In this article, a brief historical timeline of discoveries in thyroid anatomy, the embryology, gross anatomy and histology of the thyroid gland will be reviewed.
Historical timeline of discoveries in thyroidology.
- 1543 Vesal described the thyroid gland.
- 1606 Paracelsus related cretinism to the thyroid gland (published posthumously).
- 1786 Parry described hyperthyroidism (published posthumously 1825).
- 1802 Flaiani described hyperthyroidism.
- 1820 Coindet introduced iodine into the treatment of goiter.
- 1833 Boussingault recommended iodine for the prevention of goiter.
- 1835 Graves described hyperthyroidism.
- 1836 King assumed the presence of an internal secretion of the thyroid.
- 1840 Basedow gave a classic description of the Merseburg triad (exophthalmos, goiter and tachycardia).
- 1852 Chatin justified the theory that iodine deficiency caused goiter, by proving a diminished iodine content of the drinking water in endemic areas.
- 1873 Gull described the classic picture of myxedema.
- 1878 Ord related it to atrophy of the thyroid gland.
- 1882 First description of the complications of thyroidectomy in man by the Reverdin brothers.
- 1883 Kocher described “cachexia strumipriva” (postoperative myxedema).
- 1886 Moebius found that Graves’ disease was due to hyperfunction of the thyroid gland.
- 1888 Report of the Myxedema Commission of the Clinical Society of London.
- 1891 Murray successfully treated myxedema with injections of thyroid extract.
- 1893 Friedrich Von Muller demonstrated a negative metabolic balance in hyperthyroidism.
- 1895 Magnus-Levy recognized that the oxygen consumption at rest was elevated in thyrotoxicosis and reduced in myxedema and that the basal metabolic rate following the administration of desiccated tissue was increased.
- 1896 Baumann showed that iodine was a constituent of the thyroid gland.
- 1899 Oswald isolated thyroglobulin as a component of the thyroid.
- 1910 Marine and Lenhart succeeded in preventing goiter by using iodine in animal experiments.
- 1912 Gudernatsch recognized the acceleration of metamorphosis caused by thyroxine.
- 1913 Plummer described the toxic adenoma.
- 1914 Kendall succeeded in purifying and crystallizing the thyroid hormone, thyroxme.
- 1917 First successful iodine-prophylaxis of goiter in man by Marine and Kimball.
- 1918 Aub, Dubois, Benedict, and Harris introduced the measurement of basal metabolic rate as a clinical method.
- 1922 Plummer introduced iodine treatment for hyperthyroidism.
- 1926 Harington established the chemical constitution of thyroxine.
- 1927 Harington and Barger synthesized thyroxine.
- 1927 Smith showed the existence of thyrotropin in the pituitary gland.
- 1928 Chesney, Clawson and Webster discovered goitrogenic substances in different types of cabbage.
- 1940 Introduction of radioactive iodine for the clinical evaluation of thyroid function by Hertz, Roberts, Means, and Evans.
- 1942 Astwood systematically examined goitrogenic substances and introduced thiouracil into the treatment of hyperthyroidism.
- 1942 Hamilton and Lawrence introduced radioactive iodine into the treatment of the thyroid gland.
- 1952 Discovery of triiodothyronine by Gross and Pitt-Rivers and Roche, Michel, and Lissitzky.
- 1956 Adams, Purves, and Mckenzie independently found the long-acting thyroid stimulator (LATS) in the serum of thyrotoxic patients.
- 1956 Roitt, Doniach, Campbell, and Hudson discovered thyroid antibodies in Hashimoto
- 1970 Gullemin and Schally successfully isolated thyrotropin releasing hormone (TRH)
- from hypothalamic extracts.
- 1970 Gillessen and co-workers established the chemical constitution of TRH and synthesized the hormone.
Embryology of the Thyroid Gland
The thyroid gland appears very early in embryonic life. In the human embryo (approximately 3.5 to 4 mm in length), an entodermal outpocketing forms in the floor of the oral cavity, just beneath the buccopharyngeal membrane and between the first pair of pharyngeal pouches.
At the bottom of this small pit, an epithelial bud protrudes into the underlying mesenchyma. The primordium becomes displaced caudally, but remains attached to the floor of the pharynx by the thyroglossal duct.
During its descent, the originally compact bud becomes bilobed and differentiates into a mass of irregularly arranged epithelial cords, which later form the isthmus and the lateral lobes of the gland.
When the primordium reaches the level of the uppermost tracheal cartilage, the thyroglossal duct becomes fragmented (involutes). A cranial fragment, the lingual duct, remains attached to the tongue initially but usually disappears at later stages. Occasionally however, salivary gland-like structures and small colloid-filled follicles develop from its epithelium.
Clinical Pearl
Persistent fragments of the thyroglossal duct may develop into fluid filled pockets known as thyroglossal cysts. These can become infected in later life or even undergo malignant transformation.
The point of origin of the duct forms the foramen cecum, an enlarged pit which persists, in about 50 % of the population, in the midpoint of the sulcus terminalis between dorsum and radix linguae.
The distal fragment of the thyroglossal duct gives rise to the pyramidal lobe. In the eighth week, small rounded or elongated cavities begin to appear in the thyroid cords. They develop into the primary thyroid follicles, which acquire colloid at the beginning of the third gestational month and become functional soon afterwards.
Gross Anatomy of the Thyroid Gland
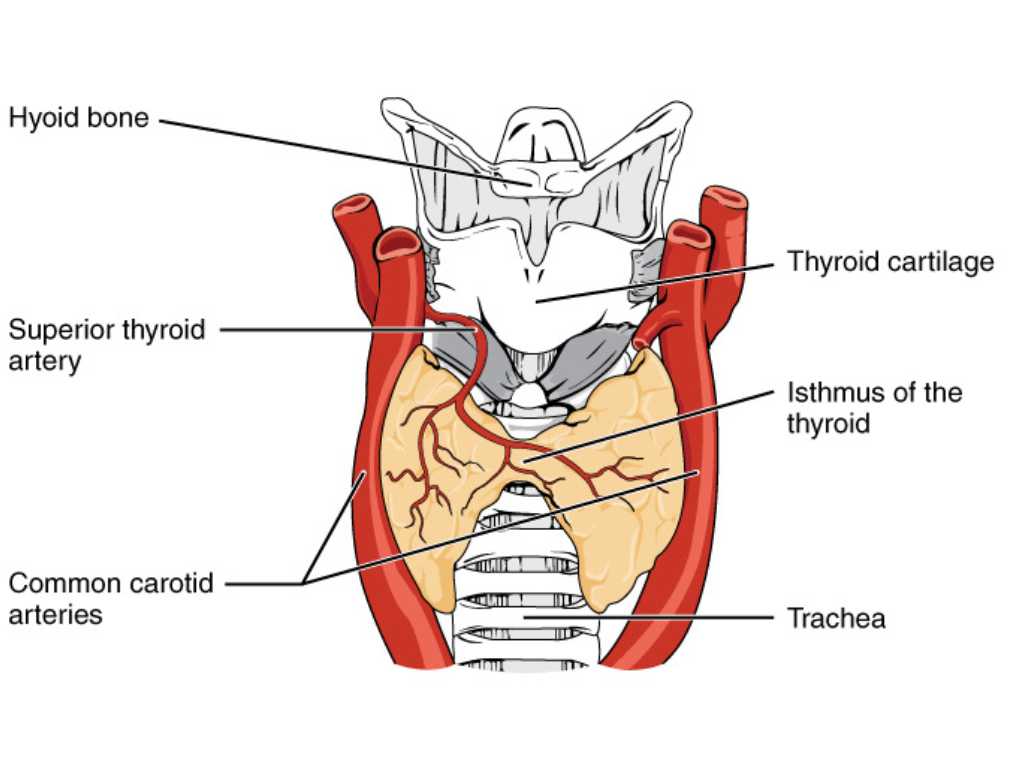
The thyroid gland consists of a left and a right lobe which are connected across the median plane by the narrow isthmus.
The lateral lobes are conical in shape. The base is usually on a level with the fourth or fifth tracheal ring. The apex, which is directed upwards, usually reaches the oblique line of the thyroid cartilage. The isthmus usually covers the second and third tracheal rings, but may also be higher or lower.
The pyramidal lobe varies widely in size and shape, occasionally extending up to the hyoid bone. The gland is situated at the level of the fifth to seventh cervical and the first thoracic vertebrae.
Surgical Pearl
Ligation of the inferior thyroid arteries during thyroidectomy therefore involves some hazard to the recurrent laryngeal nerve.
Its medial surface is in close contact with the larynx and trachea. Its posterolateral surfaces are related to the esophagus and the neurovascular tracts of the neck.
Anteriorly, the thyroid is separated from the sternothyroid muscles by the pretracheal fascia. A connective tissue capsule is closely applied to and inseparable from the glandular parenchyma. An additional, outer and thicker capsule encloses the larger branches of the thyroid blood vessels and the parathyroid glands.
Small aberrant fragments of thyroid tissue are sometimes found outside this outer capsule, mostly along the obliterated thyroglossal duct (so-called accessory thyroid glands). It is worth noting that the thyroid gland is indeed a highly vascular organ.
It is usually supplied by two pairs of arteries, the branches of which anastomose freely with each other within the parenchyma of the thyroid gland.
The superior thyroid artery arises on each side as the first branch of the external carotid. It supplies the upper, anterior, and lateral portions of the lateral lobes.
The inferior thyroid artery is a branch of the thyrocervical trunk which also arises from the first portion of the subclavian artery. It supplies the inferior, posterior and medial parts of the organ on either side.
In its course to the thyroid gland, the inferior thyroid artery crosses the recurrent laryngeal nerve of the vagus and the sympathetic trunk, which often forms a loop around it (an anatomical structure known as the ansa thyreoidea).
The recurrent laryngeal nerve ascends, on the left side, in a groove between the trachea and the esophagus (also known as the tracheoesophageal groove), and, on the right side, along the trachea.
At the level of the first tracheal ring, it gives off the inferior laryngeal nerve which runs in front of, or behind the branches of the inferior thyroid artery to supply the intrinsic muscles of the larynx.
Occasionally, there is a fifth artery, the unpaired arteria thyreoidea ima, which arises from the arch of the aorta or from the brachiocephalic trunk and ascends to the isthmus.
The veins form a rich network on the surface of the organ and on the anterior surface of the trachea. From this plexus, a superior, a middle and an inferior thyroid vein arise. The former two end in the internal jugular vein, and the latter in the innominate vein.
A dense capillary network surrounds the thyroid follicles. Closely applied to the capillaries are numerous branching lymph vessels which run in the interfollicular connective tissue, often along the arterioles, to a network in the capsule of the gland. From here, larger lymph vessels extend to the thoracic duct and to the right lymphatic duct.
Numerous autonomous nerve fibers derived from the middle and inferior cervical ganglia of the sympathetic trunk penetrate the thyroid capsule, mostly together with the arteries.
In the interfollicular spaces, they form a dense network of nonmyelinated nerve fibers, whose endings terminate in close proximity to the follicles.
Histology of the thyroid gland
At an embryonic age of about eight weeks, the epithelial cords of the thyroid primordium disintegrate into small vesicles, the primary or two-cell follicles, which contain small amounts of colloidal material.
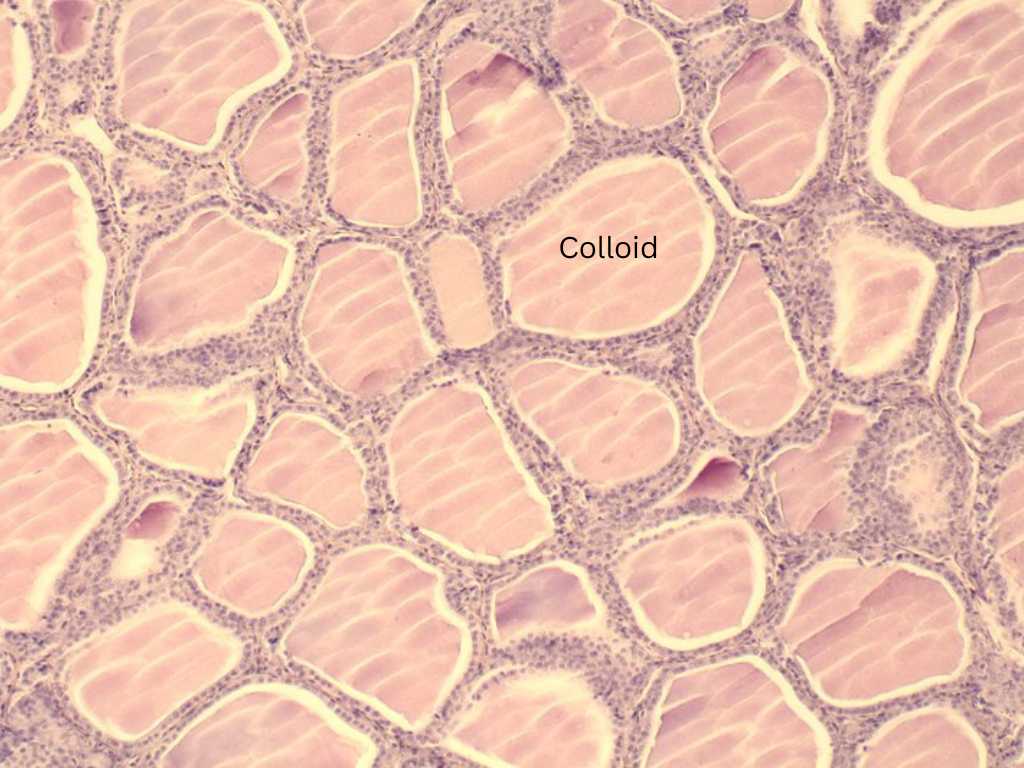 Histological view of thyroid follicular cells showing central colloid. Source: WikiCommons
Histological view of thyroid follicular cells showing central colloid. Source: WikiCommonsFrom these, rounded or rod-shaped secondary (definitive) follicles sprout out and enlarge. The follicles of the mature gland measure up to 1 mm in diameter. They contain a gelatinous colloid and are lined by a simple epithelium, the depth of which varies widely according to the functional state of the gland.
At the peak of secretory activity, the epithelial cells are columnar in shape. Mitochondria and numerous clear vesicles appear to accumulate in the apical portions of the cells and the Golgi complex is found in a supranuclear position. The colloid produced in the cells is secreted into the follicle cavity, where it gradually becomes concentrated. At this point, the epithelial cells assume a cuboid or flattened shape corresponding to a resting state.
Resorption of the colloid from its storage site seems to be initiated by liquefaction of its outermost portions. The cells again become cuboidal or columnar and their cytoplasm turns foamy. Empty follicles are characterized by their star-shaped lumen.
It is assumed that they are able to refill the follicle cavity with colloid within a few hours. Each follicle is enclosed by a very thin basal membrane and a delicate network of reticular fibers.
In addition, it is surrounded by a capillary plexus and by numerous blind terminations of lymphatic vessels. The interstitial arterial network of the thyroid gland is rich in regulatory structures such as subendothelial bundles of epitheloid muscle cells, as well as arteriovenous anastomoses.
Veins and larger lymphatics accompany the arteries. A large number of sympathetic nerve fibers originate in the middle and superior cervical ganglia and run along the larger blood vessels; they are presumed to be vasomotor.
A population of larger cells which do not stain as well is regularly observed in both the follicular epithelium and the interfollicular spaces. When stained by the silver nitrate method these parafollicular cells (mitochondria- rich cells, C cells) display a large number of small brown or black granules. Indeed, these parafollicular cells produce the hormone calcitonin.
Electron microscopy reveals a large number of microvilli and occasional single cilia at the apical surface of the epithelial cells. Their shape varies widely according to the functional state of the follicle. The microvilli of resting cells are short and straight; those of secreting or resorbing cells appear larger and pleomorphic.
Laterally, the follicle cells are joined by typical junctional complexes. Some small infoldings of the plasma membrane are regularly observed in the basal regions of the epithelium. In the active cell, the Golgi apparatus is composed of flattened saccules and numerous vesicles and vacuoles.
It is usually situated above the relatively large nucleus which occupies the basal cytoplasmic region. The endoplasmic reticulum consists of elongated, rough-surfaced cisternae and a large number of small vesicles. Ovoid or rounded mitochondria, multivesicular bodies, and vacuoles of varying size are randomly distributed within the cytoplasmic ground substance.
References
- Beynon ME, Pinneri K. An Overview of the Thyroid Gland and Thyroid-Related Deaths for the Forensic Pathologist. Acad Forensic Pathol. 2016 Jun;6(2):217-236
- Hoyes AD, Kershaw DR. Anatomy and development of the thyroid gland. Ear Nose Throat J. 1985 Jul;64(7):318-33. PMID: 3837720.
- Prakash, Rajini T, Ramachandran A, Savalgi GB, Venkata SP, Mokhasi V. Variations in the anatomy of the thyroid gland: clinical implications of a cadaver study. Anat Sci Int. 2012 Mar;87(1):45-9.
- Fancy T, Gallagher D 3rd, Hornig JD. Surgical anatomy of the thyroid and parathyroid glands. Otolaryngol Clin North Am. 2010 Apr;43(2):221-7, vii.
Kindly Let Us Know If This Was helpful? Thank You!


