In patients with diabetes mellitus, glycated hemoglobin (HbA1c) and plasma glucose (random or fasting) are typically utilized in monitoring patient response to treatment. Although these conventional monitoring tools for diabetes mellitus are reliable, there may be unique clinical scenarios in which their application is limited.
For example, glycated hemoglobin is unreliable in various conditions that affect red blood cell turnover (glycated hemoglobin (HbA1c) may be falsely elevated or, in some cases, falsely low). Fructosamine, which is a product of non-enzymatic glycation of plasma proteins (e.g., albumin, globulins, and lipoproteins), can be utilized in the evaluation diabetes control.
A1c fructosamine conversion calculator
Origin of the A1C to Fructosamine calculator
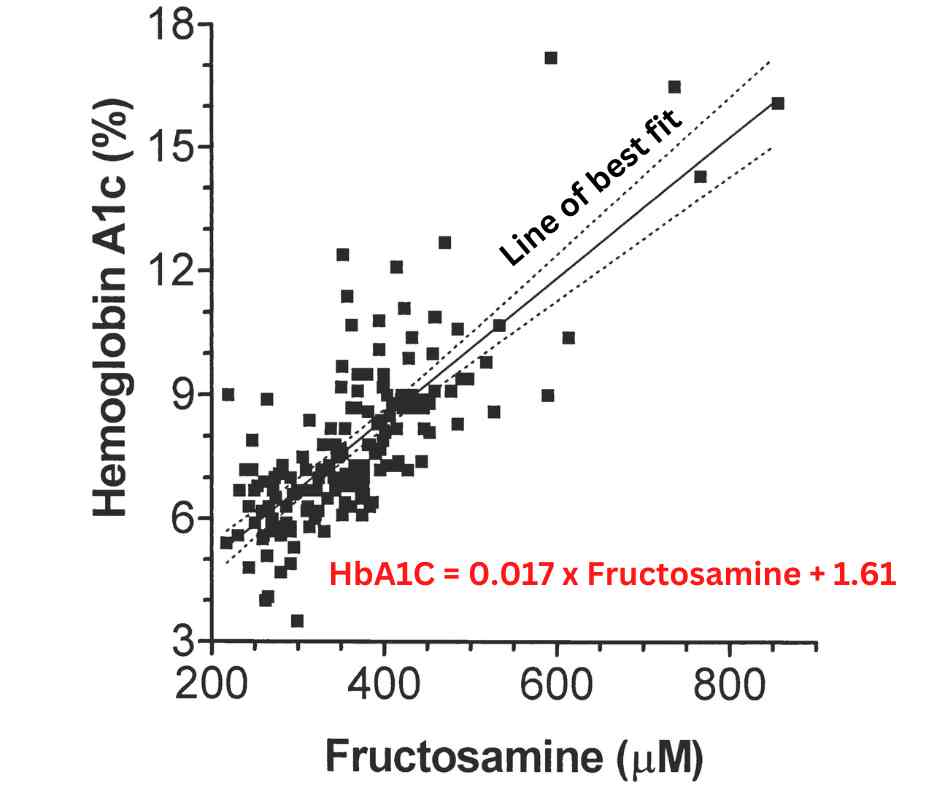
Figure 1. Linear regression equation based on Cohen et al “Discordance between HbA1C and Fructosamine: Evidence for a glycosylation gap and its relation to diabetic nephropathy”
The Equation is based on a study by Cohen et al titled “Discordance between HbA1C and Fructosamine : Evidence for a glycosylation gap and its relation to diabetic nephropathy”
The authors estimated both HbA1C and fructosamine in 153 patients with a mean age of 47 years, of which 46% had type 1 diabetes and 47% type 2 diabetes. A plot of measured HbA1C was compared to measured fructosamine. The regression line for the cohort was HbA1C = 0.017 x Fructosamine + 1.61. The r value was 0.78.
Formula Fructosamine to HbA1C conversion
HbA1c = 0.017 X fructosamine level (mmol/L) + 1.61
Fructosamine to a1c conversion chart
| Glucose (mg/dl) | A1C% | Fructosamine (Alarcon et al) | Fructosamine (Cohen et al) |
|---|---|---|---|
| 90 | 5 | 212.5 | 199.4 |
| 120 | 6 | 250 | 258.2 |
| 150 | 7 | 287.5 | 317.03 |
| 180 | 8 | 325 | 375.85 |
| 210 | 9 | 362.5 | 434.67 |
| 240 | 10 | 400 | 493.49 |
| 270 | 11 | 437.5 | 552.32 |
| 300 | 12 | 475 | 611.13 |
| 330 | 13 | 512.5 | 670 |
| 360 | 14 | 550 | 728.77 |
| 390 | 15 | 587.5 | 787.6 |
Formula for HbA1C to Fructosamine conversion
Fructosamine (mmol/L) = (HbA1c – 1.61) x 58.82
What is fructosamine?
Fructosamine is the product of the nonenzymatic glycation of protein (glucose bound to protein). It should be seen as an umbrella term for circulating proteins that have undergone glycation. Albumin, the predominant circulating protein, is measured in the fructosamine assay, although it can also be independently measured as “glycated albumin”
In contrast to glycated hemoglobin, which may be valid for assessing glycemic control up to the preceding three months before the test, the glycated albumin (or fructosamine) is only valid for the preceding three weeks.
Unfortunately, fructosamine, just like glycated hemoglobin, is also subject to various limitations. The result is unlikely to be reliable in hypoproteinemic states (nephrotic syndrome, severe liver disease, protein-energy malnutrition, protein-losing enteropathy), pregnancy, uremia, or hyperlipidemia.
Current Diagnostic Criteria for Diabetes
The current diagnostic criteria involve the utilization of either plasma glucose or glycated hemoglobin in establishing the diagnosis of diabetes mellitus. Although fructosamine is not an accepted tool in diagnosing diabetes mellitus, it can be used for monitoring the disease in clinical scenarios where the clinician expects limited utility of glycated hemoglobin.
- Glycated hemoglobin (HbA1c) value ≥6.5% (i≥48 mmol/mol)
- Fasting plasma glucose (FPG) ≥126 mg/dL ( ≥7.0 mmol/L)
- 2-hour plasma glucose ≥200 mg/dL ( ≥11.1 mmol/L) after an oral glucose tolerance test (OGTT) using a 75 g anhydrous glucose load
- Random plasma glucose ≥200 mg/dL (≥11.1 mmol/L) in the setting of hyperglycemic symptoms (polyuria, polydipsia, unintentional weight loss).
Current diagnostic criteria for prediabetes
Prediabetes is a progressive and highly variable clinical entity that leads almost universally to diabetes mellitus if left untreated.
- HbA1c range of 5.7-6.4% (39-46 mmol/mol)
- Fasting plasma glucose between 100-126 mg/dL (5.6-6.9 mmol/L)
- 2-hour plasma glucose between 140-199 mg/dL (7.8-11.0 mmol/L) after an oral glucose load (75grams of anhydrous glucose)
Monitoring of diabetes mellitus
For nonpregnant adults, the goal of diabetes treatment is to aim for the following glycated hemoglobin and capillary glucose targets.
- HbA1c value <7.0% (<53 mmol/mol)
- Preprandial capillary plasma glucose between 70-130 mg/dL (3.9-7.2 mmol/L)
- Peak postprandial capillary plasma glucose <180 mg/dL (<10.0 mmol/L).
Conditions that can affect the clinical utility of glycated hemoglobin
A simple rule of thumb for recalling the causes of either falsely high or low glycated A1c is to recognize the conditions that alter the life span of red blood cells. Since glycated hemoglobin measures how long the red blood cell is exposed to continuing glycation in the setting of significant hyperglycemia, conditions that alter the life span of a red blood cell can impact the final value of this diagnostic test.
Patients with blood loss, either acutely or chronically, experience a depletion of red blood cells, which will falsely lower glycated hemoglobin. A similar scenario occurs in patients with hemolytic anemia. Since the spleen is important in the clearing of old (senescent) red blood cells, in patients with a large spleen, a state of “hypersplenism” occurs whereby red cells are removed from circulation at a much faster rate than usual. This also causes a falsely low glycated hemoglobin.
Red blood cell transfusion can lead to a falsely high glycated hemoglobin if it is stored in a high dextrose-containing medium or low due to a delusional of circulating red blood cells. To further complicate matters, hemoglobin variants and significant vitamin C ingestion may result in either falsely high or low A1c depending on the assay technique.
Falsely high A1c | Falsely low A1c |
Decreased red cell turnover (iron, B12, or folate deficiency) | Acute (e.g., hemolysis of variable etiology) or chronic blood loss anemia |
Splenectomy (spleen clears senescent erythrocytes) | Splenomegaly (storage diseases, infections, etc.) |
Uremia (false detection of carbamyl-hemoglobin) | End-stage renal disease (chronic anemia, decreased red cell survival due to uremic toxicity) |
Hypertriglyceridemia | Hypervitaminosis E (impairs glycation) |
Hyperbilirubinemia | Ribavirin (hemolytic anemia) |
Hyperglycation (physiologic variant) | Pregnancy (decreased red cell lifespan, dilutional effect, especially in the second trimester and increased erythropoietin production) |
Chronic opioid dependence | |
Lead toxicity | |
Alcohol abuse disorder |
Since glycated hemoglobin A1c is fraught with various limitations, in certain clinical situations the use of an alternative method of monitoring diabetes mellitus may be required.
What is Hemoglobin A1c?
References
- Radin MS. Pitfalls in hemoglobin A1c measurement: when results may be misleading. J Gen Intern Med. 2014 Feb;29(2):388-94.
- Wendy O. Henderson, MD, Mary H. Parker, PharmD, FASHP, FCCP, BCPS, BCCP and Bryan C. Batch, MD, MHS. Cleveland Clinic Journal of Medicine February 2021, 88 (2) 81-85
- Robert M. Cohen, Yancey R. Holmes, Thomas C. Chenier, Clinton H. Joiner; Discordance Between HbA1c and Fructosamine: Evidence for a glycosylation gap and its relation to diabetic nephropathy. Diabetes Care 1 January 2003; 26 (1): 163–167.
- Lorena Alarcon-Casas Wright, Irl B. Hirsch; The Challenge of the Use of Glycemic Biomarkers in Diabetes: Reflecting on Hemoglobin A1C, 1,5-Anhydroglucitol, and the Glycated Proteins Fructosamine and Glycated Albumin. Diabetes Spectr 1 August 2012; 25 (3): 141–148.


Hello Leanne, we apologize for any confusion caused by the discrepancies between the results of the fructosamine calculator and the chart. The fructosamine calculator is based on the regression equation or formula estimated by Cohen et al. from a cohort of 153 subjects. However, our initial chart presented the results of a review article by Alarcon-Casas and Hirsch. The fructosamine estimates in that study were based on estimates from older studies. Please, review that article here (https://doi.org/10.2337/diaspect.25.3.141). The revised chart now presents the fructosamine estimates from both articles.
This calculator is based on a formula by Cohen et al., which may differ slightly from the one used in the initial chart (Alarcon-Casas and Hirsch), which could explain the differences in the results. Another reason for the differences in the fructosamine estimates may be that the analytical methods (assays) vary between studies. Ultimately, the formula proposed by Cohen et al. is more widely accepted and serves as the basis for this fructosamine to A1C calculator.
Thanks for your helpful feedback. It will be interesting to hear other clinicians’ experiences regarding the A1C to fructosamine conversion formula.
Hello. I was using the information on this page:
https://myendoconsult.com/learn/fructosamine-to-a1c-conversion-calculator/
to better understand the correlation between fructosamine levels and A1c. However, I noticed that when I input the fructosamine level in your calculator (example 353), I got a different result than from your chart below (7.61 from calculator vs approx 8.1 from the chart). I tried some other numbers – and the results from the calculator never matches the chart. I have also used the calculation HbA1c = 0.017 X fructosamine level (µmol/L) + 1.61 and for the fructosamine level above I got the same result as your calculator. Which is correct? I cannot think of any reason why the calculator and the chart wouldn’t be nearly the same.
Thank you for any information you can give me to help better understand this
Leanne