Insulin pumps are becoming increasingly popular as a way to manage diabetes, and for a good reason. Insulin pumps can provide better blood sugar control than multiple daily injections of insulin and can be much less disruptive to your life.
If you’re considering an insulin pump, there are a few things you should know. First, insulin pumps are not for everyone. They require a significant investment of time and effort to learn how to use them properly, and they’re not right for everyone with diabetes. Second, even if an insulin pump is right for you, it’s important to understand how they work and what their limitations are. Here’s a quick overview of insulin pumps.
Our Rating of the Best Insulin Pump
1
Tandem T Slim X2
Integrates with Dexcom G6, No calibrations needed, hybrid closed loop system. Touch screen display. Insulin Capacity = 300units
2
Omnipod 5
Integrates with Dexcom G6. No calibrations needed, hybrid closed loop system, Touch screen display. Insulin capacity = 200units
3
Medtronic 780G
Integrates with Medtronic Guardian™ 4 sensor, which does not require calibrations with SmartGuard™ technology, hybrid closed loop system, physical buttons, insulin capacity = 300units
How do insulin pumps work?
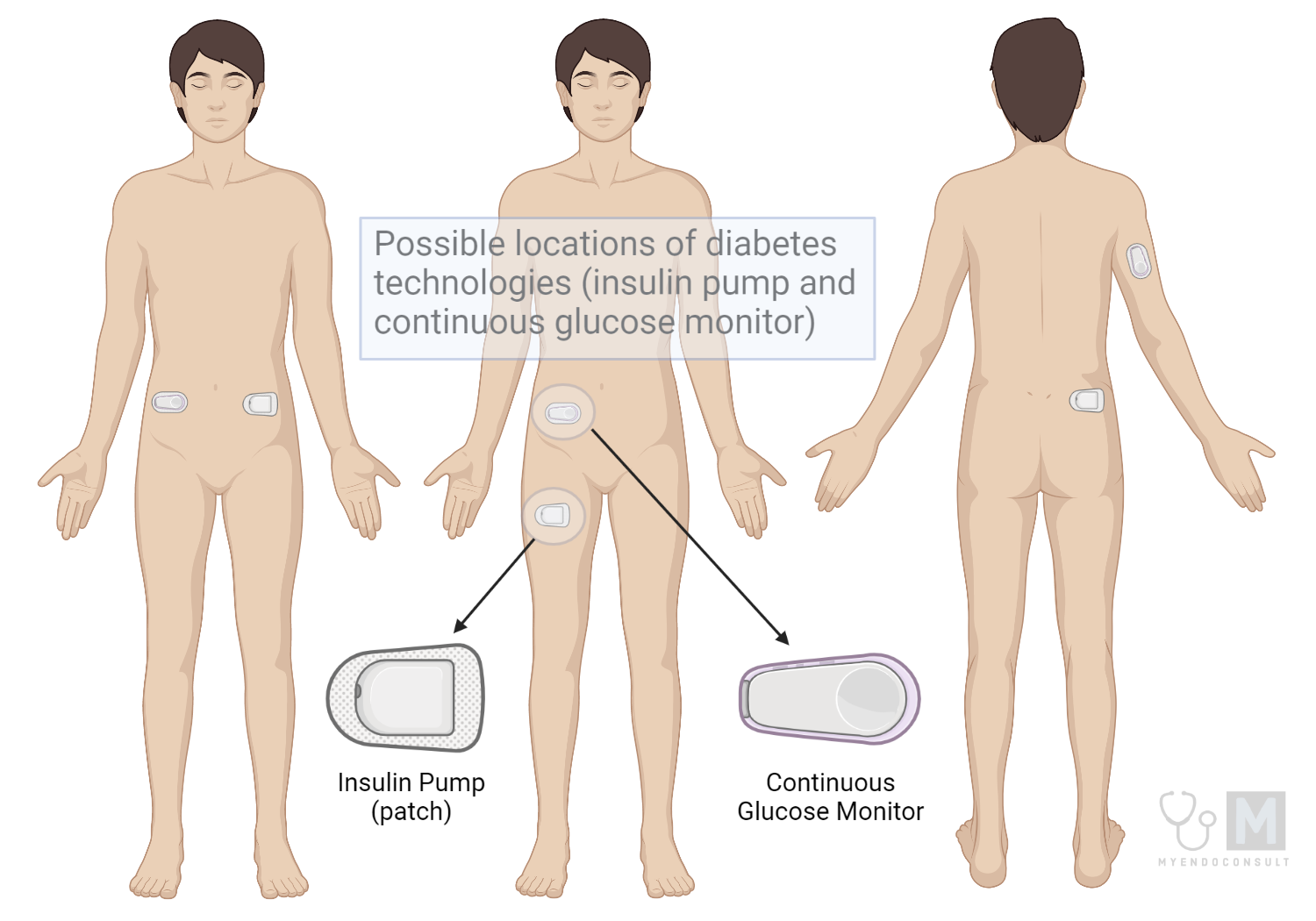
An insulin pump is a small, computerized device that delivers insulin through a catheter placed just under the skin. Insulin pumps are programmed to deliver small, steady doses of insulin throughout the day (known as a basal rate), and can also give larger doses of insulin at mealtimes (bolus doses).
What are the benefits of using an insulin pump?
There are several potential benefits to using an insulin pump. These include:
- Improved blood sugar control
- More flexibility in your daily routine
- Fewer low blood sugar episodes
- Reduced risk of long-term complications from diabetes
However, it’s important to remember that insulin pumps are not a cure for diabetes, and they don’t eliminate the need for careful self-management.
What are the disadvantages of using an insulin pump?
There are also some disadvantages to using an insulin pump. These include:
- The need for frequent blood sugar monitoring (CGMs have largely reduced the burden of frequent checks)
- The risk of diabetic ketoacidosis if the pump is not used properly (a diabetes emergency plan is required if you are on a pump)
- The inconvenience of wearing the pump all the time
- The cost of the pump and supplies
The types of insulin pumps
| Manufacturer | Medtronic | Insulet | Tandem Diabetes Care |
 |  | ||
| Legacy models | MiniMed (530G, 630G, 670G, 770G, 780G), MiniMed 508, Minimed Paradigm (511, 512, 712, 515, 715), MiniMed Paradigm REAL-time (522, 722), MiniMed Paradigm REAL-Time Revel) | Omnipod DASH, Insulet Omnipod UST400, Omnipod Eros | Tandem T:Slim G4, Tandem T:Flex |
| Current Model (Flagship) | MiniMed™ 780G system | Omnipod 5 | Tandem T:Slim X2 |
| Features | Links to a CGM (Guardian™ 4 sensor or Guardian™ sensor 3, Guardian™ 4 transmitter or Guardian™ Link 3 transmitter, Accu-Check Guide Link meter, and Test strips). Integrated insulin pump and display screen. Smartphone app (displays your blood sugar trends over time). Compatible with Medtronic Extended infusion set. | Links to Dexcom G6. PDM (An android phone displays blood sugars and pump settings). Can link to personal smartphone | Links to Dexcom G6. Integrated insulin pump and display screen. |
| Dimensions | 3.78 length x 2.11 width x 0.96 depth (inches) | 2.05 length x 1.53 width x 0.57 depth (inches) | 3.13 length x 2.0 width x 0.6 depth (inches) |
| Compatible insulin | Rapid-acting U100 insulin (Humalog® and NovoLog®) | U-100 insulins: Novolog, Humalog, admelog, fiasp | U-100 insulins: Novolog, Humalog |
| Basal increment | 0.025 units, 0.05 units, 0.1 units, Max bolus 0 to 25 units | 0.05 units | 0.1 units |
| Maximum basal rate | 0 to 35 units per hour or the Max Basal Rate amount, whichever is lower | 30 units per hour | 15 units per hour |
| Maximum bolus | Bolus Speeds Trending Standard: 1.5 units/minute Quick: 15 units/minute | 30 units | 25 units |
| Capacity of the reservoir | 300 units | 200 units | 300 units |
| Battery life | The pump requires one new AA (1.5 V) battery. For best results, use a new AA lithium (FR6) battery. The pump also accepts an AA alkaline (LR6) or a fully charged AA NiMH (HR6) nickel-metal hydride rechargeable battery. | Rechargeable lithium battery (android phone as PDM) | The rechargeable lithium battery of the pump can last for up to 7 days (depending on settings) |
| Basal programming | Three basal patterns | 12 basal patterns | 6 patterns |
| Insulin on board | Yes, SmartGuard™ technology can only be used for patients requiring 8 to 250 units/24hrs | Yes. SmartAdjust Technology | Yes. Control IQ and Basal IQ Technology |
| CGM integration | Yes, (Compatible with Guardian™ 4 sensor, change sensor every 7 days) | Yes (Compatible with Dexcom G6 CGM) | Yes (Compatible with Dexcom G6 CGM) |
| Calibration of CGM | No (when using the Guardian™ 4 sensor with SmartGuard™ technology) | No | No |
| Future Model | N/A | N/A | Tandem Mobi (tubeless pump), Tandem TSlim X3 (Mobile bolus feature or bolus by phone approved by FDA on Feb 16th 2022) |
| Major limitation | Patients are tethered to a tubing. | Restricted to 200units of insulin per day | Patients are tethered to a tubing. |
| Major Advantage | Hybrid-closed loop system. Meal Detection™ technology. Compatible with Medtronic Extended infusion set (up to 7 day wear time) | Hybrid-closed loop system. Tubeless pump | Hybrid-closed loop system |
How do I choose an insulin pump?
If you’re thinking about using an insulin pump, talk to your doctor or diabetes educator. They can help you decide if an insulin pump is right for you and, if so, which type of pump would be best. Once you’ve decided to use an insulin pump, you’ll need to choose a pump that’s right for you. There are many different brands and models of insulin pumps available, so it’s important to do your research before making a decision.
Considerations when choosing an insulin pump include:
- Ease of use: Some pumps are easier to use than others. Be sure to get a demonstration of the pump before you buy it.
- Cost: Insulin pumps are expensive, so be sure to find out what your insurance will cover.
- Size and weight: Insulin pumps come in different sizes and weights. Consider how easy the pump will be to carry with you throughout the day.
- Battery life: Insulin pumps run on batteries, so you’ll need to know how long the pump can run on a single charge.
- Features: Insulin pumps have different features, such as the ability to give bolus doses of insulin at mealtimes or to suspend insulin delivery when blood sugar is low. Consider which features are most important to you.
Choosing the best insulin pump
When it comes to insulin pumps, there is no one-size-fits-all solution. The best pump for you will depend on your individual needs and preferences. However, there are some factors that you should keep in mind when choosing a pump. First, consider the size of the pump. If you are active or frequently on the go, you may prefer a smaller, more compact pump. Second, think about the features that are important to you. Some pumps offer more advanced features than others, such as bolus calculators and wireless connectivity. Finally, be sure to consult with your healthcare team to ensure that the pump you choose is compatible with your insurance coverage. With all of these factors in mind, you can be sure to find the best insulin pump for your needs.
Tandem T Slim X2
The Tandem T slim X2 insulin pump is a state-of-the-art device that offers users the latest in diabetes technology. The pump features control IQ, which automatically adjusts basal insulin delivery to keep blood sugar levels in target range. In addition, the pump is a hybrid closed loop system, meaning that it can be used with compatible continuous glucose monitors (Dexcom G6) to improve control further.
| Feature | Comment |
| Time in range (70-180mg/dl) | The control IQ system prevents extreme glucose readings. |
| Ease of placing pump commands (bolus entries etc) | Via a colored and responsive touch screen |
| Water resistance | Watertight to a depth of 3 feet for up to 30 minutes |
| Effect of elevation above sea level | Interruption in insulin delivery can occur low atmospheric pressures (mountain climbing above 10,000 feet or take-off during air travel) |
| Integration with other devices | Bluetooth connectivity to phones and CGMs |
| Tethered Tubing | Tubing may get caught on clothing etc. |
| Battery life | It may require a recharge every 7 days (maximum, depending on usage) |
| Risk of inadvertent entries | The unlock procedure prevents accidental insulin boluses |
Omnipod 5
The Omnipod 5 Insulin Pump is a small, wearable insulin pump that provides a convenient and discreet way to manage diabetes. The pump can be worn on the body for up to three days at a time, and it is waterproof, so it can be worn during activities such as swimming or showering. The pump delivers insulin through a small plastic tube (cannula) that is inserted just under the skin. The pump automatically delivers insulin based on the user’s glucose levels, and it can also be manually adjusted to provide bolus doses of insulin before meals or snacks. The Omnipod 5 Insulin Pump is an easy-to-use and effective way to manage diabetes, and it offers a convenient and discreet alternative to traditional insulin pumps.
| Feature | Comment |
| Time in range (70-180mg/dl) | SmartAdjust Technology is a hybrid closed loop system |
| Ease of placing pump commands (bolus entries etc) | Entries via a simple touch screen of a separate handheld android smart device. |
| Water resistance | Waterproof for depths up to 25 feet for up to 60 minutes. It has IP28 certification |
| Effect of Elevation above sea level | Interruption in insulin delivery can occur at low atmospheric pressures (mountain climbing above 10,000 feet or take-off during air travel) |
| Integration with other devices | Bluetooth connectivity to phones and CGMs. Insulin pump can be controlled via either an Insulet-provided controller or a compatible phone (using the Omnipod 5 app) |
| Tethered Tubing | This is a tubeless pump. Some users love this feature. |
| Battery life | Recharge of lithium battery in Insulet-provided controller or a compatible phone |
| Risk of inadvertent entries | The unlock procedure prevents accidental insulin boluses |
Medtronic Minimed 780G
The Medtronic MiniMed™ 780G system is an insulin pump that utilizes advanced features to help people with diabetes manage their condition. The pump is capable of delivering insulin in small doses throughout the day, or it can automatically deliver a large bolus of insulin at mealtimes. The pump is designed with Meal Detection™ technology, which detects a rapid rise of blood sugar levels, typical during mealtimes, and pushing a correction dose. The pump is also able to automatically adjust insulin delivery based on the user’s blood sugar levels. The MiniMed™ 780G system also features a CGM (Continuous Glucose Monitor) that continuously monitors the user’s blood sugar levels and sends alerts to the pump if those levels get too high or too low. The system also comes with a smartphone app that allows users to track their blood sugar levels, insulin delivery, and other important data.
Feature | Comment |
Time in range (70-180mg/dl) | SmartGuard™ technology is a hybrid closed loop system. Fingersticks required in manual mode and to enter SmartGuard™. Pivotal trial participants spend avg of > 93% in SmartGuard™. |
Ease of placing pump commands (bolus entries etc) | Hard tactile physical buttons and a complex menu (learning curve) |
Water resistance | Waterproof for depths up to 12 feet for up to 24 hours (when the reservoir and tubing are properly inserted) |
Effect of Elevation above sea level | Interruption in insulin delivery can occur at low atmospheric pressures (mountain climbing above 10,150 feet) |
Integration with other devices | Bluetooth connectivity to smart phones, CGMs, and select Apple Watches®. |
Tethered Tubing | Tubing may get caught on clothing etc. |
Battery life | Standard AA battery life |
Risk of inadvertent entries | The unlock procedure prevents accidental insulin boluses |
The Verdict
Tandem T Slim X2
The Tandem T Slim X2 is arguably the best hybrid closed loop system on the market. It integrates with the Dexcom G6 CGM (the current gold standard of continuous glucose monitoring) which means no fingersticks. The control IQ keeps you in range.

Omnipod 5
The SmartAdjust technology is Insulet’s new hybrid closed loop system which is fully integrated with Dexcom G6. It is the third hybrid-closed loop system on the market. The absence of a tubing makes it appealing to some patients (e.g. athletes). Users of this pump type have more “real estate” in terms of their preferred site of pump placement. This can be advantageous in patients with significant scar tissue (lipohypertrophy), since alternate sites can be readily utilized without the inconvenience of being tethered to an infusion set.

Medtronic Minimed 780G
The current version of medtronic’s Minimed series, the Minimed 780G is an excellent hybrid closed loop system. Multiple or daily calibrations are no longer needed when using the Guardian™ 4 sensor with SmartGuard™ technology. Alerts issues from 770G have been addressed and are significantly less frequent. This is a huge improvement on previous versions of this pump, placing it on par with both the Tandem T slim X2 and Omnipod 5 pumps in terms of ease of use. The meal detection technology is a revolutionary feature that helps mitigate periods of significant postprandial hyperglycemia. As practicing endocrinologists, we have received very good feedback from patients who have switched to the current Minimed 780G pump.

Selecting a personalized insulin pump
We have developed this simple tool to help you select the right insulin pump for you. There are three simple questions. Are you willing to check your blood sugar twice a day? Do you prefer a tubed or tubeless pump and finally, how many units of insulin do you require a day. This tool is based on a well thought out algorithm based on feedback from patients, diabetes educators and diabetes care specialists.
Who can get an insulin pump?
Based on the current medicare guidelines in 2023, patients with type 1 diabetes mellitus and type 2 diabetes patients on an intensive multiple daily insulin injection regimen qualify for insulin pump therapy.
The decision to use an insulin pump as part of diabetes management is an individual one, and should be made in consultation with a healthcare provider. However, there are some general guidelines for who may be a good candidate for an insulin pump:
- Type 1 diabetes: Insulin pumps are typically used by people with type 1 diabetes who require insulin to manage their blood sugar levels.
- Intensive insulin therapy: Insulin pumps are generally used for people who require intensive insulin therapy, which means taking multiple daily injections of insulin or using a basal-bolus insulin regimen.
- Self-management skills: Insulin pump therapy requires a high level of self-management skills, including the ability to perform blood glucose monitoring and calculate insulin doses.
- Motivation and willingness to learn: Insulin pump therapy also requires a high level of motivation and willingness to learn about the device and its use.
- Financial coverage: Insulin pumps can be expensive, and may not be covered by insurance or other healthcare plans. People who are interested in using an insulin pump should check with their insurance provider to see if it is covered and what the cost may be.
In addition to these general guidelines, there may be specific medical considerations that need to be taken into account when deciding whether insulin pump therapy is appropriate. This includes factors such as pregnancy, age, and other health conditions.
It is important to note that insulin pumps are not appropriate for everyone with diabetes, and not everyone will benefit from this type of therapy. Your healthcare provider can help you determine if insulin pump therapy is right for you, and can provide guidance on how to use the device and manage your diabetes effectively.
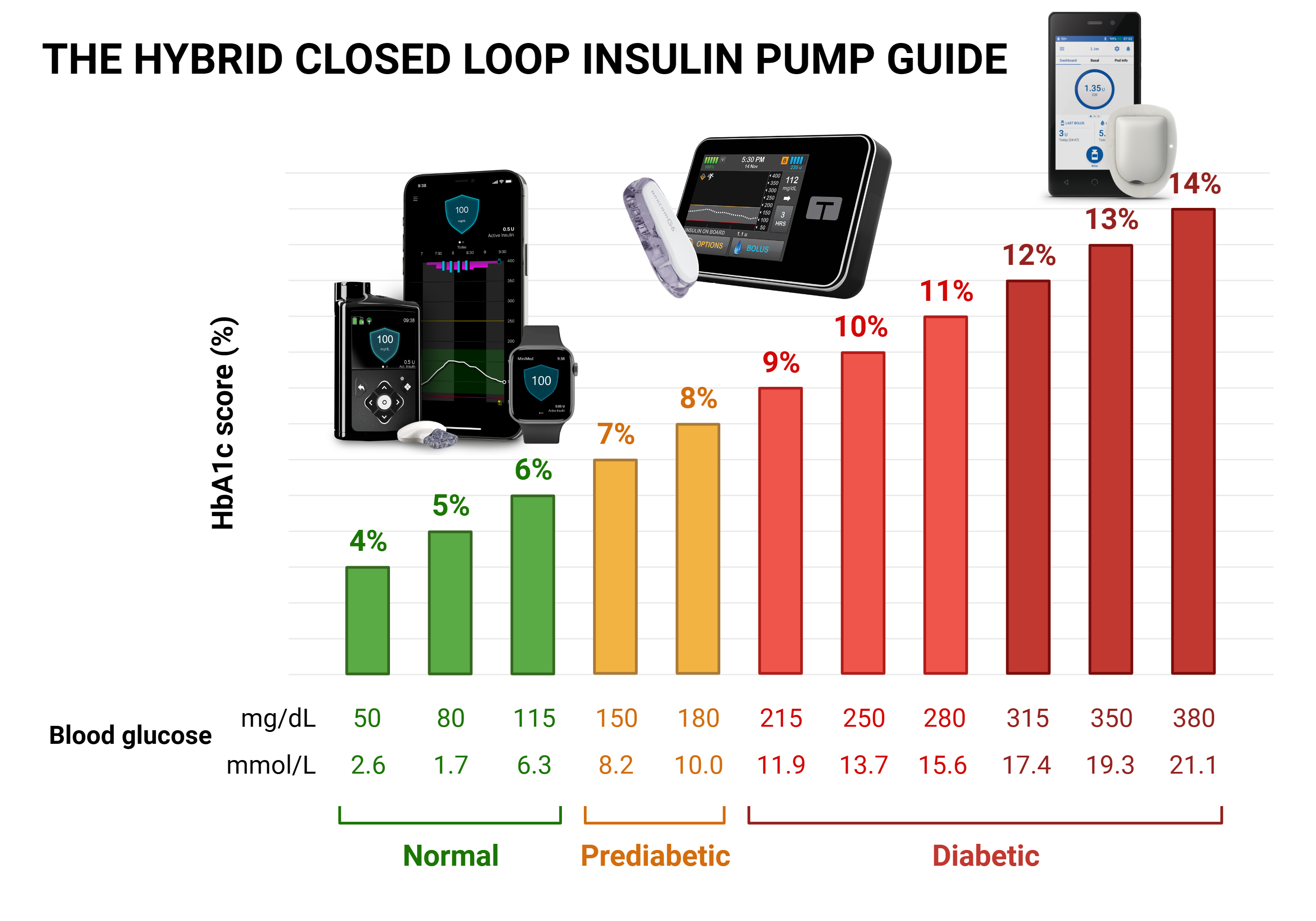
What does a hybrid closed-loop insulin pump mean?
The term “hybrid” in the context of the hybrid closed loop insulin pump refers to the combination of a continuous glucose monitor (CGM) and an insulin pump. The system is considered “closed loop” because the CGM and insulin pump are integrated and work together to automate insulin delivery. However, the system is not fully closed loop, as it still requires some manual input from the user.
The system is also referred to as an “artificial pancreas” because it mimics the function of the pancreas in delivering insulin to the body. The hybrid closed loop system uses the CGM to measure blood glucose levels in real-time, and the insulin pump uses an algorithm to calculate the appropriate amount of insulin to deliver based on the glucose levels, rate of glucose and the estimated insulin sensitivity factor of the individual.
Benefits
The hybrid closed-loop system has several benefits over traditional insulin pumps, including:
- Improved glucose control: The hybrid closed-loop system can help to maintain stable blood glucose levels, which can reduce the risk of long-term complications associated with diabetes.
- Reduced risk of hypoglycemia: The algorithm used by the hybrid closed-loop system is designed to minimize the risk of hypoglycemia by automatically adjusting insulin delivery based on glucose levels.
- Flexibility: The hybrid closed-loop system allows for more flexibility in daily activities, as the system can adjust insulin delivery based on changes in activity or food intake.
- Ease of use: The hybrid closed loop system is designed to be user-friendly and easy to operate, with a simple interface and automated features.
Limitations
The hybrid closed loop system also has some limitations, including:
- Cost: The hybrid closed loop system can be expensive, and may not be covered by insurance or other healthcare plans.
- Training: The system requires specialized training to use effectively, and may not be appropriate for individuals who are not able to learn how to use it.
- Maintenance: The system requires regular maintenance, including changing infusion sets and sensors, which can be time-consuming and require additional supplies.
New Insulin pump therapies in 2023
Medtronic’s diabetes program has faced significant competition in both the insulin pump and continuous glucose monitoring device sectors. Current generation hybrid closed loop systems such as the Tandem T slim X2 and Insulet’s omnipod 5 are fully integrated with the current gold standard for continuous glucose monitoring (CGM), that is, Dexcom G6 (soon to be Dexcom G7).
The major limitation to Medtronic’s adaptation by patients and endocrinologists alike had been the need for repeated fingerstick calibrations. The newest version of medtronic’s minimed series, no longer requires calibration. The current Medtronic Minimed 780G (with guardian sensor 4) is ideal for diabetes management (1,2).
References
- Collyns OJ, Meier RA, Betts ZL, Chan DSH, Frampton C, Frewen CM, et al. Improved Glycemic Outcomes With Medtronic MiniMed Advanced Hybrid Closed-Loop Delivery: Results From a Randomized Crossover Trial Comparing Automated Insulin Delivery With Predictive Low Glucose Suspend in People With Type 1 Diabetes. Diabetes Care. 2021 Feb 12;44(4):969–75.
- Medtronic announces latest data on MiniMedTM 780G system with the newest GuardianTM 4 sensori at American Diabetes Association 82nd Scientific Sessions [Internet]. Medtronic News. [cited 2022 Dec 5]. Available from: https://news.medtronic.com/Medtronic-Announces-Latest-Data-on-MiniMed-TM-780G-system-with-the-newest-Guardian-TM-4-sensor-at-American-Diabetes-Association-82nd-Scientific-Sessions
- American Diabetes Association Professional Practice Committee; Summary of Revisions: Standards of Medical Care in Diabetes—2022. Diabetes Care 1 January 2022; 45 (Supplement_1): S4–S7. https://doi.org/10.2337/dc22-Srev
Disclaimer
The opinions expressed here represent the views of a practicing hormone specialist (endocrinologist) and must not substitute the advice of your health care provider. This blog post is written for a non-medical audience interested in learning more about hormonal disorders. The author has no commercial conflicts of interest to declare. Also, read our privacy policy.
Kindly Let Us Know If This Was helpful? Thank You!


