Pituitary apoplexy is an uncommon endocrine emergency characterized by severe headaches (“worst headache of my life), vision changes, and vomiting. This constellation of symptoms is often referred to as the “apoplexy triad.” Although this dramatic presentation is classically observed in pituitary apoplexy, up to 25% of patients may be completely asymptomatic.
Historical Perspective
Apoplexy is a derivative of the Greek word “apoplessein,” which means “stroke.” Giovanni Morgagni made the first detailed anatomic descriptions of pituitary apoplexy in the 1760s. He classified apoplexy according to gross findings at autopsy. The presence of serous fluid in the sellar was defined as “apoplexia serosa” while gross hemorrhage into the sellar was aptly called “apoplexia sanguinea”
It has been postulated that the famous biblical story of David beheading Goliath may have occurred in the setting of an apoplectic event. Goliath, possibly suffering from a growth hormone excess state was struck in the middle of the forehead by a stone slung by David. Goliath became disoriented, fell and was subsequently decapitated by David.
Epidemiology
Pituitary apoplexy occurs in 2-12% of patients with pituitary adenomas (mostly the nonfunctioning subtype). It has a prevalence of 6.2 cases per 100,000 and an incidence of 0.17 episodes per 100,000 per year. The condition is frequent in males during the 5th to 6th decade of life.
Clinical Signs and Symptoms
Due to the intimate anatomic relations of the pituitary gland to intracranial nerves and vessels, most symptoms are neurologic.
- Headaches
- Nausea and vomiting
- Visual field defects, diplopia, and reduced visual acuity
- Meningeal irritation presents as meningismus
- Hemodynamic instability with postural hypotension
- Hemiparesis
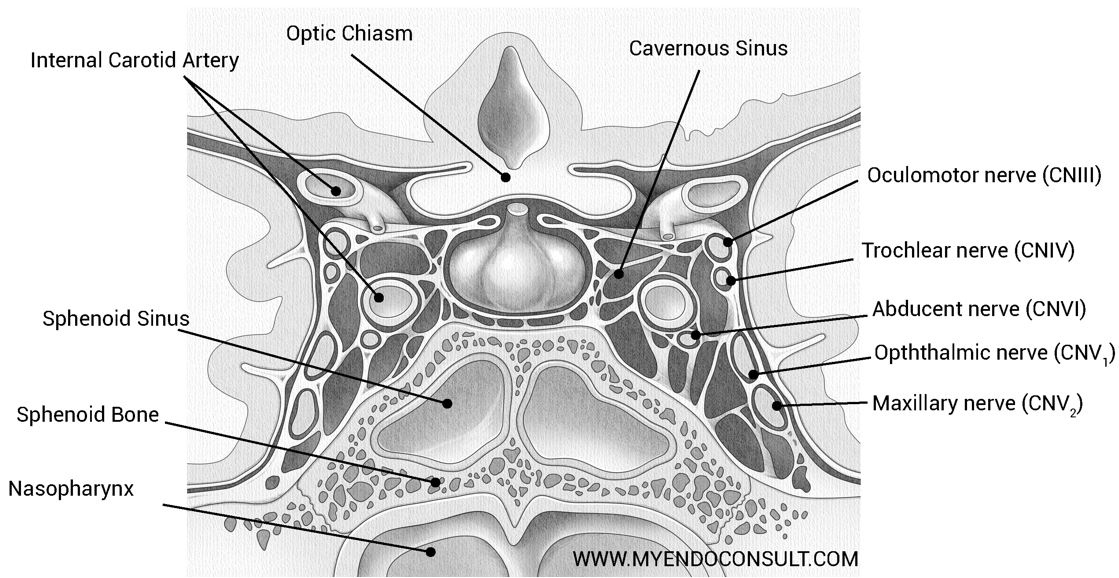
The cavernous sinus is a reticulated structure composed of interlacing filaments. The cavernous sinuses lie on either side of the sphenoid bone, adjacent to the pituitary gland. The internal carotid artery and abducens nerve lie on the medial wall of the cavernous sinus. The intracavernosal portion of cranial nerves III, IV, and ophthalmic and maxillary branches of V, lie on the lateral wall of the cavernous sinus. [Download a higher resolution image]
Etiology of Pituitary Apoplexy
| Risk factor | Mechanism |
|---|---|
| Nonfunctioning pituitary macroadenoma | Growth and outstripping its blood supply (ischemia with hemorrhagic conversion) |
| Functional tumors | Rapid growth and an ischemia-hemorrhagic conversion sequence |
| Hypertension or hypotension | vasospasm |
| Endocrine stimulation tests using thyrotropin-releasing hormone agonists | An imbalance between increased metabolic demands of pituitary tissue and pituitary perfusion. |
| Anticoagulants | Hemorrhage |
| Estrogen | - |
| Head Trauma | “David and Goliath.” Also, see the historical perspective above |
| Infections (including COVID-19 virus) | Coagulopathy |
Mechanism of Pituitary Apoplexy
The underlying pathophysiology of pituitary apoplexy is incompletely understood at this time and may vary greatly, depending on the inciting factor. What is, however, known is that a final common pathway of ischemia and hemorrhage leads to an increase in intrasellar pressure and the development of neurologic symptoms.
The normal pituitary gland is supplied by an intricate capillary network called the hypophyseal portal system. This system has its venous supply from hypothalamic portal veins (which drain into venous sinuses and subsequently into the jugular veins) and arterial supply from the superior and inferior hypophyseal arteries (originating from the internal carotid arteries).
Pituitary adenomas, however, receive a majority of their blood supply directly from arterioles and not the classic portal hypophyseal system. Rapid metabolic demands of pituitary tissue compared to the rest of the gland result in a situation where these tumors outgrowth their blood supply. This leads to ischemia, infarction, and eventually hemorrhage.
Also, tumors are supplied by thin friable vessels which have a propensity to rupture due to their incomplete maturity.
Diagnostic Tests
| Test | Reason(s) |
|---|---|
| Frank hyperintensity on T1 weighted MRI | Blood appears as a hyperintense sellar lesion |
| Hyponatremia | Adrenal insufficiency |
| Thrombocytopenia | - |
| Low TSH and free T4 | Central hypothyroidism |
| Visual field defects | Compression of cranial nerves in the cavernous sinus |
| Prolonged prothrombin time | - |
Treatment of Pituitary Apoplexy
All patients with apoplexy have a presumptive diagnosis of central adrenal insufficiency. Glucocorticoid therapy is indeed lifesaving; as such, testing for adrenal insufficiency is not required in an acute emergency. High-dose glucocorticoid therapy should be administered before pituitary imaging when there is a high index of suspicion for the condition: IV hydrocortisone 100mg stat and 100mg q8h. Adrenal insufficiency can present with hypoglycemia; as such, 5% dextrose in normal saline infusion is recommended in an acute setting.
Surgery
Transsphenoidal surgery with either an endoscope or microscope is recommended for sellar decompression. Even in expert centers, residual central pituitary hormonal insufficiencies may be persistent postoperatively. Surgery is indicated in the event of acute mental status changes or compromised vision (cranial nerve palsies)
Conservative approach
Treatment of central adrenal insufficiency with steroids is usually required. Spontaneous improvement in acute symptoms has been known to occur in patients with apoplexy. In patients with normal visual fields and no acute cranial nerve palsies, observation is a reasonable approach (expectant management)
Prognosis of Pituitary Apoplexy
Unfortunately, up to 80% of patients have persistent hypopituitarism following an apoplectic insult to the pituitary gland.
References
- Briet C, Salenave S, Bonneville JF, Laws ER, Chanson P. Pituitary Apoplexy. Endocr Rev. 2015 Dec;36(6):622-45. doi: 10.1210/er.2015-1042.
- Vanderpump M, Higgens C, Wass JA. UK guidelines for the management of pituitary apoplexy a rare but potentially fatal medical emergency. Emerg Med J. 2011 Jul;28(7):550-1. doi: 10.1136/emj.2010.106898.
Kindly Let Us Know If This Was helpful? Thank You!


