C-peptide blood testing is an essential diagnostic tool used by endocrinologists to evaluate and manage disorders related to abnormal insulin levels. These disorders include diabetes, hypoglycemia, and insulinoma. In some cases, the test is also used to identify patients who secretly self-administer insulin. This article will explore the reference ranges, indications, clinical applications, and procedures for C-peptide blood testing.
The reference range for C-peptide in adults is as follows:
- Fasting: 0.5-2.0 ng/mL (0.17-0.66 nmol/L)
- 1 hour after glucose load: 5-12 ng/mL
Synthesis of insulin
The synthesis of insulin is a complex multistep biochemical process that takes place in the beta cells of the pancreatic islets of Langerhans. The process can be outlined in the following steps:
The process begins with the transcription of the insulin gene (INS) located on chromosome 11 in humans. The DNA sequence of the insulin gene is transcribed into a precursor messenger RNA (pre-mRNA).
Consequently, pre-mRNA undergoes splicing to remove introns, which are non-coding sequences. This process results in the formation of mature mRNA containing the coding sequence for insulin.
The mature mRNA moves from the nucleus to the cytoplasm, where it is translated by ribosomes. This translation process generates a precursor polypeptide called preproinsulin.
Next, preproinsulin contains a signal peptide that directs it to the rough endoplasmic reticulum (RER) for processing. In the RER, the signal peptide is cleaved, resulting in the formation of proinsulin. Proinsulin is a single-chain polypeptide consisting of three domains: the A chain, the B chain, and the connecting peptide, or C-peptide.
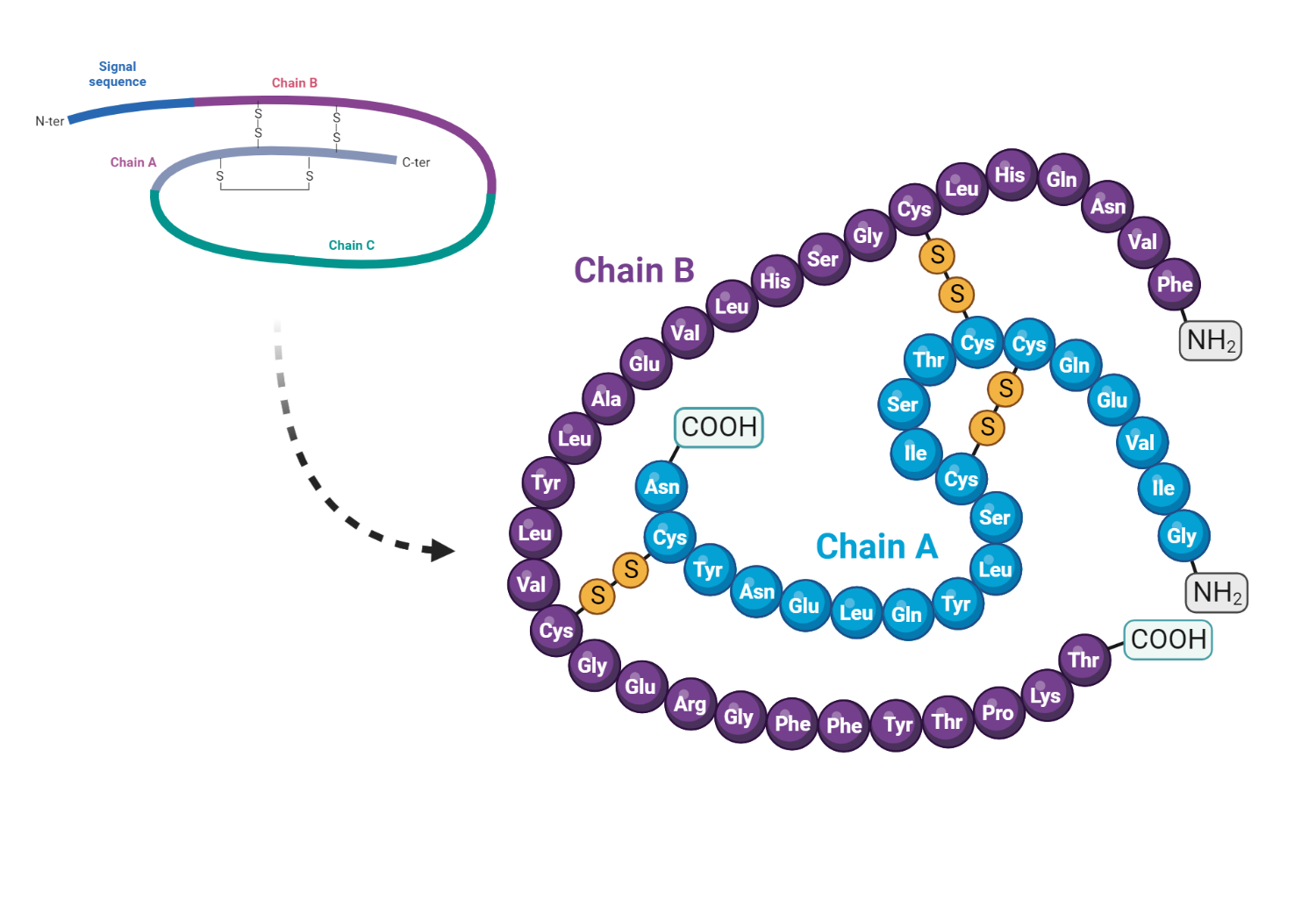
Next, proinsulin undergoes folding in the RER, where three disulfide bonds are formed between the A and B chains. These disulfide bonds are critical for insulin's correct folding and biological activity.
The correctly folded proinsulin is then transported to the Golgi apparatus, where it undergoes further processing.
In the Golgi apparatus, proinsulin is packaged into secretory granules. During this packaging process, prohormone convertase enzymes (PC1/3 and PC2) cleave the C-peptide from proinsulin, producing mature insulin and a separate C-peptide amino acid sequence.
Mature insulin is a heterodimer consisting of an A chain and a B chain, which are connected by two disulfide bonds. The C-peptide is not part of the final insulin molecule, although it is released in equimolar amounts with insulin during secretion.
Insulin-containing secretory granules are stored in the beta cells until an appropriate stimulus triggers their release, such as increased blood glucose levels. The granules fuse with the cell membrane upon stimulation, releasing insulin and C-peptide into the bloodstream.
Indications and Uses
C-peptide blood testing has several applications in medical diagnostics and management, including:
C-peptide levels can provide valuable insight into the underlying cause of hypoglycemia. Low C-peptide levels (≤2 ng/mL) with high insulin levels suggest exogenous hyperinsulinism, while decreased C-peptide, insulin, and glucose levels are associated with non-insulin-mediated hypoglycemia, such as liver disease, ethanol hypoglycemia, or adrenal insufficiency. Elevated C-peptide levels (>2 ng/mL) with increased insulin and proinsulin levels are typically seen in patients with insulinomas or hypoglycemia secondary to oral hypoglycemic agent use.
C-peptide levels can help differentiate between type 1 and type 2 diabetes. Low C-peptide and insulin levels accompanied by islet cell antibodies indicate type 1 diabetes, while elevated C-peptide and insulin levels without autoimmune markers suggest type 2 diabetes.
Elevated C-peptide, insulin, and proinsulin levels with low beta-hydroxybutyrate serum concentrations may indicate insulinoma. C-peptide levels of 2 nmol/L or higher typically point to insulinoma. The diagnosis is often made during a prolonged fast using Whipple's triad: symptomatic patients with serum glucose levels less than 45 mg/dL, hypoglycemic symptoms while fasting, and relief of symptoms after glucose administration.
Clinical Application
C-peptide is a protein that connects the beta and alpha chains of proinsulin. During the conversion of proinsulin to insulin in the beta cells of the islet of Langerhans in the pancreas, the chains of proinsulin are separated, releasing C-peptide into the portal vein in nearly equal amounts as insulin. C-peptide levels can provide an accurate assessment of islet cell function in some instances, more so than insulin levels.
Increased C-peptide levels may indicate insulinoma, pancreas transplant, renal failure, or administration of oral hypoglycemic agents. Decreased levels may indicate factitious hypoglycemia, diabetes mellitus, or total pancreatectomy.
Related Tests
- Blood glucose : venous glucose assessment
- Glucagon: An islet cell hormone that increases serum glucose levels
- Glycosylated hemoglobin: An indirect measure of chronic glucose levels
- Insulin assay: Direct measurement of insulin
Optimal Testing Conditions
Renal failure can cause increased C-peptide levels, and oral hypoglycemic agents (e.g., sulfonylureas) may also lead to elevated levels.
Kindly Let Us Know If This Was helpful? Thank You!


