In this article, we will review the ACTH (cortrosyn) stimulation test in both the diagnosis of adrenal insufficiency and nonclassic congenital adrenal hyperplasia. Recent changes to the cutoff limits of the cortisol assay and optimal testing conditions will be covered.
The ACTH (cortrosyn) stimulation test is performed to determine if the adrenal glands can respond appropriately to exogenous ACTH.
In patients with primary adrenal insufficiency, serum cortisol is low in the setting of elevated adrenocorticotropic hormone levels. Furthermore, the 24-hour urinary cortisol excretion is low in patients with adrenal insufficiency.
A helpful rule of thumb is that in symptomatic patients, an 8 am serum ACTH concentration greater than 500 pg/mL and a concomitant serum cortisol concentration less than 5 μg/dL is diagnostic of primary adrenal insufficiency. In this setting, an ACTH stimulation test is unnecessary.
How is the ACTH (Cortrosyn) Stimulation Test Performed?
In preparing for this test, patients should be instructed to hold off glucocorticoids for at least 24 hours before the test since common exogenous steroids such as hydrocortisone and prednisone are detectable on the cortisol assay.
There are some additional caveats in performing this test.
- It is essential to understand the role of binding proteins on total cortisol assessment. Total cortisol, which is the form of cortisol measured on most immunoassays, is estimated based on this equation. Total cortisol is equal to free cortisol plus bound cortisol. Forms of binding proteins for cortisol include corticosteroid binding globulin (CBG) and albumin. Consequently, clinical states that alter these binding proteins can affect the measured value of total cortisol in plasma. Oral estrogen increases corticosteroid-binding globulin, which results in the elevation of total cortisol levels. The mechanism is beyond the scope of this video.
- Patients with low serum albumin (usually below 2.5 grams per dL) will have low total cortisol. This is because albumin is a major binding protein for cortisol.
- So can the cortrosyn stimulation test differentiate between primary and secondary adrenal insufficiency? The answer is NO! It is simply a test to evaluate the ability of the adrenal glands to respond to exogenous ACTH stimulation. Although the test has a high specificity for both primary and secondary adrenal insufficiency, it has a very low sensitivity for secondary adrenal insufficiency. This is because, within three months of developing secondary adrenal insufficiency, the adrenal cortex remains responsive to exogenous ACTH stimulation. For this reason, even if a patient has secondary adrenal insufficiency, the ACTH (cortrosyn stimulation test) may return falsely negative within the first few months of developing adrenal insufficiency. This is because although there is no obvious ACTH stimulation of cortisol production in secondary adrenal insufficiency, the adrenal cortex may take up to three months to develop significant atrophy. Consequently, when exogenous steroids are administered, the adrenal cortex continues to maintain a sufficient response
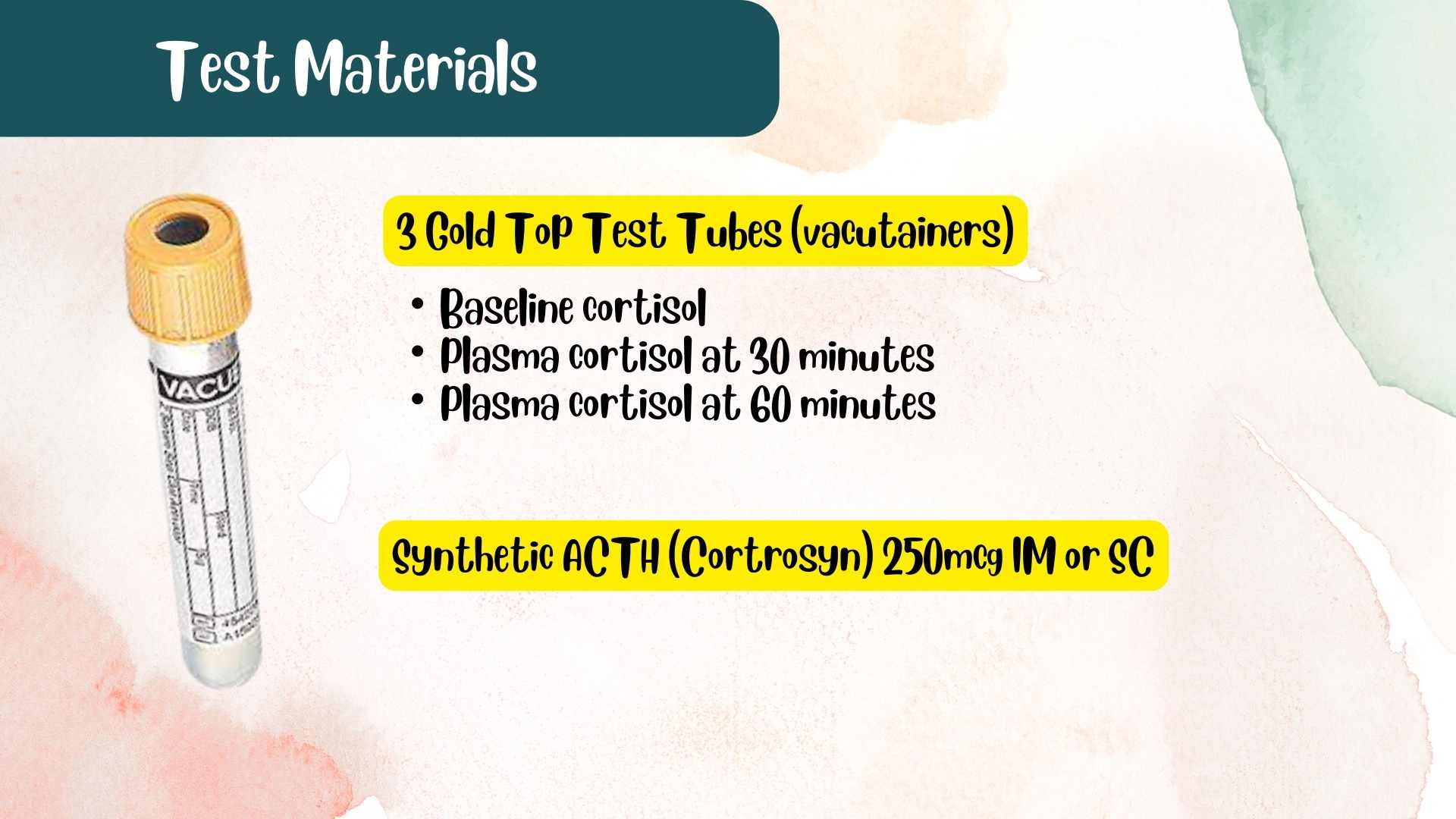
The materials needed for the test include three gold top tubes. They should be labeled for the collection of serum cortisol at baseline, 30 and 60 minutes.
- This test can be performed in either the outpatient or inpatient setting.
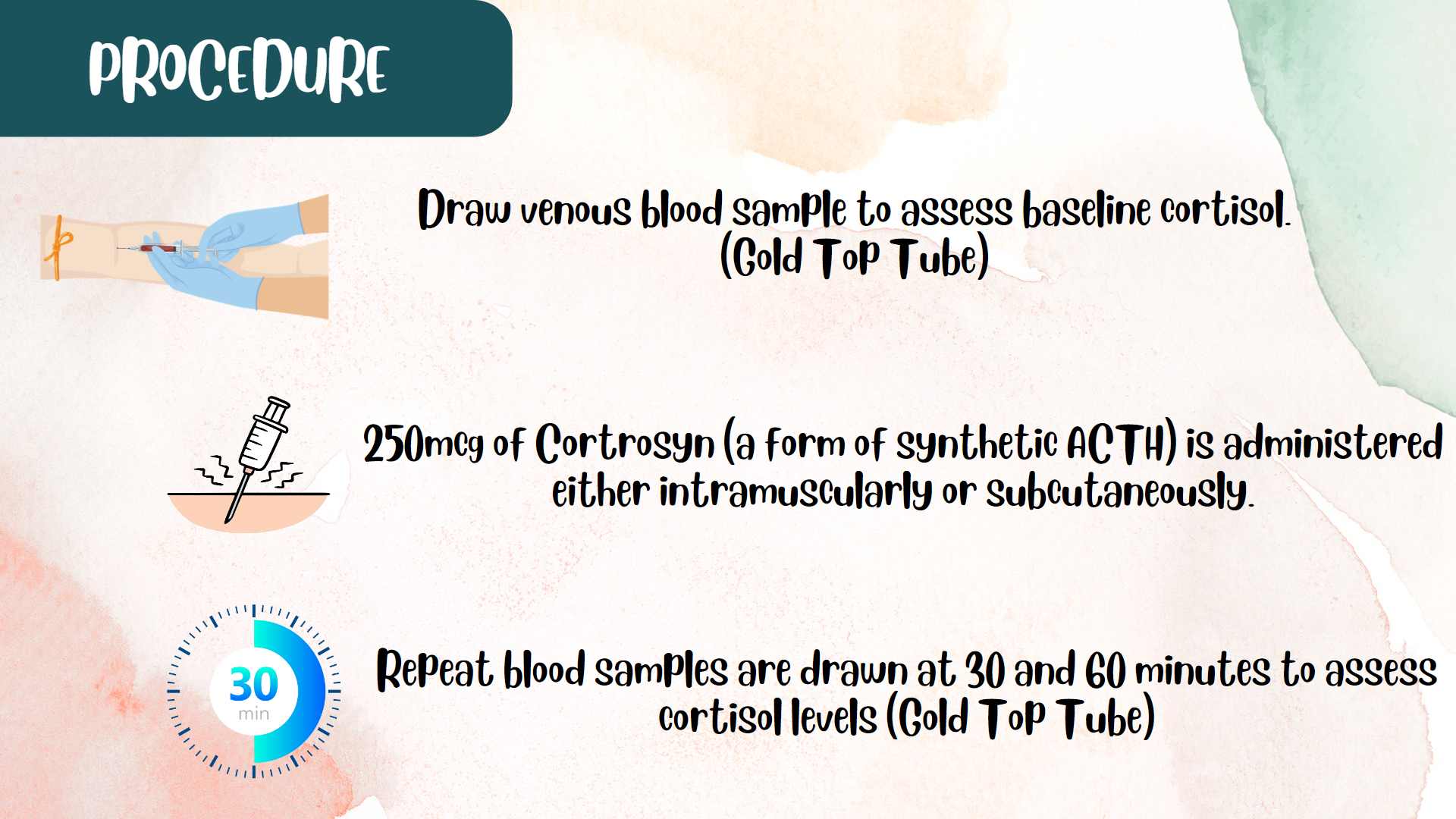
- A venous blood sample is drawn to assess baseline cortisol.
- 250mcg of Cortrosyn (a form of synthetic ACTH) is administered either intramuscularly or subcutaneously.
- Repeat blood samples are drawn at 30 and 60 minutes.
ACTH Stimulation Test interpretation
- A normal response shows a peak stimulated cortisol value > 18 mcg/dl at either 30 or 60 minutes.
- When the cosyntropin-stimulation test is performed in patients with primary adrenal failure, the serum cortisol concentration does not change from baseline (the baseline value is typically <5 μg/dL, and the increment after cosyntropin administration is <7 μg/dL), and the peak value remains below 18 μg/dL.
- In secondary adrenal insufficiency, the increment after cosyntropin administration is <7 μg/dL), and the peak value remains below 18 μg/dL.
The traditionally accepted cutoff value for post-stimulation cortisol, that is, 18mcg per dl, was based on polyclonal antibody-based immunoassays. In recent times, immunoassays such as the Roche Elesys II assay is based on a monoclonal antibody with a much lower detection limit for cortisol. Consequently, when using these newer assays, the acceptable post-stimulation cortisol level, especially at 60 minutes, is anywhere from 14 to 15 mcg/dL and not the traditional cutoff of 18 mcg per dl.
As you may recall, low serum albumin can artifactually reduce the measured total cortisol. For patients with expected low total cortisol, such as those with chronic liver disease, free cortisol (instead of total cortisol) should be measured at baseline, 30 and 60 minutes. A normal response is a peak-stimulated free cortisol value greater than 1.2 mcg per dL at either 30 or 60 minutes.
Cortrosyn stimulation test in nonclassic CAH
This is not exactly the end of the clinical utility of this test since it is also a screening test for 21 hydroxylase deficiency, a cause of nonclassic congenital adrenal insufficiency. This is a milder form of congenital adrenal hyperplasia which may result in oligomenorrhea, infertility, and hirsutism in women.
The test is best performed in the early follicular phase of the menstrual cycle in women being investigated for hyperandrogenemia. Also, oral contraceptive pills should be discontinued for at least 8 weeks before the test.
- In this test, both 17 hydroxyprogesterone and cortisol are drawn at baseline. 250mcg of cortrosyn is then administered intramuscularly. Samples of 17 hydroxyprogesterone and cortisol are then drawn at 60 minutes.
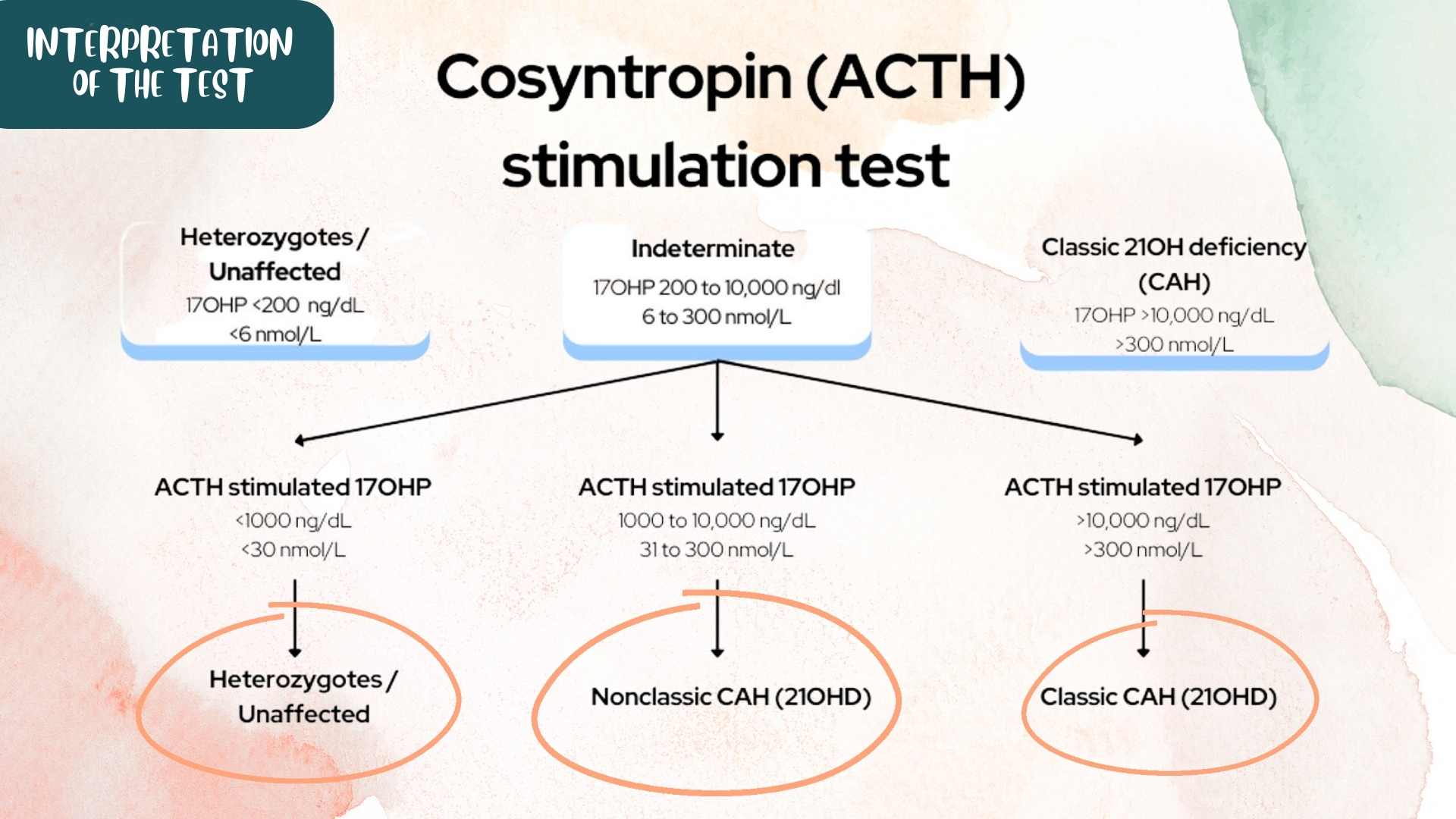
- If the basal 17 hydroxyprogesterone is less than (or 200ng per dl), the diagnosis is highly unlikely as such an ACTH test is not necessary in this setting.
- If basal 17 hydroxyprogesterone is greater than 10,000 ng/ml (or 1000 ng per dl), this is highly suggestive of classic 21 hydroxylase deficiency and not the nonclassic 21 hydroxylase deficiency of late-onset congenital adrenal hyperplasia.
- For patients with basal 17 hydroxyprogesterone between 200 ng/ml and 10,000 ng/ml, then an ACTH stimulation test will be required.
ACTH stimulation test interpretation in nonclassic CAH
For patients with nonclassic CAH, a value of 17-hydroxyprogesterone at 60 min sample between 1000 to 10,000 ng/dl is diagnostic.
If the stimulated 17-hydroxyprogesterone at 60 min sample is less than 1000 ng/dl, then the patient is either a heterozygote or is unaffected.
If the stimulated 17-hydroxyprogesterone at 60 min sample is greater than 10,000 ng/dl, then the patient has classic 21 hydroxylase deficiency.
I hope you found this article on the ACTH stimulation test helpful.
Kindly Let Us Know If This Was helpful? Thank You!


