Beta-hydroxybutyrate (BHB) is a vital indicator of ketone-producing metabolic energy deficits that result from insufficient carbohydrate metabolism, leading to increased fatty acid catabolism. This article discusses the significance, reference ranges, indications and uses, clinical applications, and related tests of BHB measurements in whole blood, serum, or plasma. Furthermore, the article provides insight into the procedure, storage, handling, patient communication for BHB testing, and a detailed explanation of the ketogenesis process.
Ketone bodies, including beta-hydroxybutyrate, acetoacetate, and acetone, are produced in the liver from fatty acids during periods of low glucose availability, such as fasting, prolonged exercise, or carbohydrate-restricted diets. Elevated levels of BHB can be diagnostic of ketoacidosis, a life-threatening condition that results from the excessive production of ketone bodies. Beta-hydroxybutyrate is a significant marker for diagnosing diabetic ketoacidosis (DKA) and alcoholic ketoacidosis (AKA), two common forms of ketoacidosis.
Ketogenesis Process
The process of ketone body formation, known as ketogenesis, occurs primarily in the liver's mitochondria. Under normal circumstances, glucose is the primary fuel source for the body. However, during times of limited glucose availability, the liver begins to break down fatty acids into ketone bodies as an alternative energy source. This process is divided into several steps:
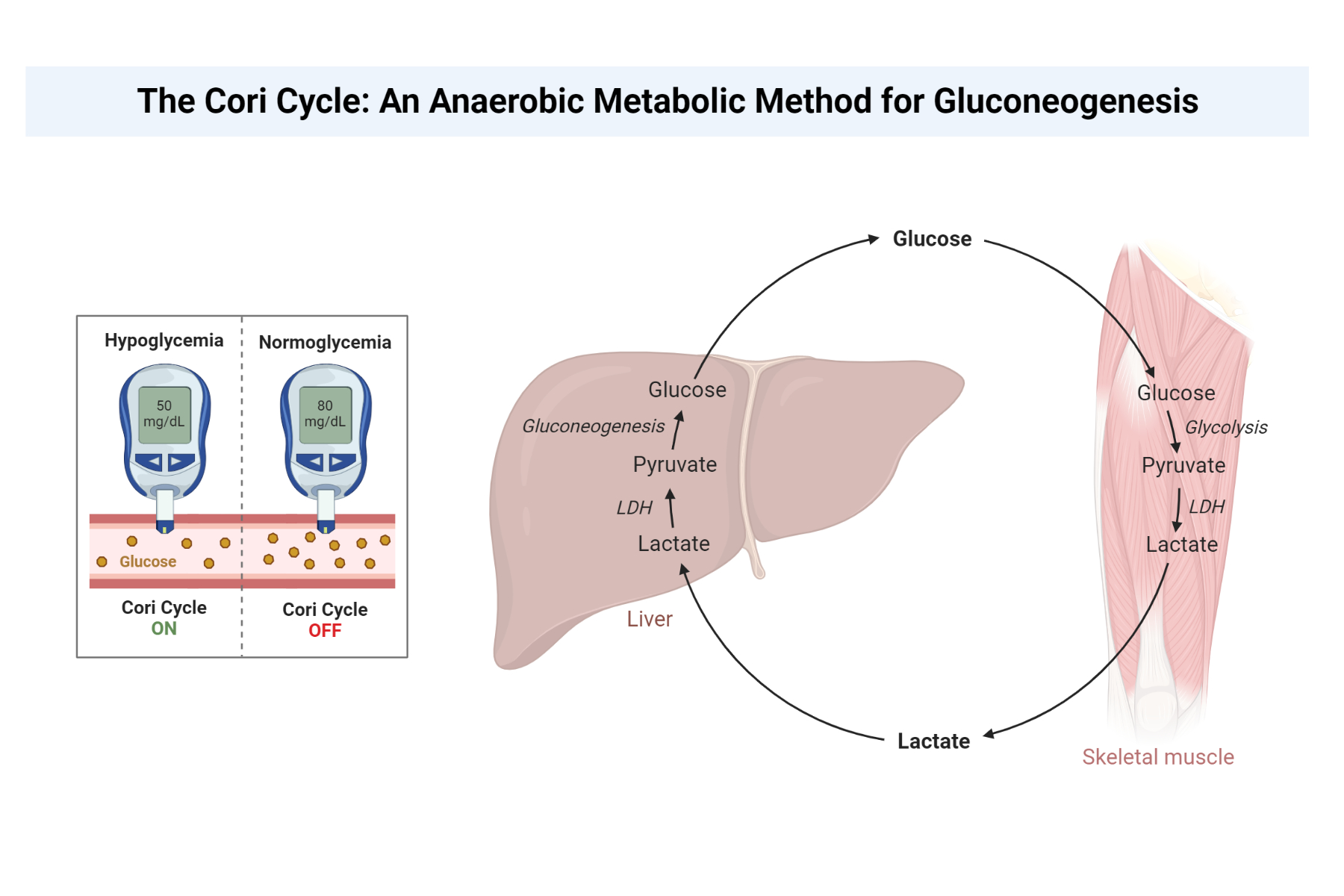
Lipolysis: In adipose tissue, triglycerides are hydrolyzed into glycerol and free fatty acids. The glycerol can be converted into glucose through gluconeogenesis, while the free fatty acids are released into the bloodstream and transported to the liver.
Beta-oxidation: Free fatty acids present in the liver then undergo beta-oxidation, a process that breaks them down into two-carbon acetyl-CoA molecules.
Formation of ketone bodies: The acetyl-CoA molecules are then converted into ketone bodies (acetoacetate, beta-hydroxybutyrate, and acetone) through a series of enzymatic reactions in the liver's mitochondria. The ketone bodies are released into the bloodstream and transported to peripheral tissues, where they can be used as an alternative energy source.
Reference Range
The reference range for BHB in whole blood, serum, or plasma is 0.21 to 2.81 mg/dL (20-270 micromol/L). When using the enzymatic-kinetic technique, the reference range for serum is less than 3.02 mg/dL (290 micromol/L).
Indications and Uses
BHB testing is indicated in cases of suspected alcoholic ketoacidosis and diabetic ketoacidosis. These conditions arise due to different etiologies, with DKA occurring in diabetic patients who experience a shortage of insulin and AKA occurring in individuals who consume excessive amounts of alcohol.
Clinical Applications
Common tests for ketone bodies, such as Acetest, Chemstrip, and Ketostix, do not detect beta-hydroxybutyrate. A handheld meter sensor system is available to monitor BHB and glucose levels simultaneously. The presence of elevated BHB levels is diagnostic of ketoacidosis, whereas the absence of concomitant hyperglycemia supports the diagnosis of alcoholic ketoacidosis. BHB levels equal to or greater than 3 mmol/L are indicative of ketoacidosis. In very severe diabetic ketoacidosis, the beta-hydroxybutyrate serum concentration may exceed 25 mmol/L.
Patients with isopropanol intoxication can present with high acetone levels without acidosis, anion gap, or abnormal glucose levels. In such cases, BHB testing can help differentiate between isopropanol intoxication and ketoacidosis.
Related Tests
In addition to BHB testing, urine ketones, and blood glucose level tests are crucial in diagnosing ketoacidosis. Urine ketones provide information on the presence of acetoacetate and acetone, while blood glucose levels help determine the severity of the condition and guide treatment.
Procedure
To measure BHB levels, plasma (lithium-heparin or fluoride-oxalate), serum, or perchloric acid (PCA) extracts can be analyzed. It is important to note that EDTA-plasma samples produce values that are 60% lower than specimens preserved with fluoride-oxalate or PCA.
Storage and Handling
Whole blood specimens are stable at room temperature for up to 48 hours. Plasma samples are stable at room temperature for up to 7 days, at 4°C for 14 days, and at -20°C for 6 months. PCA extracts can be stored at -20°C for up to 1 year. Repeated freeze-thaw cycling has no detrimental effect on sample integrity.
Patient Communication
There is no specific preparation required for patients before BHB testing. It is essential to inform patients that the test will involve drawing a blood sample, which may cause minor discomfort or bruising at the needle insertion site. Patients should be advised to report any unusual symptoms or side effects after the test. Once the test results are available, healthcare providers should discuss the findings with patients, explaining the implications of elevated BHB levels and potential treatment options, if necessary.
Conclusion
Beta-hydroxybutyrate is a valuable diagnostic tool for detecting ketone-producing metabolic energy deficits, such as diabetic ketoacidosis and alcoholic ketoacidosis. Understanding the ketogenesis process helps provide a more comprehensive view of the role BHB plays in energy metabolism and the potential consequences of elevated levels. BHB testing, combined with related tests such as urine ketones and blood glucose levels, is essential for accurate diagnosis and appropriate treatment of ketoacidosis. Proper storage and handling of samples, as well as clear communication with patients, ensure reliable results and optimal patient care.
Reference
Porter WH et al. Laboratory and clinical evaluation of assays for beta-hydroxybutyrate. Am J Clin Pathol 1997;107(3):353-8.
Kindly Let Us Know If This Was helpful? Thank You!


