The mechanism of action of desmopressin and its clinical application in the management of central diabetes insipidus will be reviewed.
Physiology of Antiduretic Hormone Action
Antidiuretic hormone and regulation of serum osmolarity
Arginine vasopressin (AVP) is synthesized in the nuclei of paired hypothalamohypophyseal neurons originating from supraoptic and paraventricular nuclei of the hypothalamus and terminating in the posterior pituitary gland(1).
Neurosecretory granules containing AVP are transported along axons that terminate in fenestrated capillaries in the neurohypophysis (posterior pituitary)(2). The osmolarity sensing center (osmostat), located in the hypothalamus, regulates the release of AVP via relay neurons projecting to the cell bodies of the supraoptic and paraventricular nuclei(3).
There is a linear relationship between plasma osmolarity and plasma AVP levels, such that significant increases in plasma osmolarity cause a corresponding increase in plasma AVP(4). In the setting of dehydration, AVP, also known as antidiuretic hormone (ADH), increases water conservation at the level of the collecting duct, a process that increases urine osmolarity and leads to the restoration of normal plasma osmolarity(5) (see Fig. 1.0).
Key Message
Based on the results of this study, the frequency of significant hyponatremia (<130 mmol/L) was 4.2% when subjects were on intranasal desmopressin, compared to 1.3% when on oral desmopressin. This was statistically significant. Normal water and sodium balance are better achieved with oral DDAVP compared to intranasally administered DDAVP(16).
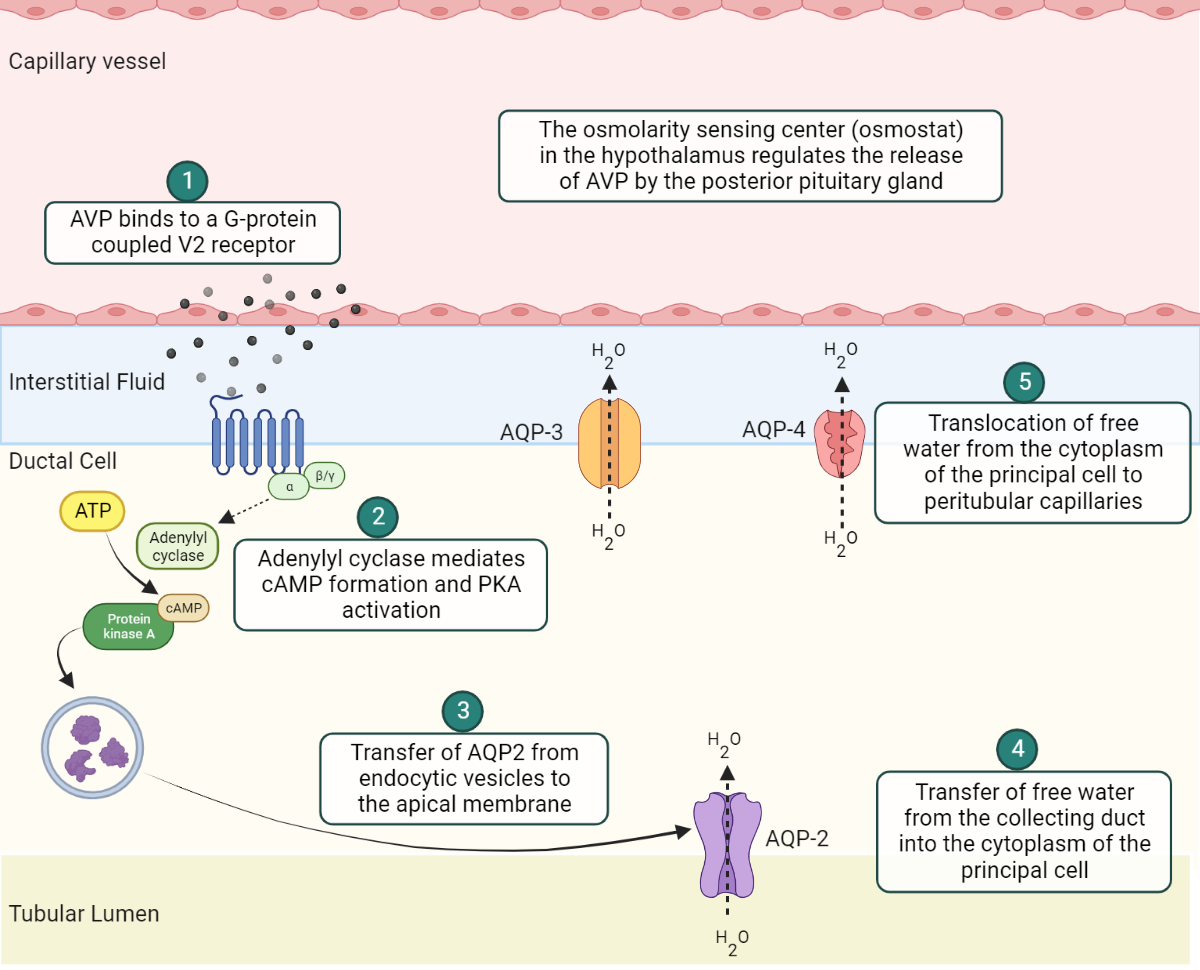
Fig. 1.0 Schematic representation of AVP mediated water conservation at the principal cell of the renal collecting duct
AVP binds to V2 receptors on G-protein coupled V2 receptors on the basolateral membrane (BM) of the principal cell(6). This initiates a cascade of intracellular processes involving adenylyl cyclase mediated cyclic adenosine monophosphate (cAMP) production and subsequent activation of protein kinase A (PKA). Afterwards, PKA will promote the liberation of aquaporins from endocytic vesicles. Aquaporin-2 (AQP2) released from vesicles inserts into the apical membrane (AM) of the collecting duct. This promotes the translocation of free water from the collecting duct into the cytoplasm of the principal cell(7). Aquaporin-3 (AQP3) and aquaporin-4 (AQP4) water channels, which are integral components (i.e., they are not released from endocytic vesicles) of the BM, facilitate the final transfer of water from the cytoplasm to the peritubular capillaries(5).
Mechanism of action of Desmopressin
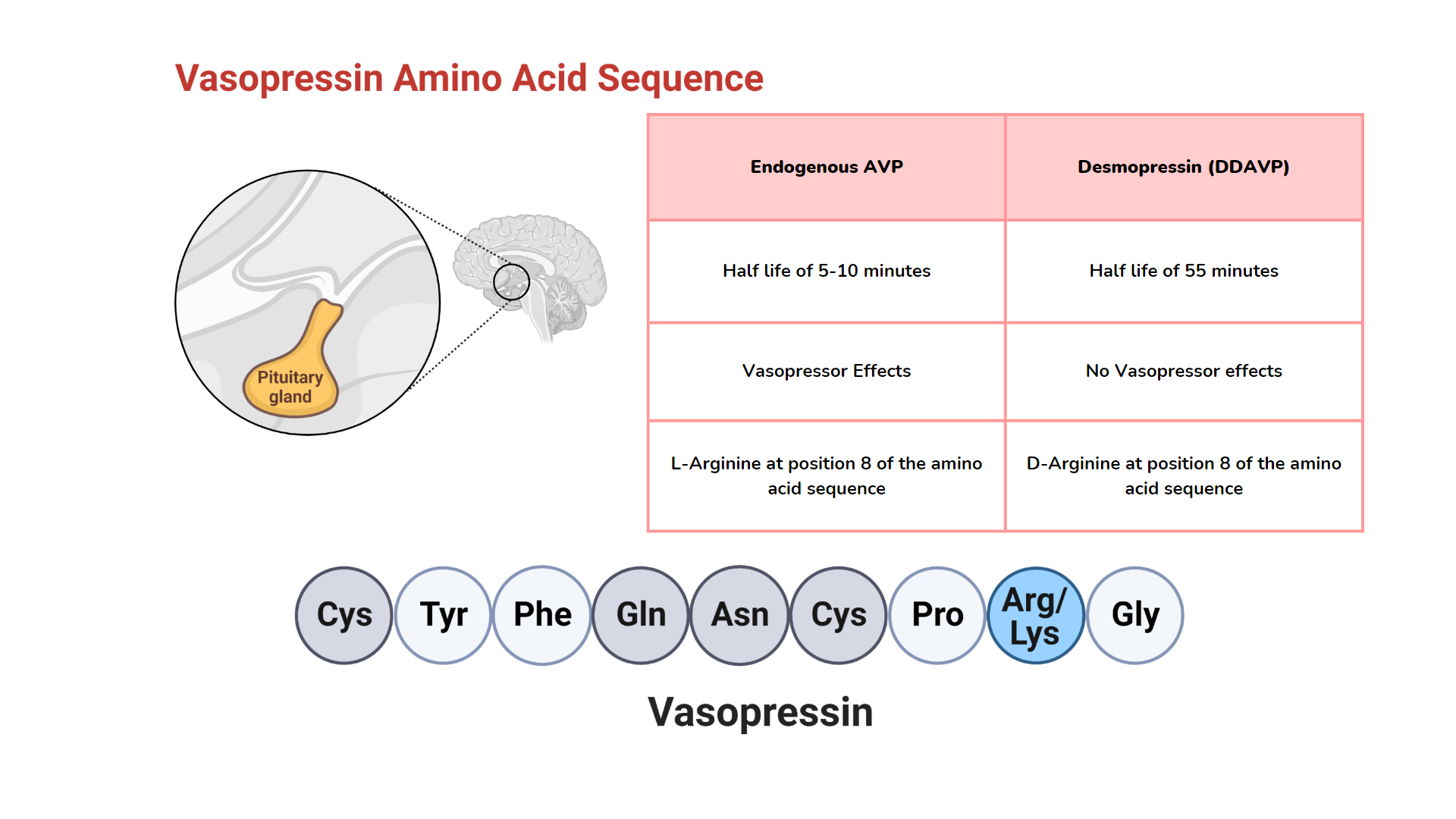
Desmopressin (1-deamino-8-D-arginine vasopressin, DDAVP) is an analog of arginine vasopressin (AVP)(8) with a prolonged plasma half-life of approximately 55 minutes (comparatively, endogenous AVP has a half-life of 5 to 10 minutes) (9).
It is worthy to note that substitution of D-arginine for L-arginine at position number 8 of the AVP amino acid chain eliminates the vasopressor effects of this synthetic analog of AVP(10).
Desmopressin promotes water conservation by binding to V2 receptors in renal collecting ducts(8). (See figure 1.0). During periods of significant dehydration, the central thirst mechanism allows the consumption of free water, which results in the restoration of intravascular volume and osmolarity(5,11).
Desmopressin Practice Guide
- Desmopressin can be administered safely through various routes (including intravenous, subcutaneous, oral, intranasal, and intramuscular). A simple rule of thumb is to use a conversion factor of 1:10 when converting between routes of administration(8).
Desmopressin conversion via the route of administration
Intravenous/Subcutaneous : Intranasal : Oral = 1mcg : 10mcg : 100mcg
- Co-administration of NSAIDs and desmopressin can lead to life-threatening hyponatremia(12). In normal physiology, prostaglandin E2 (PgE2) impairs the liberation of AQP2 from their endocytic vesicles after AVP to V2 receptor interaction. Cyclooxygenase inhibitors impair the synthesis of PgE2, thus increasing the availability of AQP2 (water intoxication) (13).
- Consider a “DDAVP holiday” intermittently to reduce the likely risk of hyponatremia. Patients can be advised to delay administration of a scheduled dose of DDAVP once a week until 2 or 3 successive episodes of breakthrough polyuria(14).
- Gastrointestinal peptidases denature oral desmopressin; as such, patients should be counseled on the importance of taking this medication either on an empty stomach or at least 90 minutes after a meal(15).
- Pituitary adenomas seldom present with central diabetes insipidus(CDI). CDI in the setting of a sellar mass is more suggestive of an alternative differential diagnosis, such as craniopharyngiomas or a granulomatous process(14).
Clinical Trial Evidence
In this retrospective study, the incidence of hyponatremia in patients with central diabetes insipidus was evaluated between intranasal and oral desmopressin routes of administration. Thirty-two subjects who had previously been well controlled on stable doses of intranasal DDAVP were switched to an oral route of administration for a maximum duration of 18months(16).
Explore the pathophysiology of various endocrine diseases and the mechanism of action of medications utilized in their treatment. Click here to learn more!
References
- Ishunina TA, Swaab DF. Vasopressin and Oxytocin Neurons of the Human Supraoptic and Paraventricular Nucleus; Size Changes in Relation to Age and Sex. J Clin Endocrinol Metab. 1999 Dec 1;84(12):4637–44.
- Miyata S. New aspects in fenestrated capillary and tissue dynamics in the sensory circumventricular organs of adult brains. Front Neurosci. 2015 Oct 27;9:390.
- Verbalis JG. How Does the Brain Sense Osmolality? J Am Soc Nephrol. 2007 Dec 1;18(12):3056–9.
- Terwel D, Jolles J. The relationship between plasma osmolality and plasma vasopressin concentration is altered in old male Lewis rats. Eur J Endocrinol. 1994 Jul;131(1):86–90.
- Kanbay M, Yilmaz S, Dincer N, Ortiz A, Sag AA, Covic A, et al. Antidiuretic Hormone and Serum Osmolarity Physiology and Related Outcomes: What Is Old, What Is New, and What Is Unknown? J Clin Endocrinol Metab. 2019 Nov 1;104(11):5406–20.
- Bankir L, Bichet DG, Morgenthaler NG. Vasopressin: physiology, assessment and osmosensation. J Intern Med. 2017;282(4):284–97.
- Boone M, Deen PMT. Physiology and pathophysiology of the vasopressin-regulated renal water reabsorption. Pflugers Arch. 2008 Sep;456(6):1005–24.
- Elder CJ, Dimitri PJ. Diabetes insipidus and the use of desmopressin in hospitalised children. Arch Dis Child Educ Pract Ed. 2017 Apr;102(2):100–4.
- Vilhardt H. Basic Pharmacology of Desmopressin. Drug Investig. 1990 Jan 1;2(5):2–8.
- Sawyer WH, Acosta M, Balaspiri L, Judd J, Manning M. Structural changes in the arginine vasopressin molecule that enhance antidiuretic activity and specificity. Endocrinology. 1974 Apr;94(4):1106–15.
- Bichet DG. Vasopressin and the Regulation of Thirst. Ann Nutr Metab. 2018;72 Suppl 2:3–7.
- García EBG, Ruitenberg A, Madretsma GS, Hintzen RQ. Hyponatraemic coma induced by desmopressin and ibuprofen in a woman with von Willebrand’s disease. Haemophilia. 2003;9(2):232–4.
- Verrua E, Mantovani G, Ferrante E, Noto A, Sala E, Malchiodi E, et al. Severe water intoxication secondary to the concomitant intake of non-steroidal anti-inflammatory drugs and desmopressin: a case report and review of the literature. Horm Athens Greece. 2013 Mar;12(1):135–41.
- Garrahy A, Moran C, Thompson CJ. Diagnosis and management of central diabetes insipidus in adults. Clin Endocrinol (Oxf). 2019;90(1):23–30.
- Oiso Y, Robertson GL, Nørgaard JP, Juul KV. Treatment of Neurohypophyseal Diabetes Insipidus. J Clin Endocrinol Metab. 2013 Oct 1;98(10):3958–67.
- Kataoka Y, Nishida S, Hirakawa A, Oiso Y, Arima H. Comparison of incidence of hyponatremia between intranasal and oral desmopressin in patients with central diabetes insipidus. Endocr J. 2015;62(2):195–200.
Kindly Let Us Know If This Was helpful? Thank You!


