Indication for the Water Deprivation
Diabetes Insipidus, characterized by polyuria and polydipsia, is a challenging endocrinological condition to accurately diagnose due to the overlap of clinical presentations with other disorders in the polyuria-polydipsia spectrum. In this context, the water deprivation test has long held its position as a cornerstone diagnostic tool, providing critical insights into the body’s regulation of fluid balance and aiding in the differentiation of central, nephrogenic, and primary polydipsia conditions.
Test Preparation
- Standard practice dictates patients abstain from oral intake (NPO) after their evening meal or midnight. However, in patients with severe polyuria, the NPO initiation is recommended in the early hours of the test day, around 6 am. Furthermore, if previously administered, desmopressin must be discontinued at least 24 hours before the test.
- Gold topped-tubes are required for assessing serum sodium and osmolarity.
Role of AVP in water conservation
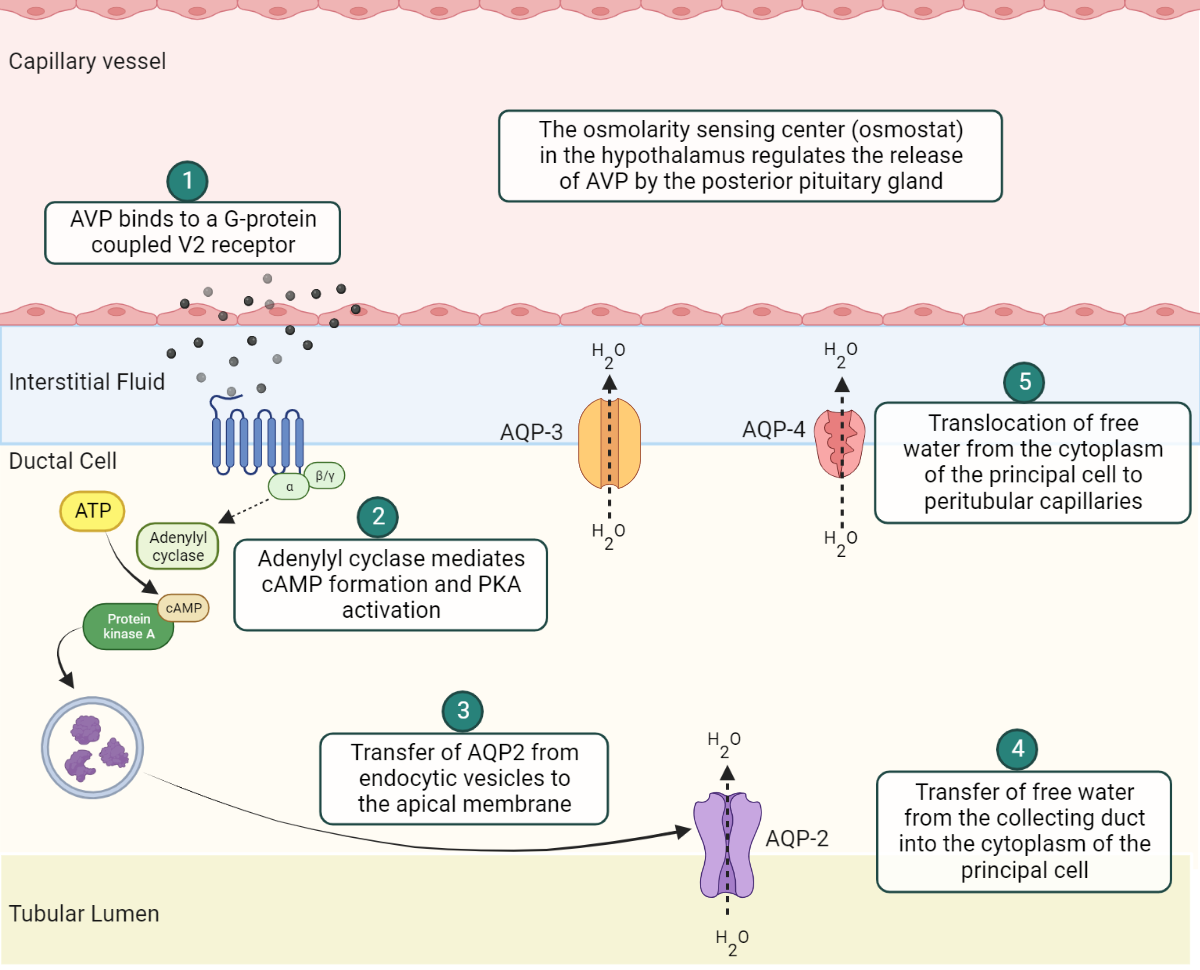
AVP connects to V2 receptors that are coupled with G-proteins, located on the basolateral membrane (BM) of the principal cell. This binding sparks a series of internal cell activities that includes the production of cyclic adenosine monophosphate (cAMP) via adenylyl cyclase and the subsequent activation of protein kinase A (PKA). Following this, PKA stimulates the discharge of aquaporins from the endocytic vesicles. Among these, aquaporin-2 (AQP2) relocates to the apical membrane (AM) of the collecting duct from the vesicles. This relocation facilitates the movement of free water from the collecting duct into the principal cell’s cytoplasm. Meanwhile, aquaporin-3 (AQP3) and aquaporin-4 (AQP4), permanent fixtures of the BM (meaning, they don’t come from endocytic vesicles), assist the final transfer of water from the cytoplasm into the peritubular capillaries.
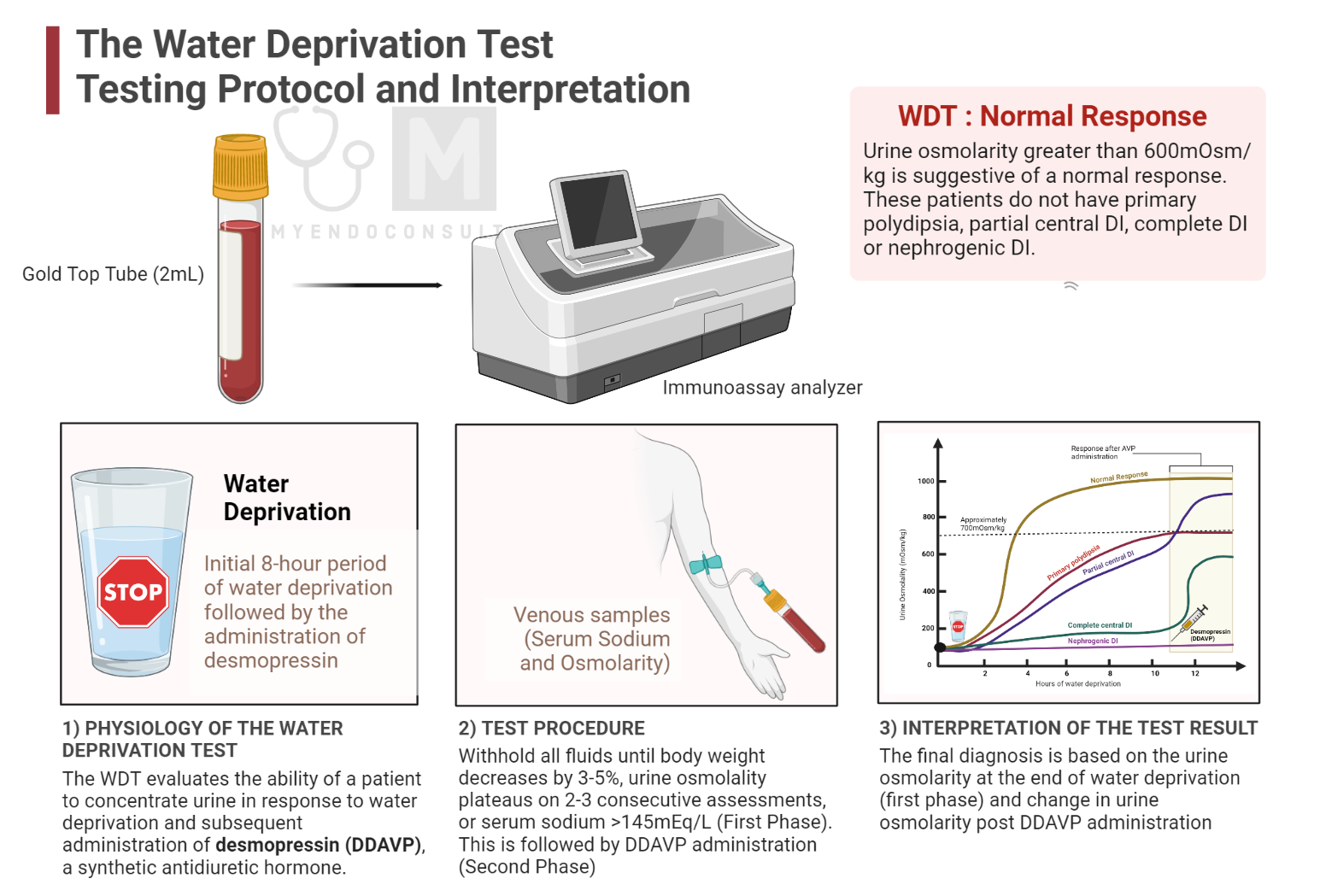
Physiologic principles: Water Deprivation Test
The water deprivation test serves as a diagnostic method to differentiate between central diabetes insipidus (CDI) and nephrogenic diabetes insipidus (NDI), both of which cause excessive urination (polyuria) and extreme thirst (polydipsia) . The fundamental principle is to evaluate the ability of a patient to concentrate urine in response to water deprivation and subsequent administration of desmopressin (DDAVP), a synthetic antidiuretic hormone.
CDI and NDI are characterized by impaired antidiuretic hormone (ADH) secretion or action, respectively. CDI results from inadequate ADH production or release from the posterior pituitary gland, often due to hypothalamic or pituitary gland dysfunction. On the other hand, NDI arises from the kidney’s inability to respond appropriately to ADH action, which can be caused by genetic mutations or specific medications.
Test Procedure
The Water Deprivation Test (WDT) is a widely used diagnostic tool consisting of two steps: an initial 8-hour period of water deprivation followed by the administration of desmopressin, a synthetic antidiuretic hormone. This test is based on the measurement of urine osmolality to assess renal antidiuretic hormone (AVP) action. Dehydration leads to an increase in plasma sodium concentration, which in turn stimulates AVP release. AVP then acts on the kidneys, causing an increase in urine osmolality. If the stimulus for AVP secretion is sufficient, urine osmolality should increase to more than 700 mOsm/kg, differentiating patients with normal vasopressin secretion and function from those with central diabetes insipidus (CDI) or nephrogenic diabetes insipidus (NDI), who cannot concentrate urine during dehydration. However, patients with prolonged significant polyuria of any cause may not concentrate their urine maximally because of chronic polyuria on renal concentrating capacity.
The second part of the test, the administration of desmopressin, is designed to differentiate CDI from NDI. In CDI, a physiological increase in urine osmolality should occur after desmopressin administration. However, different authors have varying opinions on the accepted normal level, ranging from 700 to 800 mOsm/kg. In NDI, urinary concentration remains dilute after desmopressin administration. In cases of diagnostic uncertainty, a hypertonic saline test with AVP or copeptin may be performed.
Formal (inpatient testing)
- Withhold all fluids until body weight decreases by 3-5%, urine osmolality plateaus on 2-3 consecutive assessments, or serum sodium >145mEq/L
- If any of the above criteria are met, administer 1 mcg of dDAVP subcutaneously and assess urine osmolality and volume in 2 hours.
Combined water deprivation test
- Withhold ALL fluids until the patient’s body weight decreases by 3-5%, urine osmolality plateaus on 2-3 consecutive assessments or serum sodium >145mEq/L. If serum sodium is not >145mEq/L at the end, infuse 3% of NaCl (0.1ml/kg/min) for 1 to 2 hours until serum sodium is >145mEq/L.
- Draw plasma AVP level, plasma osmolality, and urine osmolality both at the beginning and conclusion of the test, then administer 1mcg of dDAVP subcutaneously. Subsequently, measure urine osmolality and volume for 2 more hours.
- Compare baseline and post-water deprivation AVP levels in relation to plasma and urine osmolarities in order to distinguish between central and nephrogenic diabetes insipidus.
Interpretation of the Water Deprivation Test
Initial Phase of the Water Deprivation Test
Urine osmolarity greater than 600mOsm/kg is suggestive of a normal response. These patients do not have primary polydipsia, partial central DI, complete DI or nephrogenic DI.

Second phase of the test (DDAVP administration)
- If urine osmolality increases >50% after dDAVP administration, this suggests a diagnosis of central diabetes insipidus.
- If urine osmolality increases <10% after dDAVP administration, this suggests a diagnosis of nephrogenic diabetes insipidus.
- If urine osmolality increases between 10-50% (intermediate response) after dDAVP administration, this suggests an equivocal test (additional testing required)
Table 1. Summary of the water deprivation test
| Clinical Parameter (mOsm/Kg) | Polydipsia | Central DI (complete) | Central DI (partial) | Nephrogenic DI |
| Serum Osmolality (baseline) | <295 | >300 | >300 | >300 |
| Urine Osmolality (first phase) | 400-600 | <300 | 400-600 | <300 |
| Response to DDAVP (second phase) | Mild to no response | 400-600 | >600 | No response |
References
- Tomkins M, Lawless S, Martin-Grace J, Sherlock M, Thompson CJ (2022) Diagnosis and Management of Central Diabetes Insipidus in Adults. The Journal of Clinical Endocrinology & Metabolism 107:2701–2715
- Robertson GL (1995) Diabetes insipidus. Endocrinol Metab Clin North Am 24:549–572
- Christ-Crain M, Bichet DG, Fenske WK, Goldman MB, Rittig S, Verbalis JG, Verkman AS (2019) Diabetes insipidus. Nat Rev Dis Primers 5:54
- Verbalis JG (2003) Diabetes Insipidus. Rev Endocr Metab Disord 4:177–185
- Kavanagh C, Uy NS (2019) Nephrogenic Diabetes Insipidus. Pediatr Clin North Am 66:227–234
Kindly Let Us Know If This Was helpful? Thank You!


