What is the Somogyi phenomenon?
The Somogyi phenomenon, also known as the Somogyi effect or “rebound hyperglycemia,” is a pattern of blood sugar levels swinging from extremely low (hypoglycemia) to extremely high (hyperglycemia). It’s named after Michael Somogyi, a Hungarian-born professor of biochemistry who first described the phenomenon.
This effect typically occurs in people with diabetes, particularly type 1 diabetes. It happens when insulin or oral diabetic medication is taken before bedtime, leading to hypoglycemia during the early morning hours, usually between 2 a.m. and 3 a.m. This drop in blood sugar triggers a series of events:
- The body releases stress hormones like cortisol and epinephrine (adrenaline) to counteract the low blood sugar.
- These hormones stimulate the liver to release stored glucose back into the bloodstream.
- This causes a “rebound” effect, resulting in high blood sugar levels upon waking up in the morning.
- The high morning blood sugar levels can be mistaken for insufficient insulin dosage, leading to an increase in insulin dose and perpetuating the cycle.
It’s important to distinguish the Somogyi effect from the dawn phenomenon, which also results in high morning blood sugars but is due to natural circadian rhythm changes rather than a rebound from hypoglycemia.
Diagnosis of the Somogyi effect typically involves monitoring blood sugar levels during the night to confirm the presence of hypoglycemia. If it is diagnosed, management usually involves adjusting the timing, type, or amount of insulin or other diabetic medications.
Management of Somogyi Effect?
The management of the Somogyi effect primarily involves adjusting the diabetes treatment plan, which should be done under the guidance of a healthcare provider. Here are some strategies that might be considered:
- Adjusting insulin dosage or timing: If the Somogyi effect is suspected, the doctor might recommend decreasing the nighttime dose of insulin or moving the timing of the dose. For some people, splitting the insulin dose between dinner and bedtime could be helpful.
- Changing insulin types: If a person is on a type of insulin that peaks overnight, a doctor might suggest switching to a different type of insulin that has a smoother or more predictable effect.
- Diet and exercise modifications: Eating a snack before bed can help prevent nighttime hypoglycemia. Exercise routines may also need to be adjusted if they are contributing to low blood sugar levels at night.
- Continuous glucose monitoring (CGM): A CGM device can measure blood sugar levels throughout the day and night. It can help identify trends and patterns, enabling more personalized and effective management strategies. It can alert to low glucose levels, potentially preventing the onset of the Somogyi effect.
- Regular blood sugar testing: Frequent testing can help identify blood sugar patterns and can assist in differentiating between the Somogyi effect and dawn phenomenon. Testing might be required in the middle of the night (around 2 a.m to 3 a.m) when hypoglycemia is suspected.
- Diabetes education: Understanding how various factors such as diet, exercise, stress, illness, and medications affect blood glucose levels can help in better management of diabetes and prevent situations that trigger the Somogyi effect.
What is the Dawn Phenomenon?
The dawn phenomenon, also known as the dawn effect, refers to an increase in blood sugar levels in the early morning hours, typically between 2 a.m. and 8 a.m. This increase in blood glucose levels happens as a natural part of your body’s preparation to wake up.
The body prepares for waking up by secreting certain hormones, including cortisol, growth hormone, glucagon, and epinephrine. These hormones cause the liver to release glucose into the bloodstream, which raises blood sugar levels. This release is intended to give you the energy to start your day.
For people without diabetes, the body produces insulin to keep this increase in blood sugar in check. However, in people with diabetes, either the body does not produce enough insulin or the cells are resistant to the insulin’s effects. As a result, they may experience high blood sugar levels in the morning, even if they have not eaten anything since the night before.
The dawn phenomenon is different from the Somogyi effect, which is another cause of high morning blood sugars but is due to a rebound from low blood sugar (hypoglycemia) during the night.
Management of dawn phenomenon
The management of the dawn phenomenon should ideally be carried out in conjunction with a healthcare provider, as it often requires adjustments to the diabetes treatment plan. Here are some strategies that might be considered:
- Adjusting medication: Depending on the type and severity of your diabetes, your doctor may adjust the dose or timing of your medication. In some cases, if you’re taking insulin, you might need to switch to a type of insulin that’s longer-acting, or increase the dose of your evening insulin.
- Insulin pump: If you’re on insulin therapy, using an insulin pump can be beneficial. The pump can be programmed to deliver more insulin in the early morning hours to counteract the rise in blood glucose.
- Continuous glucose monitoring (CGM): CGM can be beneficial to track overnight blood sugar patterns and identify if and when the dawn phenomenon is occurring. This can help in tailoring the treatment plan more effectively.
- Dietary changes: Consuming a snack with some protein before bed can help to keep blood sugar levels steady through the night. It’s also important to monitor carbohydrate intake, as this can influence blood sugar levels.
- Exercise: Regular physical activity can improve insulin sensitivity and help manage overall blood glucose levels. However, it’s important to monitor your blood sugar before, during, and after exercise, as physical activity can lower blood glucose levels and potentially lead to hypoglycemia.
- Regular blood sugar testing: Regular testing, especially in the early morning hours, can help identify blood sugar patterns and assist in differentiating between the dawn phenomenon and other causes of high morning blood sugars, like the Somogyi effect.
Similarities between somogyi effect and dawn phenomenon
The Somogyi effect and the dawn phenomenon are both conditions that primarily affect individuals with diabetes, particularly those with type 1 diabetes. They have some key similarities, as follows:
- Morning hyperglycemia: Both the Somogyi effect and the dawn phenomenon result in high blood sugar levels (hyperglycemia) in the morning. People with either condition will typically wake up with blood glucose levels that are higher than their targets.
- Physiological responses: Both phenomena are a result of physiological responses in the body. The dawn phenomenon occurs due to natural hormonal changes in the early morning that increase insulin resistance, while the Somogyi effect is a rebound response to low blood glucose levels during the night.
- Importance of blood glucose monitoring: Identifying either condition requires regular blood glucose monitoring, particularly during the night and early morning hours. This helps to understand the pattern of glucose variations and is crucial in management strategies.
- Impact on diabetes management: Both conditions can affect the overall management of diabetes, as they may necessitate changes in diet, exercise, medication type, dosage, or timing.
Despite these similarities, the underlying causes of the Somogyi effect and dawn phenomenon are different, and they require different strategies for optimal management. Therefore, accurate identification of the specific condition is important for the appropriate treatment approach.
Differences between Somogyi Effect and Dawn Phenomenon
Refer to the table and continuous glucose monitor tracing of the glycemic profiles of Somogyi effect, Dawn phenomenon and overbasalization.
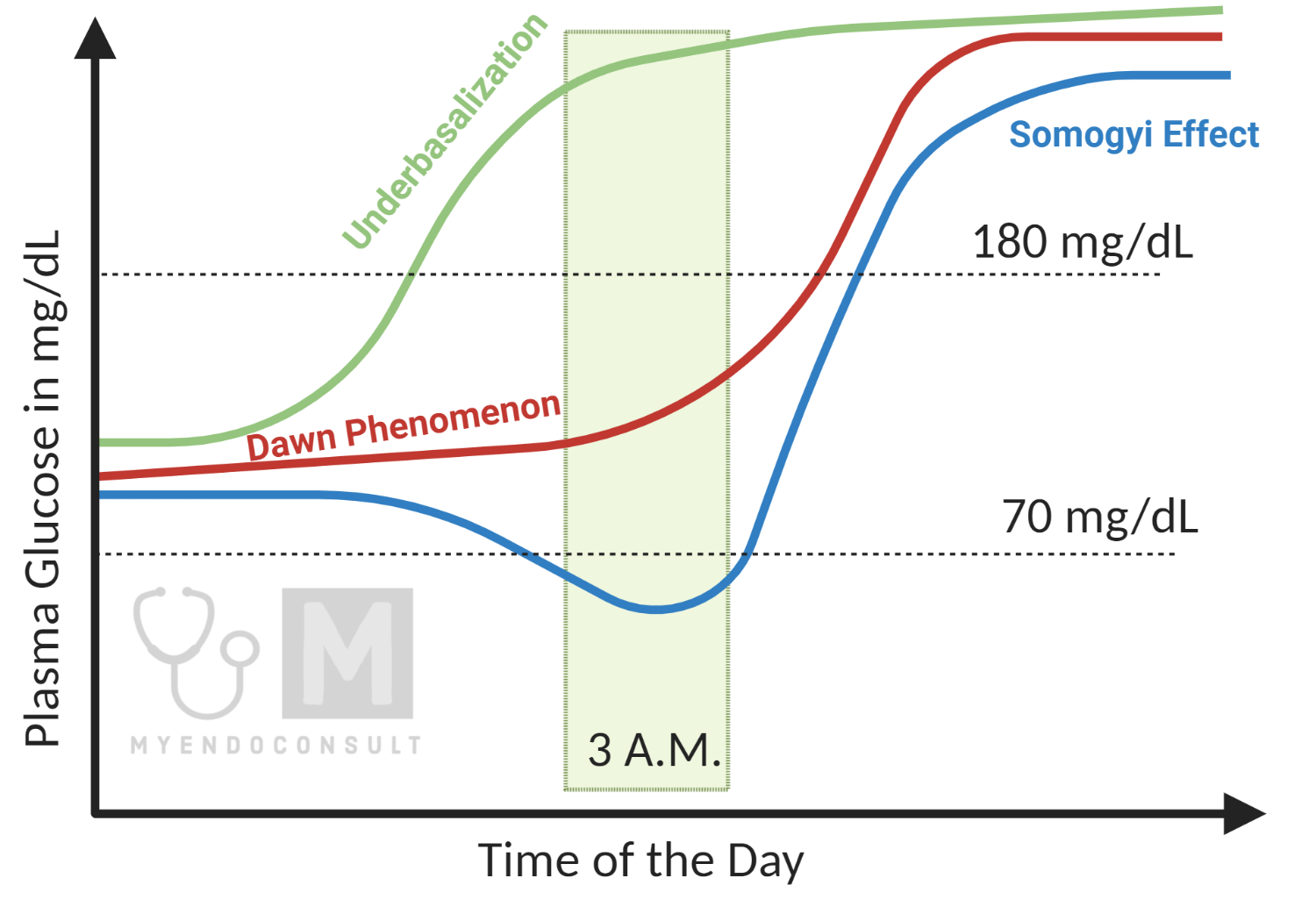
| Table 1. Comparison of the Dawn Phenomenon and Somogyi Effect | |||
| Glycemic trend | Bedtime Glucose | 3AM Glucose | Morning Glucose |
| Somogyi effect | Normal | Low (hypoglycemia) | High (hyperglycemia) |
| Dawn phenomenon | Normal | Normal | High |
| Underbasalization | Normal | High | Very high |
Frequently Asked Questions
What is underbasalization?
Underbasalization is a term often used in the management of diabetes, particularly in those using insulin therapy. “Basal” refers to the background or baseline level of insulin that is continuously present in the body. In people without diabetes, the pancreas naturally secretes this insulin. For people with diabetes, especially type 1, this must be replicated via insulin injections or an insulin pump.
Underbasalization, therefore, refers to a state where there is insufficient basal insulin to meet the body’s needs. This can lead to persistently high blood sugar levels (hyperglycemia) throughout the day and night, not just in relation to meals.
It’s important to have the right amount of basal insulin to keep blood sugar levels stable when not eating, and to counteract the glucose that is released by the liver. Too little basal insulin (underbasalization) can result in high blood sugar levels, while too much can lead to low blood sugar levels (hypoglycemia).
If underbasalization is suspected, adjustments may need to be made to the insulin regimen, such as increasing the dose of basal insulin, changing the type of insulin used, or adjusting the timing of doses.
What is overbasalization?
Overbasalization in diabetes care refers to a situation where too much basal insulin is being administered. “Basal” refers to the background or baseline level of insulin that is continuously present in the body.
In people without diabetes, the pancreas naturally secretes this insulin. However, people with diabetes, especially type 1, may need to replicate this background insulin via injections or an insulin pump.
When too much basal insulin is given (overbasalization), it can lead to persistently low blood sugar levels (hypoglycemia). Symptoms of hypoglycemia can include shaking, sweating, rapid heartbeat, confusion, and in severe cases, seizures or loss of consciousness.
If overbasalization is suspected, adjustments may need to be made to the insulin regimen, such as decreasing the dose of basal insulin, changing the type of insulin used, or adjusting the timing of doses. It’s crucial to remember that any changes to the diabetes management plan should be made under medical supervision. Regular monitoring of blood glucose levels is also key to managing diabetes effectively and safely.
Kindly Let Us Know If This Was helpful? Thank You!


