimately, the best method for measuring testicular volume will depend on the individual clinical situation and preference of the clinician.
Pathophysiology of low testicular volume in hypogonadism
As previously mentioned, testicular size is a good surrogate marker of spermiogenesis potential. Also, Leydig cells do not contribute substantially to the final testicular volume; therefore, a disruption in seminiferous tubule function will result in a significant decline in testicular size independent of Leydig cell function [6].
FSH and intra-testicular testosterone promote the development of Sertoli cells, which are present on the epithelial cells of the seminiferous tubules. LH, on the other hand, stimulates the Leydig cells of the testes, which are responsible for the synthesis of testosterone [7].
In the setting of male hypogonadism, low levels of intratesticular testosterone result in less trophic stimulation of the Sertoli cells, leading to their eventual atrophy. This accounts for the low testicular volume seen in patients with male hypogonadism [4].
What is a normal testicle size
- 4 to 5.5 cm in length x 2.5cm in width x 3cm in the anteroposterior dimension.
- The volume is reported as being greater than 20ml in whites and African Americans [8]. The assessment of testicular volume requires the use of an orchidometer – sequential beads labeled with an estimated testicular volume.
- Palpation and inspection of the testes facilitates an approximation of testicular volume by comparing it to the beads on the orchidometer.
Recommended Orchidometer for Endocrinologists
The endocrine society has highly discounted low-cost Prader orchidometers for trainees. The orchidometer is made of a sturdy and hygienic wooden material strung along a firm chord. The tool has a drawstring bag allowing for simple storage in your waist pocket. Get one here! Also, an alternative orchidometer from Amazon.com is available here if you are not a member of the Endocrine society (affiliate link).
References
1. Shalet SM. Normal testicular function and spermatogenesis. Pediatr Blood Cancer. 2009;53(2):285-288. doi:10.1002/pbc.22000
2. Stocco C. Tissue Physiology and Pathology of Aromatase. Steroids. 2012;77(1-2):27-35. doi:10.1016/j.steroids.2011.10.013
3. Vaucher L, Funaro MG, Mehta A, et al. Activation of GPER-1 estradiol receptor downregulates production of testosterone in isolated rat Leydig cells and adult human testis. PloS One. 2014;9(4):e92425. doi:10.1371/journal.pone.0092425
4. Griswold MD. The central role of Sertoli cells in spermatogenesis. Semin Cell Dev Biol. 1998;9(4):411-416. doi:10.1006/scdb.1998.0203
5. Demyashkin GA. Inhibin B in seminiferous tubules of human testes in normal spermatogenesis and in idiopathic infertility. Syst Biol Reprod Med. 2019;65(1):20-28. doi:10.1080/19396368.2018.1478470
6. Handelsman DJ, Staraj S. Testicular Size: The Effects of Aging, Malnutrition, and Illness. J Androl. 1985;6(3):144-151. doi:10.1002/j.1939-4640.1985.tb00830.x
7. Barrionuevo F, Burgos M, Jiménez R. Origin and function of embryonic Sertoli cells. Biomol Concepts. 2011;2(6):537-547. doi:10.1515/BMC.2011.044
8. Lin CC, Huang WJS, Chen KK. Measurement of Testicular Volume in Smaller Testes: How Accurate Is the Conventional Orchidometer? J Androl. 2009;30(6):685-689. doi:10.2164/jandrol.108.006460
Kindly Let Us Know If This Was helpful? Thank You!
Last update on 2024-07-25 at 00:55 / Affiliate links / Images from Amazon Product Advertising API


