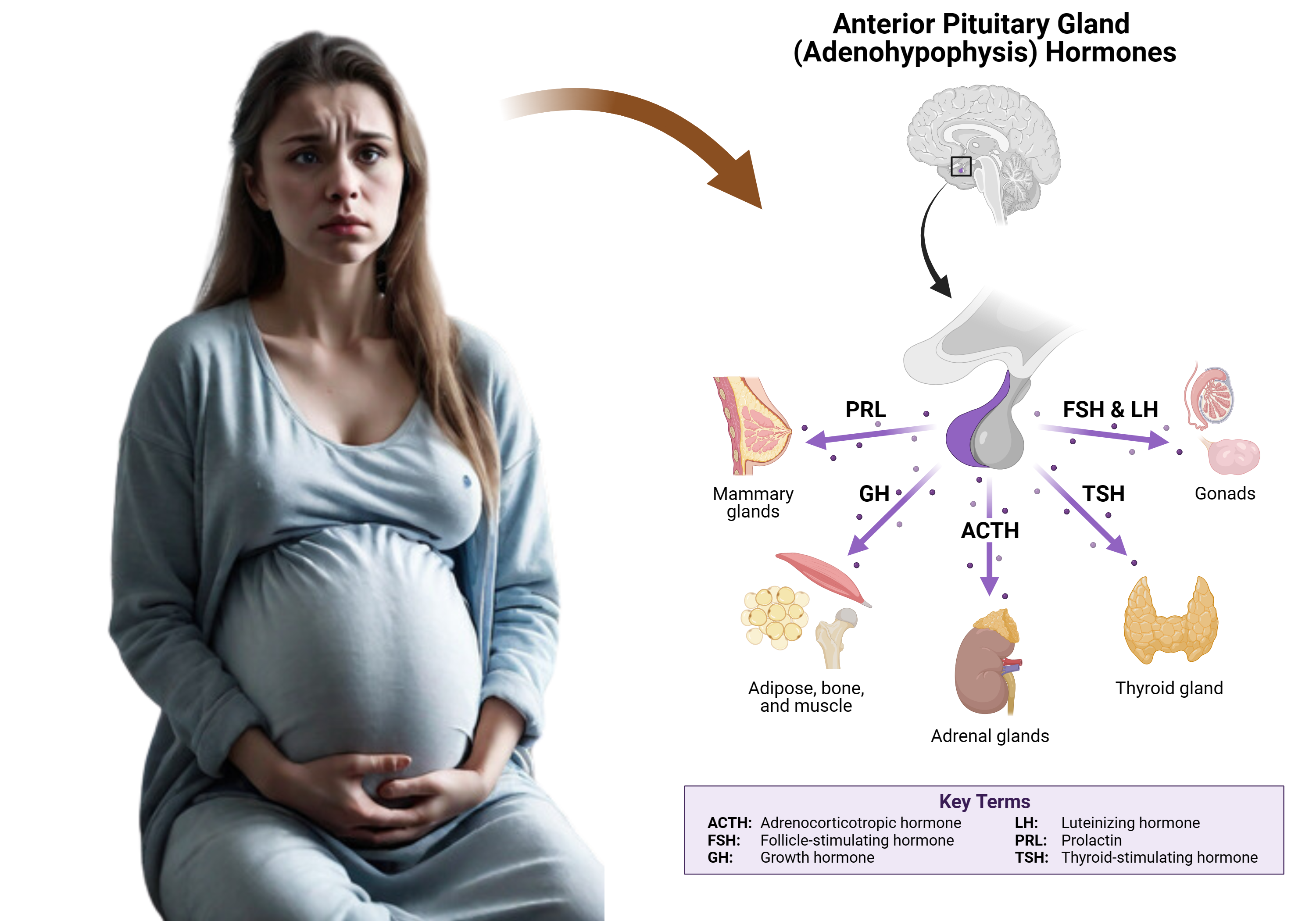
Sheehan Syndrome, first suggested by Sheehan in 1937, is a condition involving pituitary infarction following severe postpartum hemorrhage. During pregnancy, the pituitary gland enlarges, primarily due to lactotroph hyperplasia, making it vulnerable to changes in blood pressure. Sheehan hypothesized that spasm of the infundibular arteries during severe postpartum hemorrhage could lead to pituitary infarction. The condition occurs when there is prolonged lack of blood flow to the anterior pituitary, resulting in tissue necrosis, followed by stasis, thrombosis, and eventual fibrous scarring.
Clinical Presentation of Sheehan syndrome
In about half of the cases, approximately 97% of the anterior lobe is affected, but a small portion remains connected to the hypothalamus and continues receiving blood supply. Sometimes, remnants of the anterior lobe survive, either due to a small capsular blood supply or because they are located at the gland’s lateral pole, detached from vascular or neural connections.
Normal pituitary function can be maintained with about 50% of the gland intact. However, a loss of 75% and 90% of adenohypophysis cells leads to partial and complete anterior pituitary failure, respectively. If over 30% of the gland is preserved, it often suffices to prevent acute pituitary failure.
Clinically, Sheehan Syndrome can range from hypovolemic shock (related to both uterine hemorrhage and glucocorticoid deficiency) to a gradual onset of partial to complete anterior pituitary insufficiency. It may only be recognized when the patient experiences difficulties in breastfeeding, postpartum amenorrhea, or other symptoms of hypopituitarism. Acute glucocorticoid loss can be life-threatening. Lifelong pituitary target gland replacement therapy is typically required for these patients. Diabetes insipidus is rare in this context.
Sheehan syndrome should be suspected in women with a history of significant postpartum hemorrhage, especially if they required a blood transfusion and subsequently develop symptoms such as lethargy, anorexia, weight loss, inability to lactate, amenorrhea, or loss of axillary and pubic hair.
Evaluation and Imaging of Sheehan Syndrome
The diagnosis of Sheehan Syndrome involves measuring blood levels of various pituitary-dependent hormones. These include 8 am cortisol, free thyroxine, prolactin, estradiol, and insulin-like growth factor 1. A notable feature of Sheehan Syndrome is hypoprolactinemia, which is relatively uncommon in other conditions.
Magnetic Resonance Imaging (MRI) is used to detect signs of ischemic infarct in the pituitary gland. Initially, the gland may show enlargement, but this is typically followed by gradual shrinkage over several months, leading to pituitary atrophy and the development of an empty sella turcica.
Incidence and Comparison with Other Conditions
Sheehan Syndrome used to be a common cause of postpartum hypopituitarism, but its incidence has declined due to advancements in obstetric care. Nowadays, lymphocytic hypophysitis is more commonly associated with postpartum pituitary dysfunction.
In rare cases, a normal, non-pregnant pituitary gland may also undergo infarction in the context of hemorrhagic shock, although this is an uncommon occurrence.
Conclusion
In conclusion, Sheehan Syndrome is a critical postpartum condition characterized by the dysfunction or failure of the pituitary gland due to severe blood loss during childbirth. Its varied clinical presentation, ranging from mild hormonal deficiencies to severe endocrine failure, necessitates a high degree of clinical vigilance, especially in women with a history of significant postpartum hemorrhage. Advances in obstetric care have reduced its incidence, yet it remains an important differential diagnosis in postpartum women presenting with symptoms suggestive of pituitary insufficiency. Effective management relies on timely diagnosis, often through hormonal assessments and imaging techniques like MRI, followed by appropriate and often lifelong hormone replacement therapy. Awareness and understanding of Sheehan Syndrome are essential for preventing its potentially severe consequences and ensuring the well-being of affected women.
Sheehan Syndrome Quiz
Question 1:
What is the primary cause of Sheehan Syndrome?
A) Genetic mutation
B) Severe blood loss or hypovolemic shock during or after childbirth
C) Autoimmune reaction
D) Infection during pregnancy
Answer:
B) Severe blood loss or hypovolemic shock during or after childbirth
Explanation:
Sheehan Syndrome is primarily caused by severe blood loss or hypovolemic shock that occurs during or after childbirth. This significant loss of blood leads to inadequate blood flow to the pituitary gland, resulting in tissue damage or necrosis. Choices A, C, and D are not associated with the development of Sheehan Syndrome.
Question 2:
Which hormone deficiency is NOT typically associated with Sheehan Syndrome?
A) Cortisol
B) Insulin
C) Prolactin
D) Thyroxine
Answer:
B) Insulin
Explanation:
Sheehan Syndrome is characterized by deficiencies in pituitary-dependent hormones due to damage to the pituitary gland. Common hormonal deficiencies include cortisol, prolactin, and thyroxine (free thyroxine). Insulin, however, is produced by the pancreas and is not typically affected by Sheehan Syndrome.
Question 3:
Which imaging technique is most commonly used to diagnose Sheehan Syndrome?
A) X-Ray
B) Ultrasound
C) Magnetic Resonance Imaging (MRI)
D) Computed Tomography (CT) scan
Answer:
C) Magnetic Resonance Imaging (MRI)
Explanation:
Magnetic Resonance Imaging (MRI) is the preferred imaging technique for diagnosing Sheehan Syndrome. MRI can show evidence of ischemic infarct in the pituitary gland, which typically presents as enlargement followed by gradual shrinkage and eventual atrophy, leading to the development of an empty sella. X-Ray, Ultrasound, and CT scans are less commonly used for diagnosing this specific condition.
Kindly Let Us Know If This Was helpful? Thank You!


