The mechanism of action of cabergoline and its clinical application in the management of acromegaly will be reviewed.
Physiology
Growth hormone physiology and the role of central dopaminergic pathways : The binding of dopamine to D2 receptors in either pituitary somatotrophs or lactotrophs impairs the release of GH and prolactin, respectively(1). Additionally, dopamine impairs hypothalamic somatostatin release, which results in increased GHRH secretion(2)
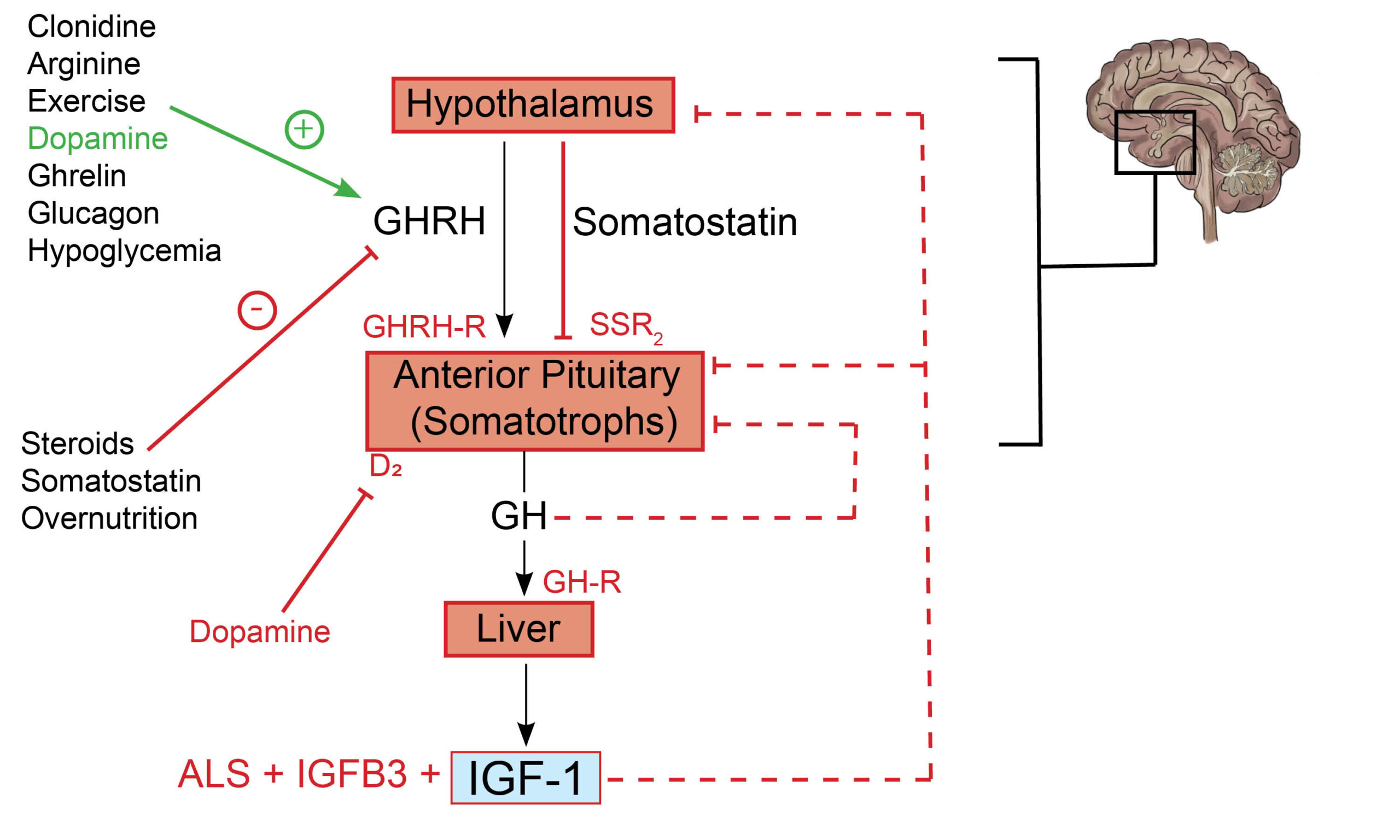
The differential effects of dopamine on GH secretion should be appreciated in normal physiology. The effects of DA at the level of the anterior pituitary gland are more profound than its effects in the hypothalamus. The net effect is a reduction in GH secretion.
Mechanism of action
Growth hormone-secreting tumors express D2R receptors to varying degrees, which determines their response to dopaminergic agonists(3). Indeed, the responsiveness of D2R’s on somatotroph tumors depends on their sensitivity and the concentration of circulating GH(4).
Practice Guide
- Cabergoline is more effective than bromocriptine and leads to a reduction in tumor size in about 30% of patients(5).
Clinical Trial Evidence
There is a paucity of randomized, placebo-controlled clinical trial evidence among patients with acromegaly treated with cabergoline(6).
Key Message
IGF-1 normalization occurs in a third of acromegalic patients treated with cabergoline monotherapy. There is limited information about the effects of cabergoline on tumor size. Shrinkage of tumors was demonstrated in patients with high baseline prolactin (PRL) and IGF-1 levels. It is a reasonable treatment option in somatomammotrophic tumors (GH-PRL co-secreting tumors).
This was a meta-analysis of prospective, non-randomized studies in patients with cabergoline-treated acromegaly. A total of 227 subjects in 15 studies with significant heterogeneity were evaluated. There was no placebo group in this study. Patients were exposed to cabergoline monotherapy in variable doses ranging from 0.3 to 7mg per week. The authors defined the primary outcome as the normalization of IGF-1. The primary outcome was achieved in 34% of patients(6).
References
- Lu M, Flanagan JU, Langley RJ, Hay MP, Perry JK. Targeting growth hormone function: strategies and therapeutic applications. Signal Transduct Target Ther. 2019 Feb 8;4(1):3.
- Vance ML, Kaiser DL, Frohman LA, Rivier J, Vale WW, Thorner MO. Role of dopamine in the regulation of growth hormone secretion: dopamine and bromocriptine augment growth hormone (GH)-releasing hormone-stimulated GH secretion in normal man. J Clin Endocrinol Metab. 1987 Jun;64(6):1136–41.
- Cooper O, Greenman Y. Dopamine Agonists for Pituitary Adenomas. Front Endocrinol. 2018;9:469.
- Lawton NF, Evans AJ, Weller RO. Dopaminergic inhibition of growth hormone and prolactin release during continuous in vitro perifusion of normal and adenomatous human pituitary. J Neurol Sci. 1981 Feb;49(2):229–39.
- Chanson P. Medical Treatment of Acromegaly with Dopamine Agonists or Somatostatin Analogs. Neuroendocrinology. 2016;103(1):50–8.
- Sandret L, Maison P, Chanson P. Place of cabergoline in acromegaly: a meta-analysis. J Clin Endocrinol Metab. 2011 May;96(5):1327–35.
Explore the pathophysiology of various endocrine diseases and the mechanism of action of medications utilized in their treatment. Click here to learn more!
Kindly Let Us Know If This Was helpful? Thank You!


