Glucose monitors are one of the most important tools for people with diabetes. They help you keep track of your blood glucose levels throughout the day, which helps you manage your condition and prevent dangerous spikes or dips in your blood sugar levels. While there are several different types of glucose monitors on the market today, they all serve the same purpose: to provide immediate feedback about your body’s current state so that you can adjust your diet or diabetes medication accordingly.
There are two types of glucose monitors:
- Blood Glucose Monitors (BGMs) ; also known as glucometers
- Continuous Glucose Monitors (CGMs)
Glucometers are the most common type of blood glucose monitor. These devices check your blood sugar level and help you determine if it is too high or too low. People with diabetes use glucometers to check their fasting blood sugar levels at random times throughout the day. A healthcare professional can recommend what your targets should be based on factors like age, current medications, and other medical conditions you have.
When purchasing a glucose monitor, make sure you pick a meter that is compatible with any other devices you might use. For example, if you have an insulin pump, make sure the meter can sync with it. Also, check if your insurance will cover the cost of the meter and test strips before buying anything.
If you’re using an insulin pump to control your diabetes, be sure to get advice from your doctor about which meters (continuous glucose monitors or blood glucose monitors) are compatible with those types of devices.
Types of Blood Glucose Monitors
| Manufacturer | Types | Features |
| Abbott Diabetes Care | Freestyle freedom lite, freestyle elite, freestyle precision neo | The freestyle precision neo has test strips compatible with the freestyle libre CGM system. |
| Advocate | Advocate Redi-Code plus, Advocate Redi-Code plus speaking meter. | |
| Agamatrix | Presto, Presto Pro and Jazz Wireless 2 | |
| Arkray | Glucocard expression, Glucocard Shine, Glucocard Shine Connex, Glucocard Shine Express, Glucocard Shine XL, Glucocard Vital. | |
| Ascensia Diabetes Care | Contour Next, Contour Next EZ, Contour Next Link, Contour Next Link 2.4, Contour Next One | |
| CVS | CVS Health Advanced, CVS Health Bluetooth | |
| Dario Health | Dario Blood Glucose Monitoring System | |
| Diathrive | Diathrive Blood Glucose Monitor | |
| Fifty50 Medical | Fifty50 2.0, fifty50 2.0 sport | |
| Foracare | Fora 6 connect, For a D40D 2-in-1 (BP and glucose monitor) | |
| Genesis Health Technologies | GHT blood glucose meter | |
| IHealth | Align, Smart Gluco-Monitoring System | |
| LifeScan | Onetouch Ultra 2, Onetouch Ultramini, Onetouch Verio, Onetouch Verio Flex | |
| Livongo Health | Livongo Meter | |
| Nova Diabetes Care | Nova Max Link, Nova Max Plus | |
| Oak Tree Health | EasyMax NG and LTC, EasyMax V, Fortiscare EM66 | |
| Omnis Health | Embrace Pro, Embrace Talk, Embrace Evo | |
| One Drop | One Drop Chrome | |
| Prodigy Diabetes Care | Prodigy Autocode, Prodigy Iconnect, Prodigy Pocket, Prodigy Voice | |
| Roche | Accu-Chek aviva plus, Accu-chek guide, Accu-chek Guide Me | |
| Smart Meter | IGlucose | |
| Telcare | Telcare BGM | |
| Trividia Health | True Metrix, True Metrix Air, True Metrix Go, and TrueTrack | |
| US Diagnostics | EasyGluco, Infinity, Verasens | |
| Walmart | Relion Premier Blue, Relion Premier Classic, Relion Premier Compact, Relion Premier Voice, Relion Prime | If you plan on saving your money. Buy the cheapest and most cost friendly brand on the market, Relion Brand from Walmart! |
Parts of blood Glucose monitors
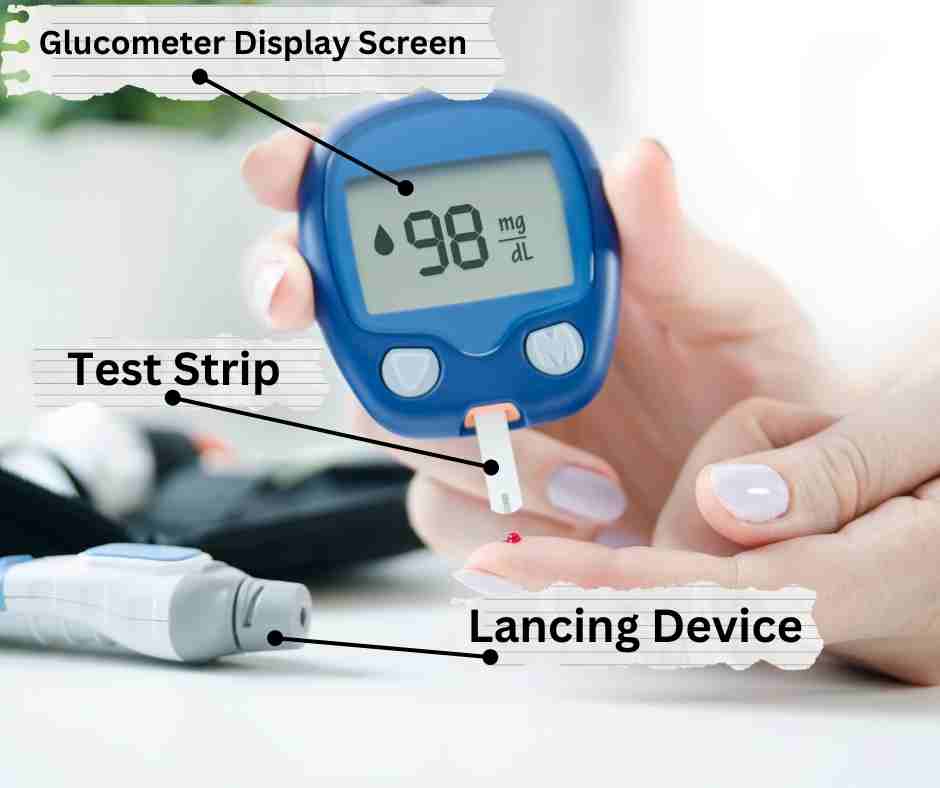
Test strip : The test strip is the part that contains the reagent required for estimating blood glucose levels. It has a slit that draws blood via capillary action when placed against a tiny drop of blood.
The meter : The handheld device with a display screen to show the estimated capillary glucose. More importantly, it has a slot to receive the test strip.
The Lancing Device : The lancing device is an important part of the glucometer. It’s what allows you to get a drop of blood for testing and also stores the needle. The lancing device has a spring-loaded needle that punctures the skin to various depths when primed and released. It puntures to various pre-selected depths based on patient preference. The most common way to use a lancet is by pressing down on it’s trigger release knob with your thumb after placing it against the desired site of the puncture. When you do this, the needle will come out and pierce through your skin; then, when you release pressure from your thumb, it retracts back into the lancing device
How Do Blood Glucose Monitors Work?
The first blood glucose monitor (glucometer) was developed in 1970 by Anton H. Clemens. It was an improvement on the previously invented dextrostix developed by Ernie Adams in 1963. Destrostix is a paper strip that produces a blue color whose intensity is proportional to the blood glucose concentration. Its major limitation was the need to compare the blue color shade to a color-concentration correlation chart. Clemens improved on this system by producing a proprietary method known as the Ames Reflectance Meter (ARM). This method measured the intensity of reflected light from the dextrostix strip in order to determine blood glucose concentration(1).
Current Glucose Monitors utilize two core principles in measuring blood glucose concentration.
- An enzymatic reaction occurs between blood glucose and an enzyme-impregnated test strip to generate a product that can be measured.
- The final product is detected and transmitted through an electrochemical gradient in order to estimate blood glucose concentration(2).
The test strips contain glucose oxidase, glucose dehydrogenase, or hexokinase enzymes. These enzymes react with glucose in capillary blood, leading to the production of either hydrogen peroxidase or intermediary compounds that can react with a color-producing compound (dye). A colorimetric method of measuring the intensity of the generated color is then used in measuring estimated glucose.
Glucose oxidase-based glucometers are the most cost-effective as such is utilized by most commercial manufacturers of glucometers.
How to choose the right glucometer (blood glucose monitor)
Accuracy of readings
The most important feature in a glucometer is the accuracy of its readings. Accuracy is critical because it’s the only way to be sure that your blood sugar levels are within target range and showing improvement over time.
Accuracy depends on two factors: the meter itself, and what kind of test strip you use. It can also vary depending on other factors like how you take your blood sample, how well you follow proper technique when testing.
Size of blood sample
The size of the blood sample requirement varies widely between models. While some meters require as little as 0.6 microliters (uL) per test, others require more than 1.8 uL for accurate results.
Time to get a reading
The time it takes to get a reading varies widely between models. Some meters take a blood sample and give you a reading in less than 30 seconds, while others take two minutes or longer. If you check your blood sugar often, this may be frustrating.
Backlit screens
Some glucometers have backlit screens that make it easier to read in dim light. This feature is a bonus if you often check your blood sugar at night. The downside of a backlit screen is that they can be more expensive than non-backlit models.
Bluetooth connectivity
If your meter has a wireless feature, it might connect to the internet or other devices using Bluetooth.
Bluetooth is more secure than USB cables because it encrypts data and authenticates each Device. This means that if your glucometer can connect by Bluetooth, you should be able to use it with a lot more devices—for example, Apple’s HealthKit or Android Wear watches would be compatible with your glucometer if they use Bluetooth.
USB rechargeable batteries
Some meters have USB rechargeable batteries, which is convenient if you travel a lot. You can charge them using your computer’s USB port, by plugging in an adapter into the car cigarette lighter (if there is one), or by charging with solar energy.
Voice Assist Technology
If you prefer to hear your results spoken aloud, some meters have voice technology that will announce your blood glucose reading. The voice can be in English or Spanish and sometimes also has a British accent. It’s important to note that while the meter may be able to give you instructions on how to use it, there are no voices available for instructions on what you should do with your blood sample after testing (e.g., how long you can keep it before discarding).
Some people find that the voice is easy to understand, and others find it difficult—so make sure that if this feature is important for you, try out some different models in person before making a purchase!
What is our recommended Blood Glucose Monitor?
In the end, your choice of glucometer depends on what features are most important for you. If you want an affordable and reliable meter that can read a blood sample quickly and accurately, then the Relion Brand (from Walmart) is a great choice. The Relion Premier classic glucometer costs 9 US Dollars per 50 glucose test strips. Indeed, this out-of-pocket cost is lower than some insurance co-pays for glucose test strips.
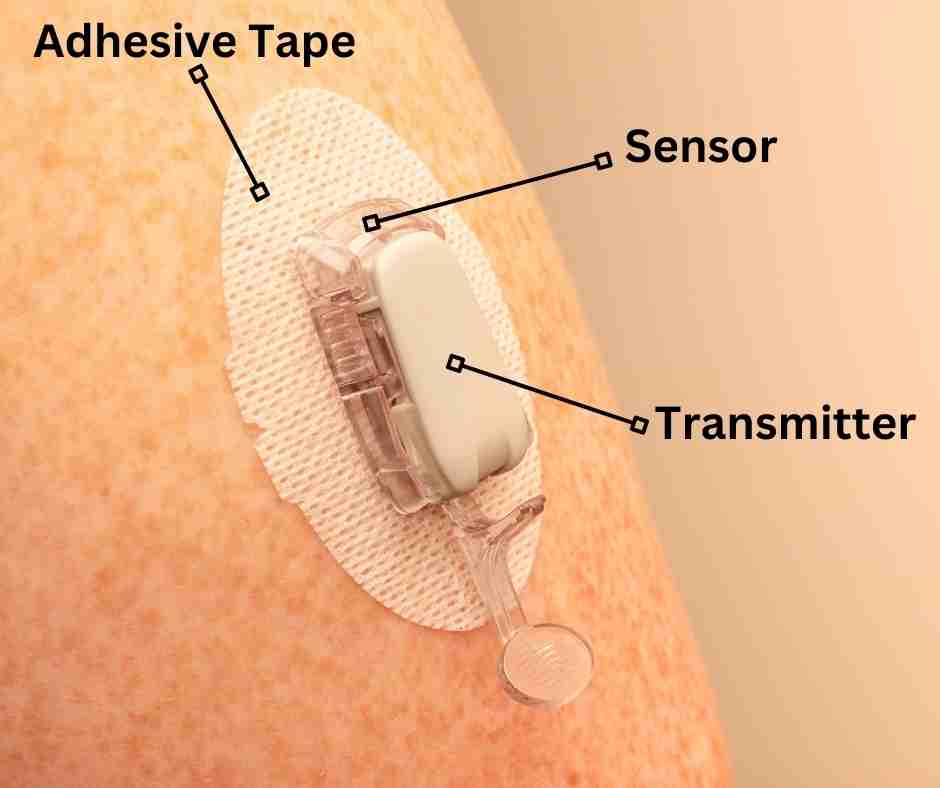
Continuous Glucose Meter
A continuous glucose meter (CGM), measures blood sugar every few minutes and sends alerts when levels are too high or low. It consists of two parts:
- A small sensor that’s inserted under the skin to measure glucose levels in interstitial fluid.
- A transmitter, which sends data from the sensor to a receiver unit that displays the information.
Pros of CGM
- Continuous glucose monitoring (CGM) can help you see trends in blood sugar, which may be helpful for adjusting meal plans and exercise routines.
- CGM allows you to see how food and exercise affect your blood sugar levels. This includes hyperglycemia and hypoglycemia, both of which can be dangerous if not monitored properly.
- CGM can help you avoid dangerous situations by showing when your glucose level is dropping or rising too quickly. If this happens, you can take action to bring it back into normal range before any physical harm occurs. Also these devices provide both tactile and sound alerts when blood sugars are dangerously high or low. Users of the Dexcom CGM system can share their blood sugar readings with a loved one. This will be most helpful for patients with cognitive impairment.
- Some brands of CGM require no calibration with fingersticks, making them a convenient tool for monitoring diabetes (e.g. Dexcom G6 and Freestyle libre).
Cons of CGM
- Some continuous glucose meters (CGM) require the user to calibrate with fingersticks (blood glucose monitor), which can be time-consuming and painful (Medtronic Guardian CGM).
- A user needs to be able to read and understand the results of their CGM device in order to make decisions about treatment plans while also considering other variables such as exercise, diet, and stress levels. As such, some users with cognitive impairments may face challenges in interpreting data accurately.
Cost and Insurance coverage for CGM
The cost of getting a CGM depends on your insurance provider and the type of device you use. If your doctor prescribes a Dexcom G6, Medtronic Guardian, or Abbott Freestyle libre CGM, it may not be covered by your insurance. In these cases, you’ll want to check out third-party financing options like CareCredit or Affirm. Alternatively, you may qualify for prescription assistance programs offered by these companies. If you are interested in paying for your sensors out of pocket, the most cost-friendly CGM system is the freestyle libre CGM from Abbott.
Brands of Continuous Glucose Meters
Dexcom G6
The Dexcom G6 sensor is a real-time, continuous glucose monitoring system that provides accurate estimated blood glucose readings based on interstitial glucose concentration. It works with various hybrid closed-loop insulin pump systems, including the Tandem T Slim X2 and Omnipod 5 insulin pumps. It is the current gold standard for CGM systems and is the go-to option recommended by diabetologists and endocrinologists.
A Dexcom G6 Applicator allows the insertion of the sensor into the skin using a simple push of a button. This can easily be done by the patient in the convenience of their home, without assistance.
The sensor sits in the subcutaneous (the fatty part of the skin) tissue. The Dexcom G6 transmitter sits on top of the sensor and sends glucose data directly to a smartphone or Dexcom G6 receiver.
The transmitter has a 3-month lifespan and should be removed and reapplied to a new sensor after every sensor change (every ten days).
- Approved Site of Application : Abdomen or Upper Buttocks
- Weight in grams : 11.4 grams
- Waterproof : It is safe for showering, bathing and swimming (limited by depth)
- Accuracy : Accuracy is based on the mean absolute relative difference between sensor glucose measurement and venous glucose (gold standard measured in a laboratory). Accuracy = 9.0%

EverSense CGM
Conventional CGM systems (Guardian, Dexcom, and Freestyle Libre) are associated with various problems, such as sensor adhesion issues, the large size of sensors, and the discomfort of wearing the sensor. The Eversense CGM system (Ascensia, previously Sensionics) is an implantable subcutaneous system that seeks to address some of the limitations of conventional CGMs.
It is inserted into the subcutaneous tissue of the upper arm by a trained physician under local anesthesia. An Eversense smart transmitter is worn over the sensor to allow the wireless transfer of glucose data to a mobile application.
The smart transmitter is kept in place with a mild silicone-based adhesive that is changed daily. The current sensor version can last for up to 6 months.
- Approved Site of Application: Upper Arms
- Weight in grams: negligible sensor weight
- Waterproof: It is safe for showering, bathing, and swimming
- Accuracy : Accuracy is based on the mean absolute relative difference between sensor glucose measurement and venous glucose (gold standard measured in a laboratory). Accuracy = 1.6%
Guardian Sensor 3
The guardian sensor 3 is a real-time CGM system. The integrated sensor-transmitter system needs to be changed every seven days. Patients on this system are required to have twice daily fingerstick calibrations (using a blood glucose monitor).
- Approved Site of Application: Abdomen and Upper Arms
- Weight in grams: 5.7 grams
- Waterproof: It is safe for showering, bathing, and swimming (limited by depth).
- Accuracy : Accuracy is based on the mean absolute relative difference between sensor glucose measurement and venous glucose (gold standard measured in a laboratory). Accuracy = 9.4%
Freestyle libre
The freestyle libre system (current version is the freestyle libre 3) is a real time CGM.The integrated sensor-transmitter system needs to be changed every 14 days. No calibrations are required, just like the Dexcom G6. The freestyle libre 3 system is smaller and has a flat side profile making it less obvious, than the current Dexcom G6. More importantly, patients are not required to scan the sensor with a reader, making it more convenient than the first version of freestyle libre.
- Approved Site of Application: Upper Arms
- Weight in grams: 5.0 grams
- Waterproof: It is safe for showering, bathing, and swimming (limited by depth).
- Accuracy : Accuracy is based on the mean absolute relative difference between sensor glucose measurement and venous glucose (gold standard measured in a laboratory). Accuracy = 12.0%
Summary of various Continuous Glucose Monitors
| CGM system (Manufacturer) | Frequency of sensor change | Need for calibration | Smartphone Compatibility | Ease of Application (Cost) |
| Dexcom G6 (Dexcom) | Every 10 days | No | Yes | Easy ($$$) |
| EverSense E3 (Ascensia) | Every 6 months | Yes (one time daily) | Yes | Hard ($$) |
| Freestyle Libre 2 (Abbott) | Every 14 days | No | Yes | Easy ($) |
| Guardian Sensor 3 (Medtronic) | Every 7 days | Yes (twice daily) | Yes | Easy ($$) |
What is our recommended Continuous Glucose Meter?
The freestyle libre series of sensors (Libre, Libre 2, or Libre 3), are the cheapest continuous glucose monitors on the market. The latest version, freestyle libre 3, has a flat side profile making it less obtrusive, compared to other real-time CGMs on the market. This version will be integrated with other hybrid closed-loop insulin pumps in the near future.
References
1. Tonyushkina K, Nichols JH. Glucose Meters: A Review of Technical Challenges to Obtaining Accurate Results. J Diabetes Sci Technol Online. 2009 Jul;3(4):971–80.
2. Bilen H, Kilicaslan A, Akcay G, Albayrak F. Performance of glucose dehydrogenase (GDH) based and glucose oxidase (GOX) based blood glucose meter systems at moderately high altitude. J Med Eng Technol. 2007 Apr;31(2):152–6.
The opinions expressed here represent the views of a practicing hormone specialist (endocrinologist) and must not substitute the advice of your health care provider. This blog post is written for a non-medical audience interested in learning more about hormonal disorders. The author has no commercial conflicts of interest to declare. Also, read our privacy policy.
Kindly Let Us Know If This Was helpful? Thank You!


