Enlargement of the thyroid gland due to any cause is called a goiter. A normal thyroid is not palpable. To be clinically discernible, a goiter has to weigh a minimum of 40grams in size. A goiter may be present in the setting of low, normal or high thyroid hormone output.
- Normal thyroid hormonal function(referred to as euthyroidism).
- Increased thyroid hormonal function (hyperthyroidism). Which may be due to either Toxic nodules or a diffuse goiter (Graves/Basedow’s disease)
- Decreased or absent thyroid hormonal function (hypothyroidism) due to Hashimoto’s thyroiditis or significant iodine deficiency.
How are Goiters Classified in practice?
- Simple (non-toxic) Goiter. This occurs in the setting of diffuse colloidal enlargement or hyperplasia.
- Toxic Goiter. Diffuse toxic goiter (also known as Grave’s or Basedow’s disease).
- Toxic nodular disease. Toxic nodular goiter of varying degrees. Solitary toxic nodule or Toxic multinodular goiter (also known as Plummer’s disease)
- Toxic malignant tumor. Thyroid cancer, on very rare occasions, may present with overt hyperthyroidism.
- Neoplastic Goiter. Neoplastic goiters may be benign or malignant. Fine needle aspiration biopsy is required in patients with high-risk nodules.
- Goiter of inflammatory etiology. Auto-immune thyroiditis (Hashimoto’s disease) and various types of transient inflammatory states, e.g., painless thyroiditis, postpartum thyroiditis, etc.
- Acute suppurative thyroiditis is usually of bacterial etiology. Antibiotic courses and intravenous hydration are required.
- Subacute thyroiditis (De Quervain’s thyroiditis).
- Riedel’s thyroiditis is characterized by a hard thyroid gland attached tenaciously to surrounding cervical tissues.
- Granulomatous thyroiditis is seen in the setting of tuberculosis.
A simple goiter is a noncancerous growth of the thyroid in the setting of normal thyroid function. It tends to occur sporadically in the general population.
A deficiency in the production of thyroid hormone due to either impaired synthesis or release promotes the release of stimulating thyroid hormone by the anterior pituitary gland. Interestingly insufficiency of thyroid hormone may be due to not only pathological conditions but physiologic ones as well.
Lack of thyroid hormone production
A state of Relative Physiological Deficiency occurs in some physiological states, such as the pubertal growth spurt, pregnancy, and postpartum periods. For example, during pregnancy, there is increased thyroxine binding globulin which binds active thyroid hormone, further reducing its plasma concentrations. Consequently, this is sensed by thyrotrophs in the anterior pituitary gland, which then release TSH. Hyperstimulation of thyroid follicular cells by high levels of TSH accounts for the onset of physiological goitrous states. Indeed, it has been postulated that intermittent exposure of the thyroid gland to high levels of TSH during the monthly menstrual cycle and possibly pregnancy accounts for the disproportionately higher incidence of goiter in women than men.
Pathological insufficiency of thyroid hormone
Iodine is a critical component of thyroid hormone. Its role in thyroid hormone synthesis may be negatively impacted by factors that modulate iodine absorption, intracellular transport, or incorporation in thyroid hormone.
The concentration of iodine in the diet or water may be inadequate in setting geographical areas. In areas with endemic goiters, such as mountainous regions, there is a loss of iodine in the topsoil. Furthermore, soils rich in limestone are laden with calcium (a mineral that exerts a goitrogenic effect). Some foods, such as cassava, contain goitrogens (cassava contains agents that can be converted into perchlorate-like compounds which inhibit thyroid hormone synthesis). Also, impaired gastrointestinal absorption of iodine or increased renal losses of iodine reduces “iodine reserve.”
Processes involved in iodine uptake (sodium iodine symporters), intrafollicular trapping and concentration of iodine can be impaired by various agents containing the ions perchlorate, pertechtenate, thiocyanate or nitrates. Historically relevant drugs which are seldom used now such as tolbutamide and chlorpropamide reduce the release of thyroid hormone.
Congenital deficiency of various enzymes necessary for oxidizing iodine (thyroid peroxidase enzyme), coupling of iodine and tyrosine, and releasing thyroid hormone contributes to overt hypothyroidism.
When the thyroid gland is exposed to excessive amounts of iodine, this insult may paradoxically interfere with the absorption, organification, and oxidation steps in thyroid hormone synthesis. This pathophysiologic phenomenon of excess iodine acutely blocking the binding of iodine to tyrosyl residues on thyroglobulin is referred to as the classic Wolff-Choikoff’s block or effect.
Clinical features
Simple nodular goiter may occur in any age group and presents as “anterior neck swelling which moves on swallowing.” Ultimately, its size may produce significant concerns for patients who may wish to have it extirpated for social reasons. Depending on the degree of tumorous growth of the thyroid gland, it may produce a myriad of compressive neck symptoms. These include hoarseness of voice, snoring, Horner’s syndrome, facial flushing (Pemberton’s sign), difficulty in swallowing and difficulty in breathing (structural compression of the trachea or diaphragmatic paresis).
On inspection, the skin over the goitrous gland may be stretched, thin, and shiny with prominent overlying superficial veins. A practical clinical pearl of obstructed venous return in the setting of a retrosternal goiter is exemplified by the presence of manubrial subcutaneous veins. Patients with retrosternal goiters can present with Horner’s syndrome, diaphragmatic paresis, and vocal cord paresis.
A simple nodular goiter may feel soft and cystic or firm, depending on the nature of the nodule. For patients with diffuse toxic goiter (Graves disease), a bruit may be appreciated over the superior poles of the thyroid gland (hyperdynamic flow in the superior thyroid arteries).
WHO Classification of Goiter
- Grade 1: Goiter is palpable.
la: Goiter is palpable but not visible on inspection even upon neck extension (a maneuver that will accentuate an enlarged thyroid). Ib: Goiter is palpable and visible on the inspection, with the neck in extension. The gland is, however, not visible with the neck in the normal, natural position
- Grade 2: Goiter is easily visible with the neck in a normal, natural position
- Grade 3: A very large goiter
Complications of Goiter
- Compressive Neck Symptoms. Compression of the trachea presents with dyspnea. Indeed, hemorrhage within a cystic or necrotic nodule can present with rapid onset of worsening dyspnea.
- Varying degrees of esophageal dysphagia. Positive Pemberton’s sign occurs due to obstruction of the thoracic inlet by a retrosternal goiter.
- Changes in voice (hoarseness) due to compression of the recurrent laryngeal nerve.
- Horner’s syndrome and paresis of the diaphragm are known complications.
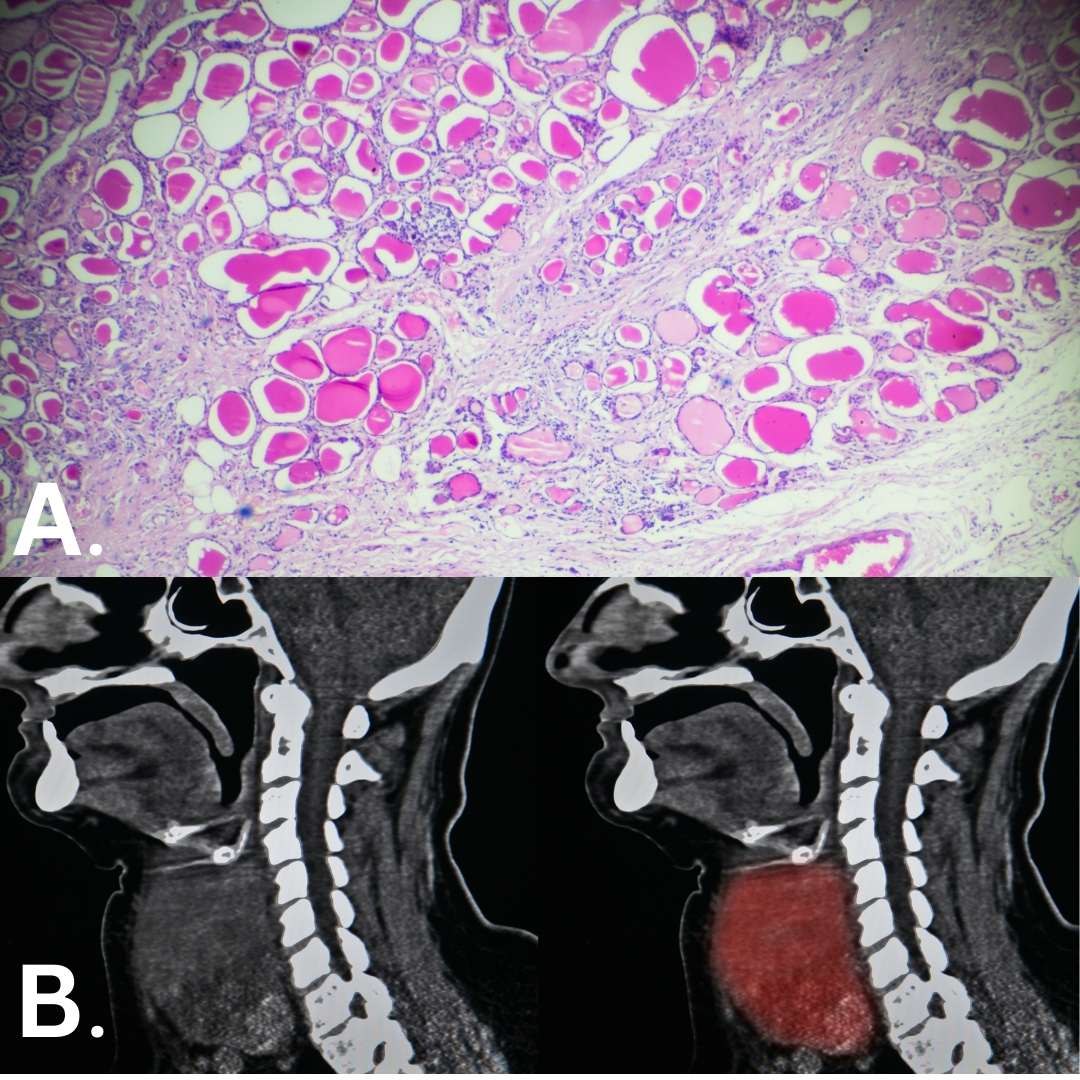
A. Clinical features of thyroid follicular cell hyperplasia. B. Significant goiter noted on computer tomography imaging (red highlight)
- Thyrotoxic transformation. Thyroid nodules may autonomously produce thyroid hormone.
The mechanism of hyperthyroidism in nodular thyroid disease : There is an initial thyroidal insult which may be in the form of nutritional iodine deficiency, goitrogens, or even autoimmune thyroid disease. Ultimately, there is a reduction in the synthesis of thyroid hormone. In response to this, there is a loss of negative feedback inhibition of pituitary thyrotropes. Consequently, there is an increase in the release of thyroid stimulating hormone. TSH promotes hypermetabolism and generation of hydrogen peroxide (required for thyroid hormone synthesis). Hydrogen peroxide can damage thyroid follicular cells. In addition, increased replication rate introduces various errors which overwhelm various intracellular processes aimed at preserving gene transcript integrity. Some of the inadvertent errors results in a gain of function mutation which promotes clonal expansion which may result in increased thyroid hormone production.
- Malignant transformation. Increased replication rate and hypermetabolism may also result in malignant transformation of a thyroid nodule.
- Infection. Viral or bacterial infection of the thyroid gland presents with anterior neck pain, tenderness, hyperpyrexia and general malaise.
Investigations
An array of investigations is required for the evaluation of Goiter.
- X-Ray: Plain radiograph of the chest (thoracic inlet and anterior-posterior diameter) may reveal a soft tissue swelling of the goiter. On some occasions, either diffuse or localized calcification involving thyroid nodules may be demonstrable on a plain roentgenogram. Tracheal deviation can be shown on inspection of the column of air in the tracheobronchial tree.
- Thyroid Ultrasound Scan: Ultrasound of the thyroid using a high-frequency probe typically shows a homogenously hyperechoic gland. Furthermore, thyroid ultrasound allows optimal screening for high risk thyroid nodules which may require fine needle biopsy.
- CT Scan: In patients with compressive symptomatology and features concerning retrosternal goiters, a CT scan of the chest may be required. Other sinister mediastinal masses such as tuberculoma, teratoma, and lymphomas would need to be ruled out.
- Thyroid function tests: TSH evaluation will usually be enough in the initial evaluation of goiters. If there is evidence of varying degrees of hypothyroidism or hyperthyroidism, additional hormonal testing would be mandated.
- Autoimmune thyroid panel: Screening tests for thyroid autoimmunity, including thyroid peroxidase antibody (TPO Ab), thyroglobulin antibody (Tg Ab), and Thyroid stimulating immunoglobulin (TSI) are recommended in select patients with goiter.
- Direct and indirect laryngoscopy: For patients with large goiters, laryngoscopy would be required in order to rule out asymptomatic vocal cord paresis.
Management of goiter
Prevention
Universal iodine supplementation in food leads to the amelioration of goiter in an at-risk population.
Medications
For patients with early onset endemic goiter, iodine supplementation may help reduce the size of a goitrous gland. Thyroid hormone supplementation was previously thought to be beneficial in nodular thyroid disease. Nonetheless, more recent evidence suggests that neither iodine nor thyroxine supplementation has demonstrable efficacy in reducing the size of a goitrous gland.
Fun fact: Despite the bold claims of this herbalist in Ghana, West Africa, this unfortunate patient’s cure for goiter cannot be “assured” through the use of herbal supplements. The photo was taken by Akuffo Quarde MD
Operative Treatment
Thyroidectomy is the treatment of choice for goiters with compressive symptomatology or cosmetic concerns.
Kindly Let Us Know If This Was helpful? Thank You!


