Glucocorticoids, such as dexamethasone, methylprednisolone, and prednisone, are a class of steroid hormones that have various effects on the immune system. One notable consequence of their use is an increase in the white blood cell (WBC) count, primarily attributed to a rise in neutrophils, also known as polymorphonuclear leukocytes (PMN). This article aims to provide a comprehensive understanding of the biological processes that lead to the increase in circulating PMNs and the importance of these changes when evaluating patients receiving glucocorticoid treatment.
The Composition of White Blood Cells
A WBC count measures the total number of leukocytes present in a patient's blood. These leukocytes consist of neutrophils (60-70%), lymphocytes (28%), monocytes (5%), eosinophils (2-4%), and basophils (0.5%). Neutrophils, being the most abundant leukocytes, play a significant role in changes observed in the WBC count. These cells, also referred to as Polymorphonuclear neutrophils (PMNs), undergo several developmental stages before maturing.
Immature neutrophils are initially released from the bone marrow and are characterized by a nonsegmented, band-like nucleus, earning them the name "bands." An increase in circulating immature neutrophils often indicates a bacterial infection, as they are mobilized to combat the invading pathogens. This phenomenon is typically referred to as a "left shift" in a WBC differential
As the immature neutrophils become activated or exposed to bacteria, their nuclei adopt a segmented appearance. Neutrophils are found in various compartments within the body, with the marginal (neutrophils attached to blood vessel endothelium) and circulating compartments being the most relevant to this discussion.
Glucocorticoids and Their Impact on WBC Count
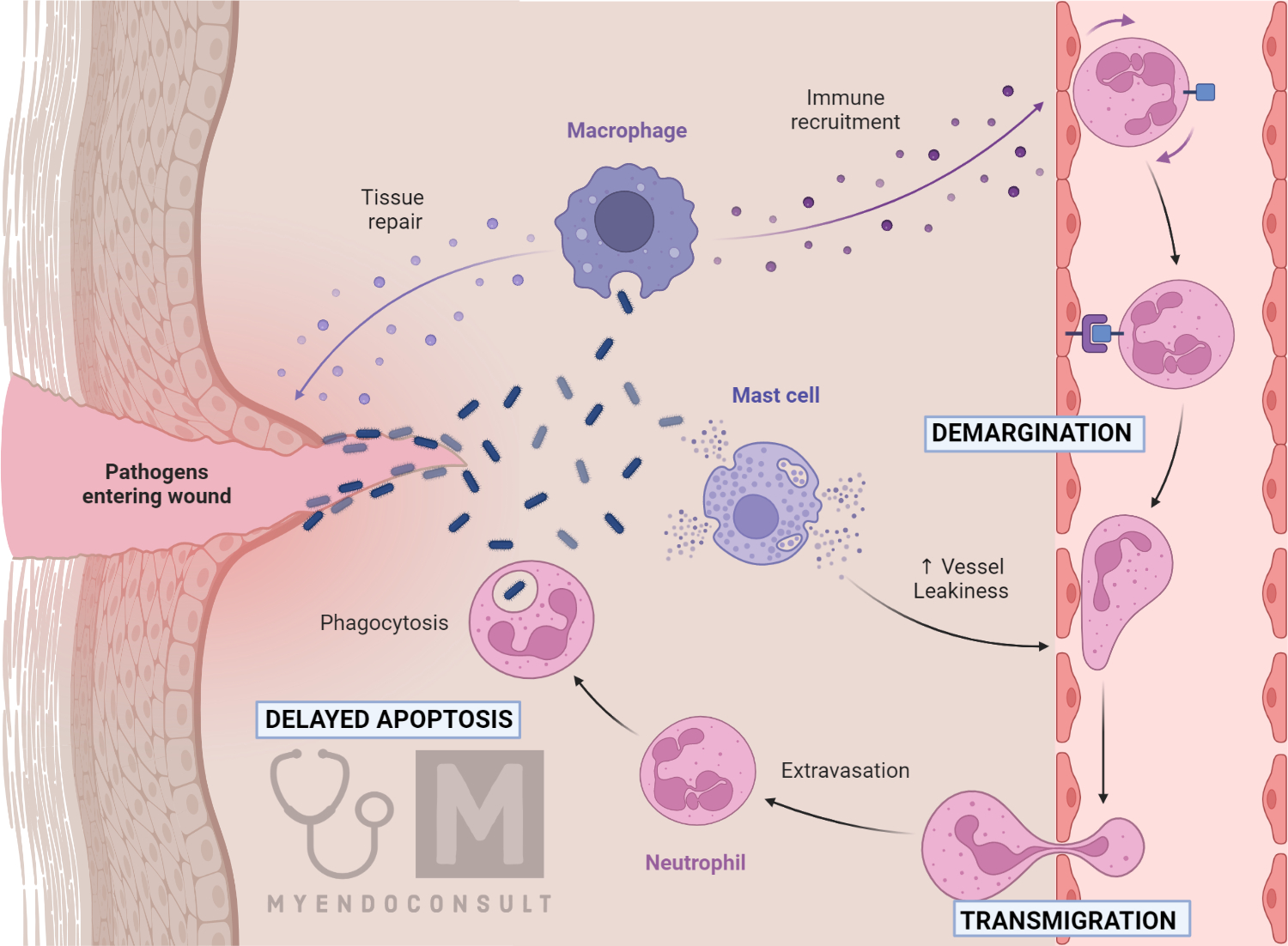
The administration of glucocorticoids (e.g., dexamethasone, methylprednisolone, prednisone) is known to cause an increase in WBC counts, predominantly due to elevated PMN levels. This increase can be attributed to several factors:
- Demargination of neutrophils from the endothelial surface of blood vessels.
- Delayed transmigration of neutrophils into tissues.
- Delayed apoptosis (programmed cell death).
- Increased release of neutrophils from the bone marrow.
While all these factors contribute to the rise in circulating neutrophils, demargination has the most significant impact. Some studies have reported WBC count increases greater than 20,000/mm3 within the first day of glucocorticoid administration, with maximum levels reached in approximately two weeks. On average, patients taking 40-80 mg of oral prednisone experience a WBC count increase of around 4,000/mm3. However, there is a high degree of variability, which may be partly due to differences in glucocorticoid dosage.
Key Message : What are bands? Bandemia, also known as a left shift, refers to an increase in the number of immature neutrophils called "bands" in the bloodstream. Neutrophils are a type of white blood cell (WBC) that play a crucial role in the immune system's defense against infections, particularly bacterial infections. It is worth noting that when the body faces an infection, it responds by increasing the production of neutrophils in the bone marrow. During this rapid phase of neutrophil production, a higher number of immature neutrophils are released into the general circulation. Indeed, these immature neutrophils are characterized by their nonsegmented, band-like nuclei, hence the name "bands." In a normal WBC differential, the percentage of bands is low, usually less than 6% of the total neutrophil count. However, when the body is fighting an infection or facing other inflammatory conditions, the percentage of bands may increase significantly. A left shift, or bandemia, is observed in a complete blood count (CBC) with a differential. This term originates from the historical practice of manually counting different types of white blood cells on a blood smear under a microscope. The various types of white blood cells were placed in columns, with the immature neutrophils (bands) on the left and the more mature neutrophils on the right. An increase in the number of bands, or immature neutrophils, was referred to as a "shift to the left." Bandemia or left shift is an important clinical indicator, as it often suggests an ongoing infection or inflammation that requires further investigation and appropriate medical intervention.
Mechanisms of Steroid induced Leukocytosis
The main mechanisms by which steroids increase WBC count are:
First, steroids cause neutrophils to detach from the endothelial surface of blood vessels. This process, called demargination, increases the number of neutrophils circulating freely in the blood, leading to an elevated WBC count.
Also, steroids slow down the process by which neutrophils migrate from the blood vessels into the tissues. This delay in transmigration results in a higher number of neutrophils remaining in the bloodstream, contributing to the increase in WBC count.
Furthermore, steroids can prolong the life of neutrophils by delaying apoptosis or programmed cell death. As a result, the overall number of neutrophils in circulation increases.
Finally, they can stimulate the bone marrow to produce and release more neutrophils, including immature neutrophils called "bands." This increased production and release of neutrophils lead to a higher WBC count.
Understanding the Clinical Implications of Glucocorticoid-Induced WBC Count Increase
In summary, glucocorticoids are known to increase WBC count, primarily due to a rise in PMNs. The primary factors contributing to this increase are demargination, delayed transmigration, delayed apoptosis, and an increase in the release of neutrophils from the bone marrow. A thorough understanding of these biological processes is essential for the proper interpretation of WBC count changes, especially when glucocorticoids are part of a patient's treatment regimen.
Monitoring and Managing WBC Count in Glucocorticoid-Treated Patients
It is important to closely monitor the WBC count of patients undergoing glucocorticoid therapy, as elevated levels may be misinterpreted as an indication of infection, potentially leading to unnecessary antibiotic treatment. In some cases, however, glucocorticoid-induced leukocytosis may mask an underlying infection. Therefore, clinicians should carefully consider the patient's clinical presentation and overall health status when evaluating changes in WBC count.
It is also essential to manage the potential side effects of glucocorticoids, such as immunosuppression, increased risk of infection, and adrenal insufficiency. Patients on long-term glucocorticoid therapy should be educated about the importance of reporting any signs of infection or other health concerns to their healthcare provider. Additionally, the healthcare team should regularly reassess the patient's glucocorticoid dosage and consider tapering the dose or discontinuing the medication if appropriate.
Conclusion
Glucocorticoids play a significant role in increasing WBC count, primarily through the elevation of PMNs. Understanding the factors behind these changes and their clinical implications is crucial for healthcare professionals when evaluating and treating patients receiving glucocorticoids. Close monitoring of WBC count and a comprehensive understanding of the patient's clinical presentation can ensure that the most appropriate diagnostic and therapeutic decisions are made, ultimately leading to improved patient outcomes.
References
Dale DC, Fauci AS, Guerry D IV et al. Comparison of agents producing a neutrophilic leukocytosis in man. Hydrocortisone, prednisone, endotoxin, and etiocholanolone. J Clin Invest 1975;56:808-13.
Nakagawa M, Terashima T, D'yachkova Y et al. Glucocorticoid-induced granulocytosis: contribution of marrow release and demargination of intravascular granulocytes. Circulation 1998;98:2307-13.
Kindly Let Us Know If This Was helpful? Thank You!


