An Overview of Pemberton's Sign
Pemberton's Sign is a clinical marker used in the detection of thoracic outlet syndrome, specifically in cases of superior vena cava obstruction. First observed and described by the renowned physician Hugh Pemberton in 1946, this sign has since become a diagnostic cornerstone in identifying venous compression in the superior thoracic aperture.
A description of the classic Pemberton’s sign noted in patients with large goiters.
What are the clinical features?
This sign is eponymously named after Dr. Hugh Pemberton, who described this classic physical finding in a letter published in Lancet in 1946 titled “sign of a submerged goitre.” He explained the method of eliciting the sign, expected clinical findings, and also proposed a mechanism for the physical finding.
The sign is elicited by instructing the patient to lift their arms such that the arms touch both sides of the head. The patient is then instructed to hold their arms in that position until facial congestion or erythema is noticed.
Mechanism of Pemberton’s sign
A recent case report used magnetic resonance imaging (MRI) of the neck to elucidate the mechanism underlying Pemberton’s sign. In this report of a patient with a retrosternal goiter, there was no demonstrable craniocaudal change in the position of the thyroid gland during the maneuver to elicit the sign.
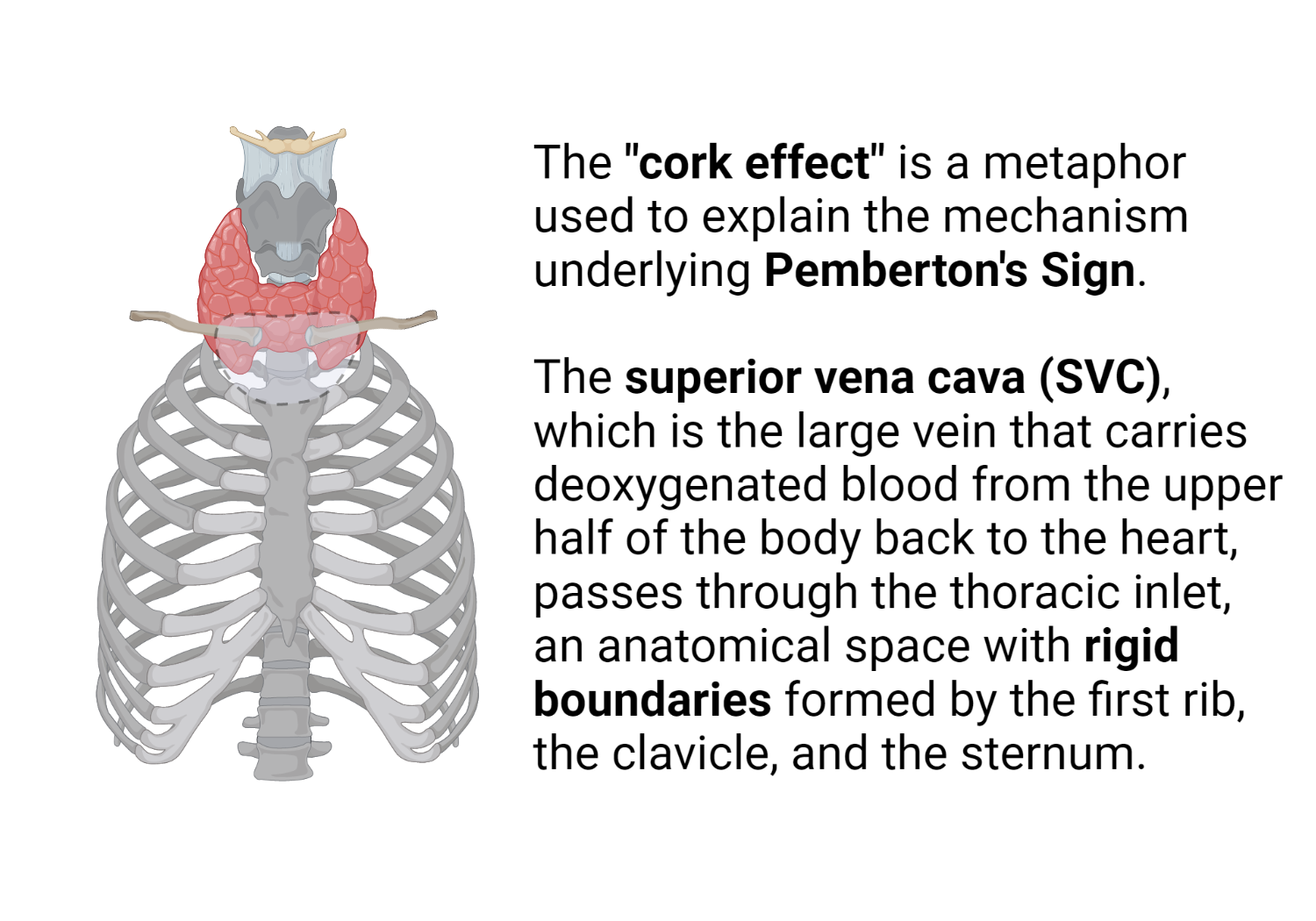
The widely accepted “cork effect” initially proposed by Pemberton was not consistent with the MRI findings noted in the study. The authors objectively confirmed compression of the external jugular and subclavian veins by the clavicles during the clinical maneuver. The thoracic inlet, however, remained relatively fixed in size, thus discounting the “cork effect” as a plausible explanation of Pemberton’s sign.
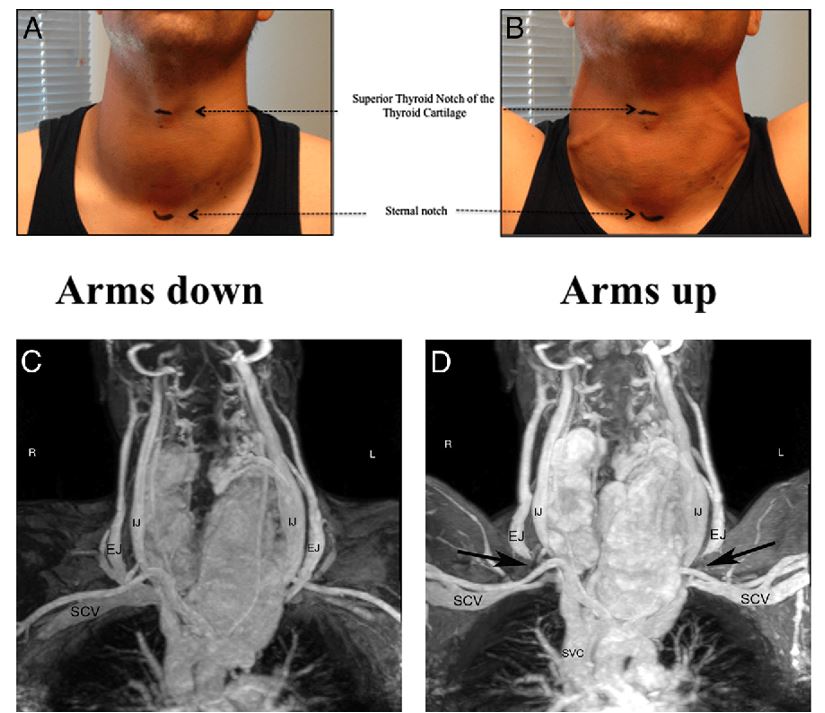
Figure 1. Mechanism of Pemberton’s sign. Dark arrows showing the compression of the external jugular veins bilaterally (pitures C and D). Thoracic inlet was not occluded by the goiter (pictures A and B). De Filippis, Elena et al. “Pemberton’s sign: explained nearly 70 years later.” The Journal of clinical endocrinology and metabolism 99 6 (2014): 1949-54 .
Correlation between Pemberton’s Sign and Thoracic Outlet Syndrome
Pemberton’s Sign is most commonly associated with thoracic outlet syndrome, although it can also indicate other thoracic obstructions such as mediastinal mass or tumors. Thoracic outlet syndrome refers to a group of disorders that occur when the blood vessels or nerves between the collarbone and the first rib (thoracic outlet) become compressed. This can cause pain in the shoulders and neck and numbness in the fingers.
Diagnostic Implications of Pemberton’s Sign
In terms of diagnosis, Pemberton’s Sign forms part of the armamentarium of physical examination maneuvers aimed at diagnosing conditions that present with venous congestion of the upper extremities due to supervisor vena cava syndrome.
It is, however, crucial to understand that Pemberton’s Sign is not pathognomonic for any particular disease and should be used in conjunction with a comprehensive medical history, clinical examination, and further diagnostic tests to confirm any suspicion of thoracic outlet syndrome or superior vena cava obstruction.
Pemberton’s Sign: A Valuable Tool in Medical Diagnosis
Although Pemberton’s Sign may not be a standalone diagnostic tool, its value lies in its simplicity and non-invasiveness. It can provide initial clinical suspicion for certain conditions that would warrant more specialized and costly investigations, thereby acting as a critical first step in the diagnostic journey..
Understanding and correctly identifying Pemberton’s Sign can prove instrumental in accelerating the diagnosis and treatment of thoracic outlet syndromes and superior vena cava obstructions, ultimately leading to improved patient outcomes.
Other Compressive signs (superior vena cava syndrome, phrenic nerve paralysis)
Superior vena cava (SVC) syndrome can occur in patients with large goiters. There are multiple case reports of mediastinal goiters leading to SVC syndrome. A goiter may sometimes not be palpable on the physical exam due to its ectopic position in the mediastinum. Clinically significant dyspnea due to either unilateral or bilateral phrenic nerve compression by large retrosternal goiters has been reported. In a recent large series of 50 retrosternal goiters, nerve compression syndromes were second only to tracheal compression in terms of clinically significant complications.
The compression of the brachiocephalic vessels by an extrinsic retrosternal thyroidal mass causes SVC syndrome. Ipsilateral distension of the subclavian, axillary, and jugular veins occurs as a consequence of impaired drainage of the brachiocephalic veins.
The phrenic nerve supplies motor innervation to the diaphragm and is derived from the 3rd,4th, and 5th cervical nerves, and passes in front of the anterior scalene muscle on its descent from the neck into the thoracic cavity. Extrinsic compression of the phrenic nerve during either its intrathoracic or cervical course results in dyspnea.
How does thyromegaly result in Horner’s syndrome?
Horner’s syndrome classically presents with ptosis, miosis, and enophthalmos. The superior cervical ganglion (SCG) serves as a relay center for higher-order neurons and has projecting from it, postganglionic neurons, which will eventually terminate in the orbit, skin of the head and neck region. It lies near the thyroid and is subject to extrinsic compression in the setting of significant thyromegaly.
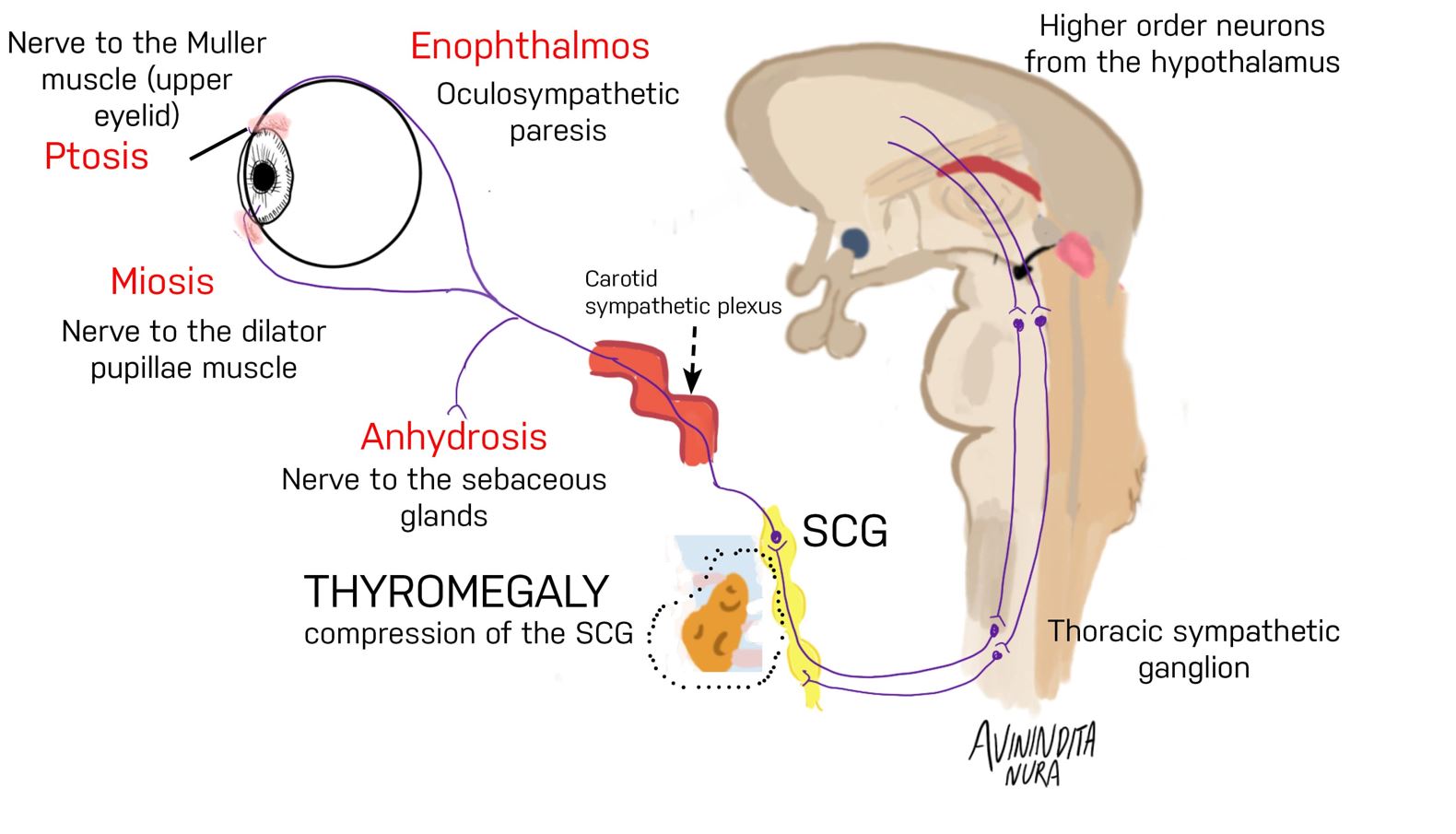
Figure. 2 Pathogenesis of thyromegaly-induced Horner’s syndrome. The superior cervical ganglion lies close to the thyroid gland and is subject to compression by an enlarged thyroid gland. Distal innervation of Muller’s muscle, dilator pupillae muscle, and sebaceous glands in the skin can be impaired by clinically significant thyromegaly. Motor neurons supplying Muller’s muscle are involved, accounting for ptosis. The involvement of sympathetic innervation of the dilator pupillae muscle accounts for miosis. Enophthalmos occurs because of oculosympathetic paresis.
References
- Pemberton HS (1946) Sign of submerged goitre. The Lancet 248:509
- De Filippis EA, Sabet A, Sun MRM, Garber JR (2014) Pemberton’s Sign: Explained Nearly 70 Years Later. J Clin Endocrinol Metab 99:1949–1954
- Marcelino M, Nobre E, Conceição J, Lopes L, Vilar H, de Castro JJ (2010) Superior Vena Cava Syndrome and Substernal Goiter. Thyroid 20:235–236
- van Doorn LG, Kranendonk SE (1996) Partial unilateral phrenic nerve paralysis caused by a large intrathoracic goitre. Neth J Med 48:216–219
- Amonoo-Kuofi HS (1999) Horner’s syndrome revisited: with an update of the central pathway. Clin Anat 12:345–361
- Kanagalingam S, Miller NR (2015) Horner syndrome: clinical perspectives. Eye Brain 7:35–46
Kindly Let Us Know If This Was helpful? Thank You!


