Interpretation of the Glucagon Stimulation Test
Indications for the Glucagon Stimulation Test
To evaluate patients who are suspected to have growth hormone (GH) deficiency.
To gauge growth hormone reserve when either the insulin tolerance test or growth hormone-releasing hormone (GHRH)–arginine tests are contraindicated, not the chosen method, or not available.
Test Requirements
Pre-Test Requirements: Patients should not consume anything (Nil per os, NPO) except water after midnight and during the test.
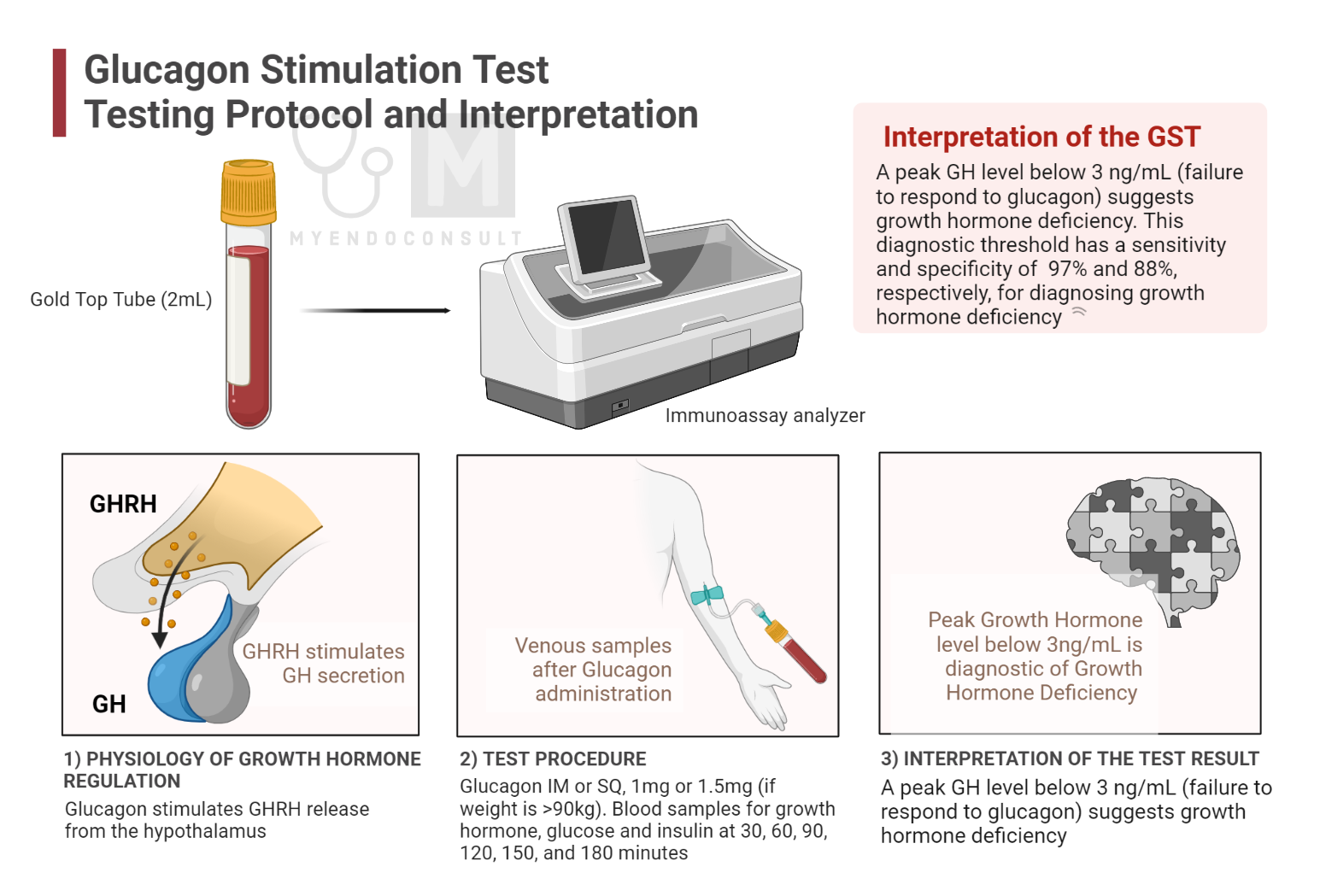
Required Equipment: Gold-topped tubes and glucagon are needed for this procedure.
Growth Hormone (GH) measurement method: An immunoenzymatic assay is used to assess the GH level.
Physiology of Growth Hormone and Glucagon Action
Biological Role and Functionality Glucagon, an important peptide hormone produced by alpha cells of the pancreas, plays a pivotal role in growth hormone (GH) regulation. Glucagon triggers the discharge of GH by influencing the hypothalamus and increasing the release of growth hormone-releasing hormone (GHRH). Subsequently, GHRH acts on the anterior pituitary gland, stimulating the synthesis and discharge of GH. In addition, GH regulation is also influenced by additional factors like somatostatin (also known as growth hormone inhibitory hormone, GHIH) and ghrelin, which inhibit and promote GH secretion.
Clinical studies have corroborated the role in GH level regulation, revealing that intravenous glucagon administration results in a substantial elevation in plasma GH levels. This response is assumed to be driven by stimulation of GHRH secretion and suppression of somatostatin release, which typically hampers GH secretion.
Beyond directly influencing GH release, glucagon also indirectly impacts GH levels through its regulation of blood glucose concentrations. A rise in blood glucose levels results in a reduction in GH secretion.
Growth Hormone Stimulation Test (Procedure)
The glucagon stimulation test serves as a diagnostic procedure used to identify GH deficiency in suspected individuals. The process involves glucagon administration, which prompts GH release from the anterior pituitary gland.
• Patients are instructed to fast for 8-12 hours before the test to guarantee precise results.
• An initial blood sample is drawn before glucose administration to assess the patient’s baseline GH, glucose, and insulin levels.
• Glucagon is administered intramuscularly or subcutaneously, typically at a dose of 1 mg or 1.5 mg (if body weight exceeds 90kg).
• Subsequent blood samples are collected at fixed intervals after administration of glucagon, typically 30, 60, 90, 120, 150, and 180 minutes. These samples are analyzed to measure GH, glucose, and insulin levels.
Interpretation of the Growth Hormone Stimulation Test
The peak GH level is determined from the collected samples, and the results are interpreted based on the specific laboratory reference range. A maximum GH response below a certain threshold (for example, less than 3 ng / mL, although this might differ between laboratories) may be indicative of growth hormone deficiency.
It should be noted that the glucagon stimulation test is not devoid of potential side effects, and patients may experience nausea, vomiting, or dizziness during the test. In addition, this test may not be appropriate for patients with certain health conditions, such as pheochromocytoma, due to the potential risk of blood pressure instability.
References
- Dichtel LE, Yuen KCJ, Bredella MA, Gerweck AV, Russell BM, Riccio AD, Gurel MH, Sluss PM, Biller BMK, Miller KK (2014) Overweight/Obese adults with pituitary disorders require lower peak growth hormone cutoff values on glucagon stimulation testing to avoid overdiagnosis of growth hormone deficiency. J Clin Endocrinol Metab 99:4712–4719
- Hosseinnezhad A, Black RM, Aeddula NR, Adhikari D, Trivedi N (2011) Glucagon-Induced Pheochromocytoma Crisis. Endocrine Practice 17:e51–e54
- Conceição FL, da Costa e Silva A, Leal Costa AJ, Vaisman M (2003) Glucagon stimulation test for the diagnosis of GH deficiency in adults. J Endocrinol Invest 26:1065–1070
Kindly Let Us Know If This Was helpful? Thank You!


