What are hormones made of? How are hormones classified, and where are they produced? This is a quick review of the endocrine system.
Introduction
Hormones are defined as chemical messengers which are dissolved in mainly extracellular fluid and carry signals between cells.
Hormones, which serve as the body's chemical messengers, can be classified into three categories based on their chemical composition: steroid, peptide, and amino acid derivative. Each type has its own unique structure and properties, leading to different mechanisms of action in the body.
Hormones are classified as peptides, steroids, and amines. We will review this classification next.
Steroid Hormones
- Derivatives of cholesterol
- They are water-insoluble (hydrophobic)
- Transported by carrier proteins
- They are typically lipid-soluble and can be administered via the oral route
- They cross the cell membrane, enter cells, and bind to intracellular receptors (cytoplasm and nucleus). This will then alter the transcription and translation of certain proteins.
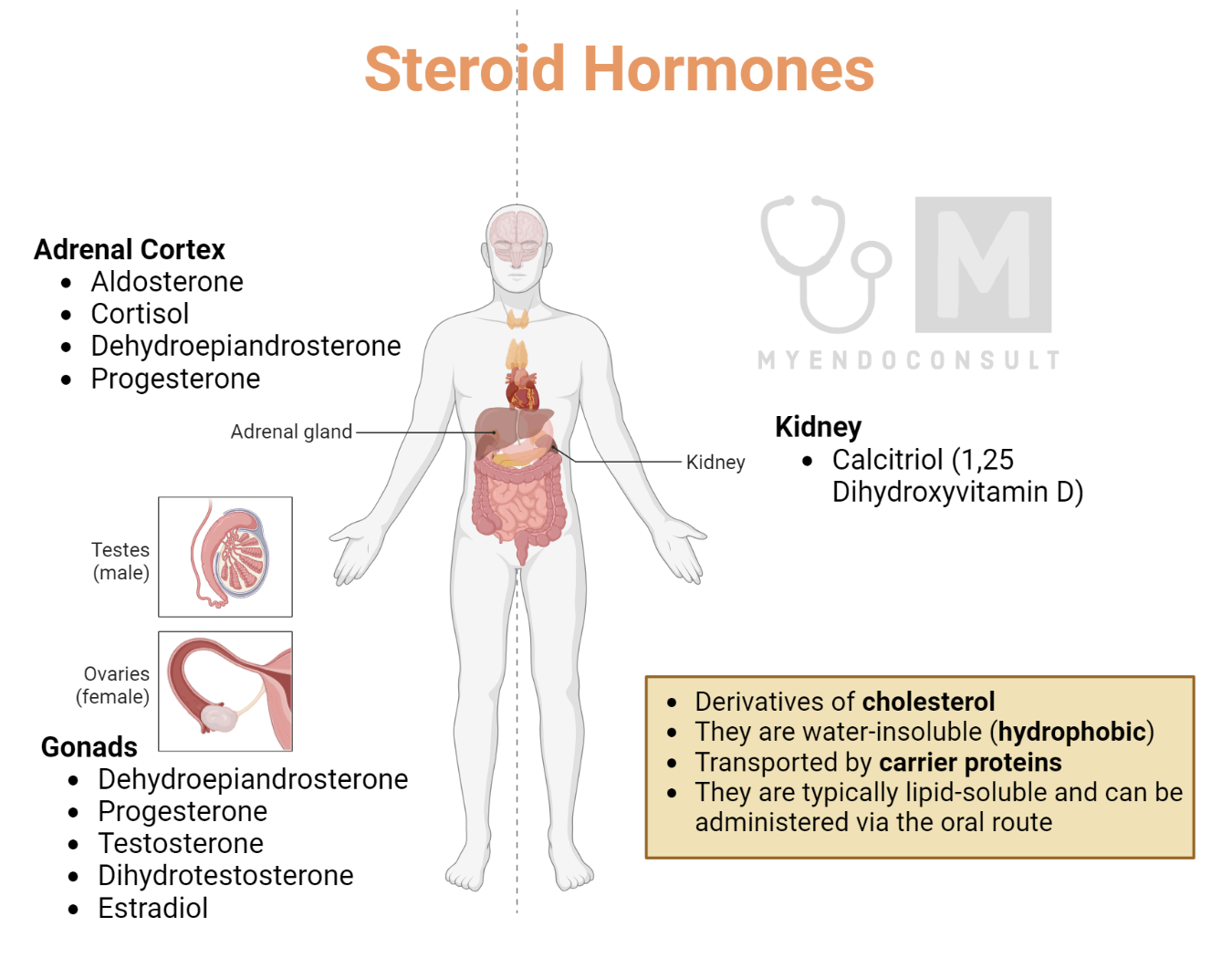
| Examples of Steroid Hormones | |
|---|---|
| Adrenal cortex | Aldosterone |
| Cortisol | |
| Dehydroepiandrosterone | |
| progesterone | |
| Gonads | Dehydroepiandrosterone |
| Progesterone | |
| Testosterone | |
| Dihydrotestosterone | |
| estradiol | |
| kidneys | Calcitriol (1,25 hydroxy vit d) |
Amine Hormones
- Derived from amino acids tyrosine and tryptophan
- Thyroid hormones behave similarly to steroid hormones (binds to intracellular receptors)
- Catecholamines behave similarly to peptide hormone
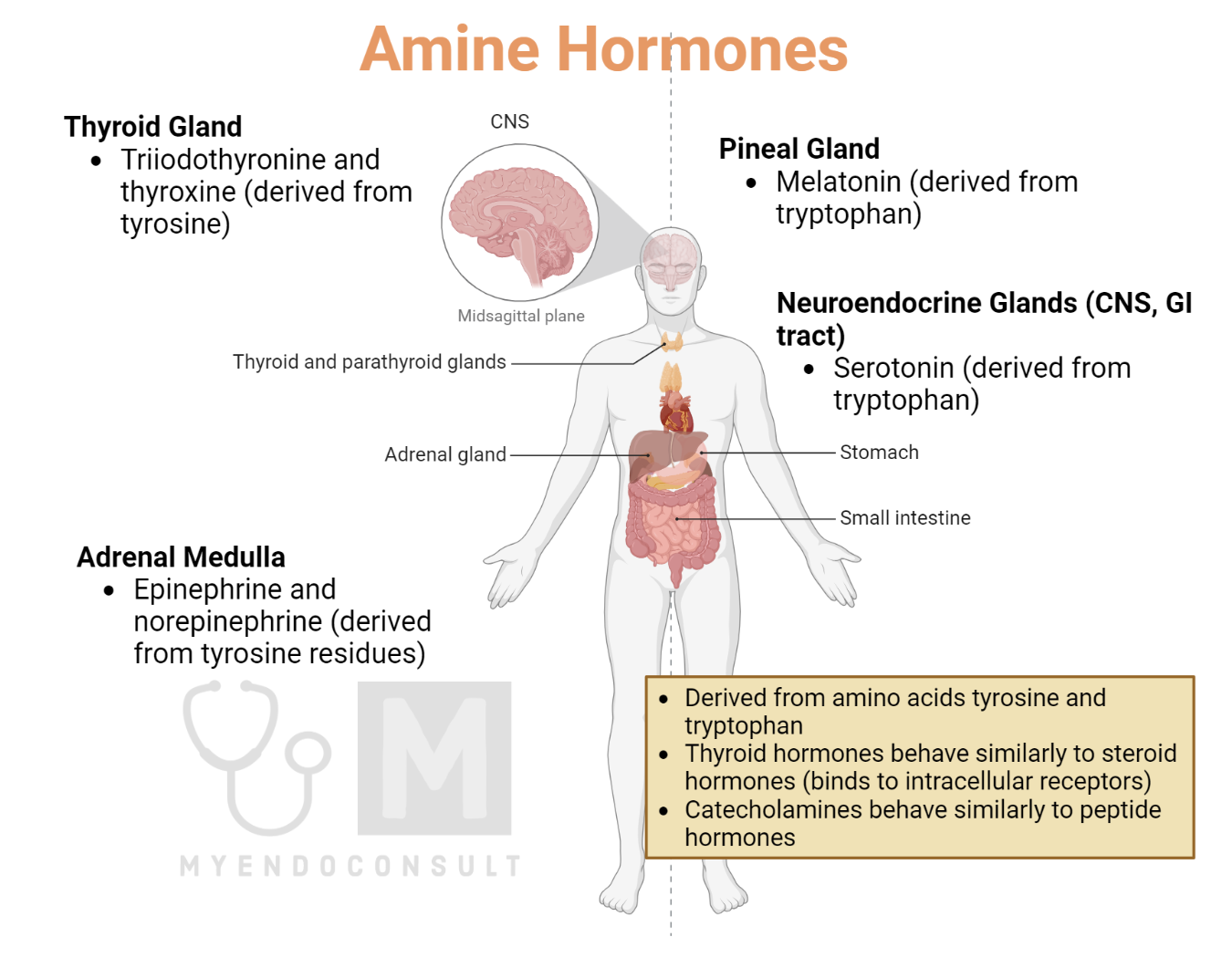
| Location | Examples of Amine Hormones |
|---|---|
| Adrenal medulla | Epinephrine and norepinephrine (derived from tyrosine residue) |
| Thyroid | triiodothyronine and thyroxine (derived from tyrosine) |
| Nonendocrine glands | Melatonin from pineal gland (tryptophan derivative) |
| Serotonin for CNS and GI tract (tryptophan derivative) |
Peptide Hormones
Peptide hormones are inactivated by gastric acid and peptidases; thus, unlike steroid hormones, they cannot be given orally. Glycoproteins (composed of peptides and carbohydrate moeities) are more stable and last longer than peptide hormones in circulation.
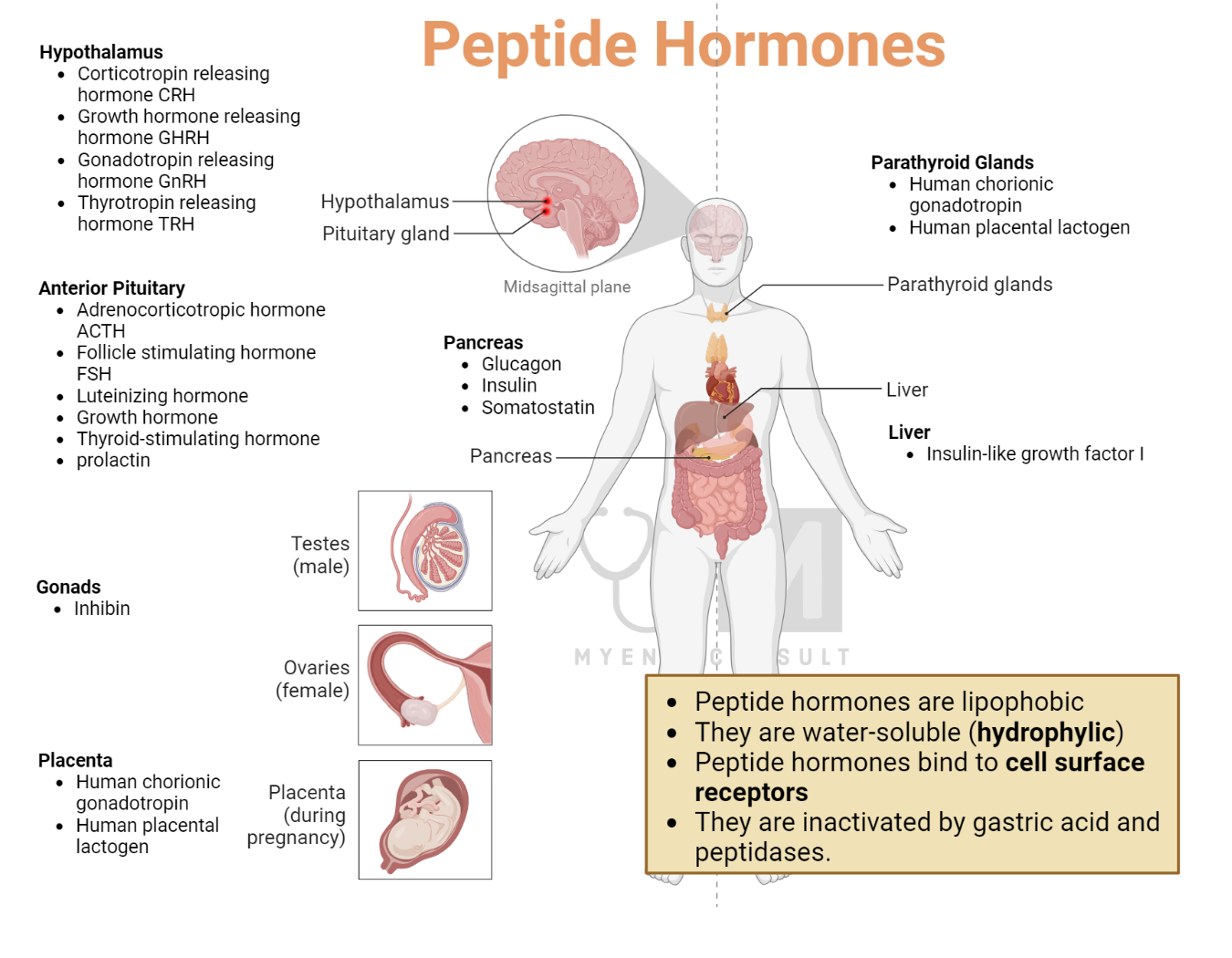
| Location | Examples of peptide hormones |
|---|---|
| Hypothalamus | Corticotropin releasing hormone CRH |
| Growth hormone releasing hormone GHRH | |
| Gonadotropin releasing hormone GnRH | |
| Thyrotropin releasing hormone TRH | |
| Anterior pituitary | Adrenocorticopric hormone ACTH |
| Follicle stimulating hormone FSH | |
| Luteinizing hormone | |
| Growth hormone | |
| Thyroid-stimulating hormone | |
| prolactin | |
| Posterior pituitary | Antidiuretic hormone |
| oxytocin | |
| Pancreatic islets | Glucagon, insulin, somatostatin |
| Calcium regulating hormone | Parathyroid hormone, calcitonin |
| Placenta | Human chorionic gonadotropin |
Hormones – Back to the basics
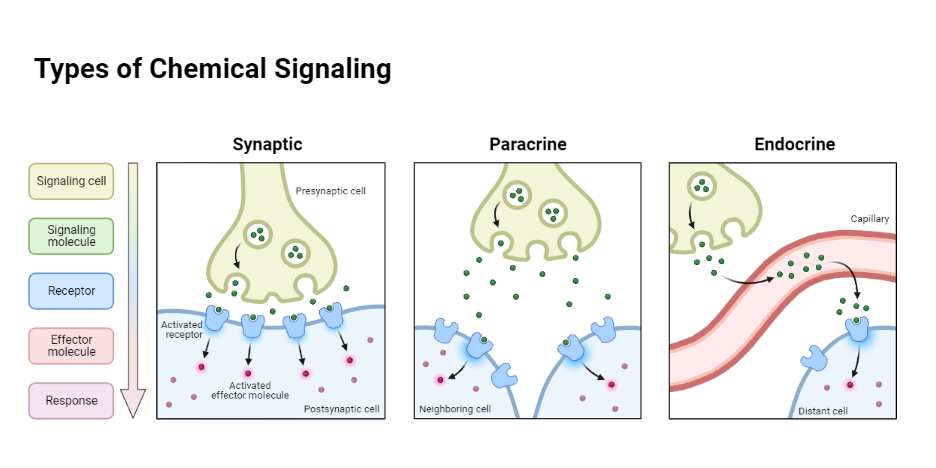
Hormones are defined as chemical messengers which are dissolved in mainly extracellular fluid and carry signals between cells. In an endocrine cell, information is transmitted via various chemical compounds known as intracellular messengers – enzymes, allosteric ligands, and proteins.
Furthermore, the function of hormones is similar to that of nerves, which also transfer signals from one cell to another.
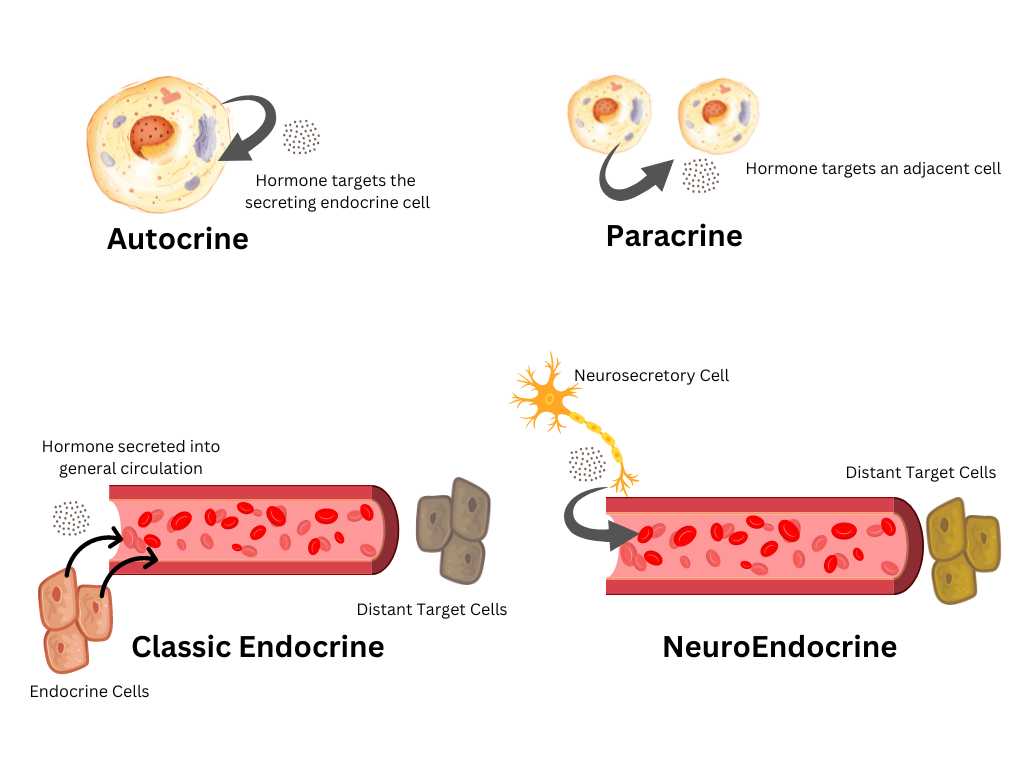
Intercellular communication cannot always be definitely assigned to either the neural or the hormonal pathway. There are certain cases where the secretion of hormones is influenced by neural stimuli, and other cases where hormones can become direct transmitters of neural information, e.g. norepinephrine, which is secreted at the nerve endings of the sympathetic nervous system.
For example, the neurosecretion of the supraoptic and paraventricular nuclei of the diencephalon is a mechanism having characteristics of both neural and hormonal communication.
In this case, information flows along the axis cylinder of a nerve cell in the form of discontinuous signals. These signals are not variations in electrical potential but rather hormone-containing particles which are converted to soluble hormones in the posterior lobe of the pituitary gland.
Hormone molecules are dissolved in the extracellular fluid and travel from their endocrine cell of origin to their appropriate receptor or target cells.
Usually, they are carried by the bloodstream and quickly reach their target cells, which may be quite distant. Hormones that diffuse only locally in the interstitial fluid surrounding an endocrine cell are called tissue hormones.
Hormone molecules transfer their information through contact with a receptor at the target cell. They thereby regulate certain chemical or physical processes within the receptor cell, which finally result in known biochemical and clinically evident hormonal actions.
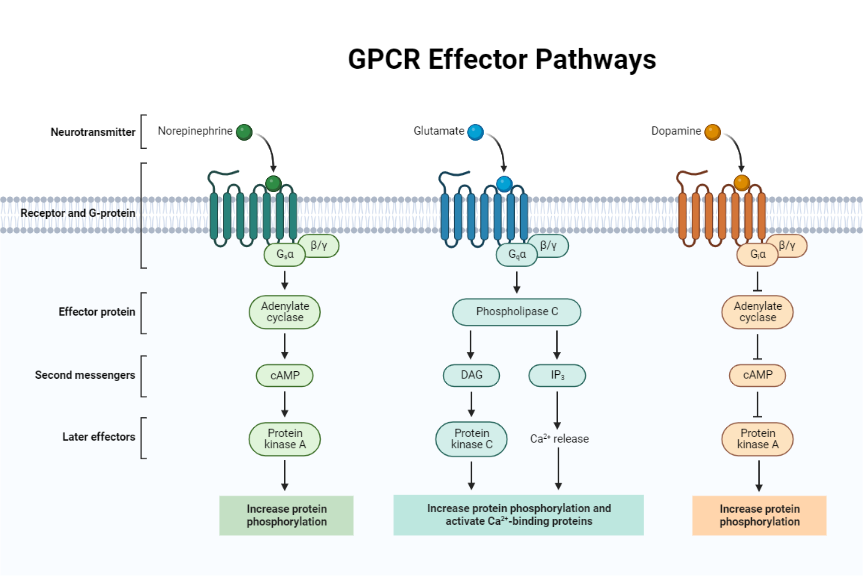
In many cases, the information contained in the hormone is reconverted at the cell membrane into an intracellular second messenger, which in tum controls a process within the cell. In this manner, information issued by the endocrine cell eventually reaches its destination.
However, the flow of information in the organism does not cease at this point. Processes may be triggered in the target cell, which leads to the formation of feedback loops.
Under the influence of a hormone, a receptor cell may release greater or smaller amounts of a chemical compound (e.g., a metabolite or another hormone) into the extracellular fluid, hereby informing the original endocrine cell that it has received and executed the instruction. Frequently, negative feedback will inhibit the endocrine cell from issuing the same information, i.e., from secreting more hormones.
Endocrine Genetics
Hormones are of great interest to the geneticist primarily because certain diseases are known to be caused by inherited deficiencies of specific hormones. Examples among the protein and peptide hormones are the inherited deficiencies of thyroid stimulating hormone and of growth hormone. In addition, several endocrine disorders are caused by an inherited deficiency of the enzymes necessary for the biosynthesis of nonprotein hormones.
Examples are the various adrenogenital syndromes and certain forms of congenital hypothyroidism. Inherited failure of the target organ to respond to its corresponding hormone is the cause of pseudohypoparathyroidism and renal diabetes insipidus.
Patients with the syndrome of multiple endocrine neoplasia suffer from an inherited tendency to develop tumors in various endocrine glands. Certain disorders of the thyroid gland, such as thyrotoxicosis, Hashimoto’s thyroiditis, and primary myxedema, all of which appear to be associated with autoimmune processes, show a familial incidence without clear-cut genetic transmission.
Other endocrine diseases, for example, Turner’s syndrome and Klinefelter’s syndrome, are due to chromosomal disorders. These syndromes have provided important information regarding the function of sex chromosomes.
It may be of interest to the biochemically oriented geneticist to know that hormones were among the first proteins to have their amino acid sequences fully elucidated. Surprisingly, certain hormones with very different actions were found to be chemically closely related. Thus, large parts of the ACTH molecule are identical to the alpha-MSH molecule. Furthermore, the whole subunit of the TSH molecule is identical to the alpha subunit of the LH molecule.
Such close similarity between two proteins is probably the end result of gene duplication, an important mechanism by which new proteins are acquired in the course of evolution.
Biosynthesis of Hormones
Protein hormones are synthesized at the ribosomes according to the “classic” concepts of molecular biochemistry.
Storage and Release of Hormones
Hormones of the pancreatic islets, anterior and posterior pituitary gland, adrenal medulla, and thyroid gland are not only synthesized but may also be stored in considerable amounts within the endocrine organ. In contrast, steroid hormones of the adrenal cortex and gonads are not stored in any significant amount. Granules surrounded by membranes can be detected in most of the endocrine cells which do store hormones by light and electron microscopy.
Thyroid hormones are stored in an unusual manner, namely extracellularly in the colloid as components of thyroglobulin. Thyroxine and triiodothyronine are probably bound by peptide bonds to this large glycoprotein molecule. Release implies the expulsion of the hormone from its endocrine cell into the extracellular fluid. The granular membrane fuses with the cell membrane and the granular content is ejected into the extracellular fluid by a process termed exocytosis.
The process of hormone release must occupy a central position in the transfer of information by hormones, as underscored by the following reasoning: Most hormones have a fixed peripheral disposal rate, or half-life, once they have left the endocrine cell. Therefore, a given hormone concentration in the extracellular fluid which is crucial for the information to be conveyed can only be achieved and maintained by adjusting the rate of hormone release. Consequently, hormone release must be a delicately controlled process.
Hormone Transport
Hormone molecules travel in the extracellular fluid from their endocrine cell of origin to their receptor cell. In most cases, hormones diffuse from the interstitial fluid surrounding the endocrine cell into the blood, which assures rapid transport to the receptor cell.
Tissue hormones are an exception. They diffuse only locally in the interstitial fluid and thus reach only neighboring cells. Often the concentration of a hormone is not uniform in all parts of the circulation, i.e., the circulating blood is subdivided into hormonal compartments. Such a process is probably of great importance for hypothalamic-releasing factors. These factors attain an effective concentration only in the very small pituitary portal veinous system. The effects of glucagon and insulin on the liver are influenced by the fact that their concentration is significantly higher in the portal system than in the arterial blood.
Certain hormones are bound to specific proteins in the blood. Assuming that only one single protein with only one binding site per molecule combines with the hormone, the reaction occurs according to the general formula:
h + p = hp
h = free hormone, p = carrier protein, hp hormone-carrier protein complex.
Experiments with isotopically labeled hormones have shown that the free hormone is in general, fully exchangeable with the protein-bound hormone. This suggests that the hormone binds to the protein by noncovalent bonds and that the free and the bound hormone are in an equilibrium governed by the law of mass action.
Receptors
For a hormone molecule to produce an effect it must come into direct physical contact with the target cell. The target cell possesses certain structures termed receptors which “recognize” a hormone and convert the information contained in the dissolved hormone into various biochemical processes within the cell. During this process of recognition, a physical or chemical reaction must take place between the hormone molecule and its receptor.
The three-dimensional shape of the receptor molecule is complementary to the shape of the hormone molecule or of parts of it, in which case the hormone and the receptor would fit together like pieces of a jigsaw puzzle.
References
- Hiller-Sturmhöfel S, Bartke A. The endocrine system: an overview. Alcohol Health Res World. 1998;22(3):153-64.
- Beato M, Klug J. Steroid hormone receptors: an update. Hum Reprod Update. 2000 May-Jun;6(3):225-36.
- Tager HS, Steiner DF. Peptide hormones. Annu Rev Biochem. 1974;43(0):509-38.
- Murrey SJ, Brecher AS. Interaction of biogenic amine hormones with acetaldehyde. Dig Dis Sci. 2010 Jan;55(1):21-7.
Kindly Let Us Know If This Was helpful? Thank You!


