Ezetimibe represents a unique therapeutic intervention in lipid management as it stands as the inaugural compound approved for reducing total and LDL cholesterol (LDL-C) levels through the inhibition of cholesterol absorption in small intestinal enterocytes.
In human subjects, Ezetimibe has demonstrated an ability to reduce cholesterol absorption by 54%, which results in a compensatory upregulation of cholesterol synthesis. This compensatory effect can be mitigated by employing a cholesterol synthesis inhibitor such as a statin.
The outcome of the intestinal cholesterol absorption blockade is a decrease in the integration of cholesterol into chylomicrons, which subsequently reduces the delivery of cholesterol to the liver via chylomicron remnants. Given that chylomicron remnants are notably atherogenic lipoproteins, a reduction in their cholesterol content could directly inhibit atherogenesis. The diminished delivery of intestinal cholesterol to the liver stimulates the expression of hepatic genes involved in LDL receptor expression and cholesterol biosynthesis, which in turn promotes hepatic LDL receptor expression and facilitates LDL-C clearance from plasma. Ezetimibe, therefore, reduces LDL-C levels by 15%-20%.
Physiology of cholesterol absorption in the intestines
For a comprehensive grasp of cholesterol absorption within the small intestine, it’s essential to elucidate the fundamental processes associated with both dietary and biliary cholesterol. Cholesterol absorption in the small intestine comprises multiple procedures, irrespective of its source.
Firstly, free cholesterol binds to the Niemann-Pick C1-like 1 (NPC1L1) protein, which is situated on the luminal aspect of the enterocyte plasma membrane. Following this, the complex associates with clathrin/AP2, a crucial facilitator for the vesicular endocytosis of the NPC1L1-cholesterol complex into the enterocyte. Additionally, clathrin and AP2 play indispensable roles in forming the small vesicles undergoing endocytosis and in the intracellular pathways interacting with the plasma membrane. In the absence of clathrin/AP2 activity, the endocytosis or delivery of NPC1L1 and cholesterol would not take place.
Once the NPC1L1-cholesterol complex is endocytosed, cholesterol is released, and NPC1L1 is recycled to the plasma membrane for further cholesterol binding and absorption. The liberated cholesterol within the cytosol undergoes esterification by acyl-coenzyme A: cholesterol acyltransferase (ACAT), resulting in the formation of cholesterol esters. These newly generated cholesterol esters amalgamate with triacylglycerol particles (derived from absorbed free fatty acids) and ApoB-48 to construct chylomicrons. Finally, the newly formed ApoB-48-containing chylomicrons are taken up into the portal or lymphatic circulation, making them available for utilization throughout the body.
Mechanism of action of Ezetimibe
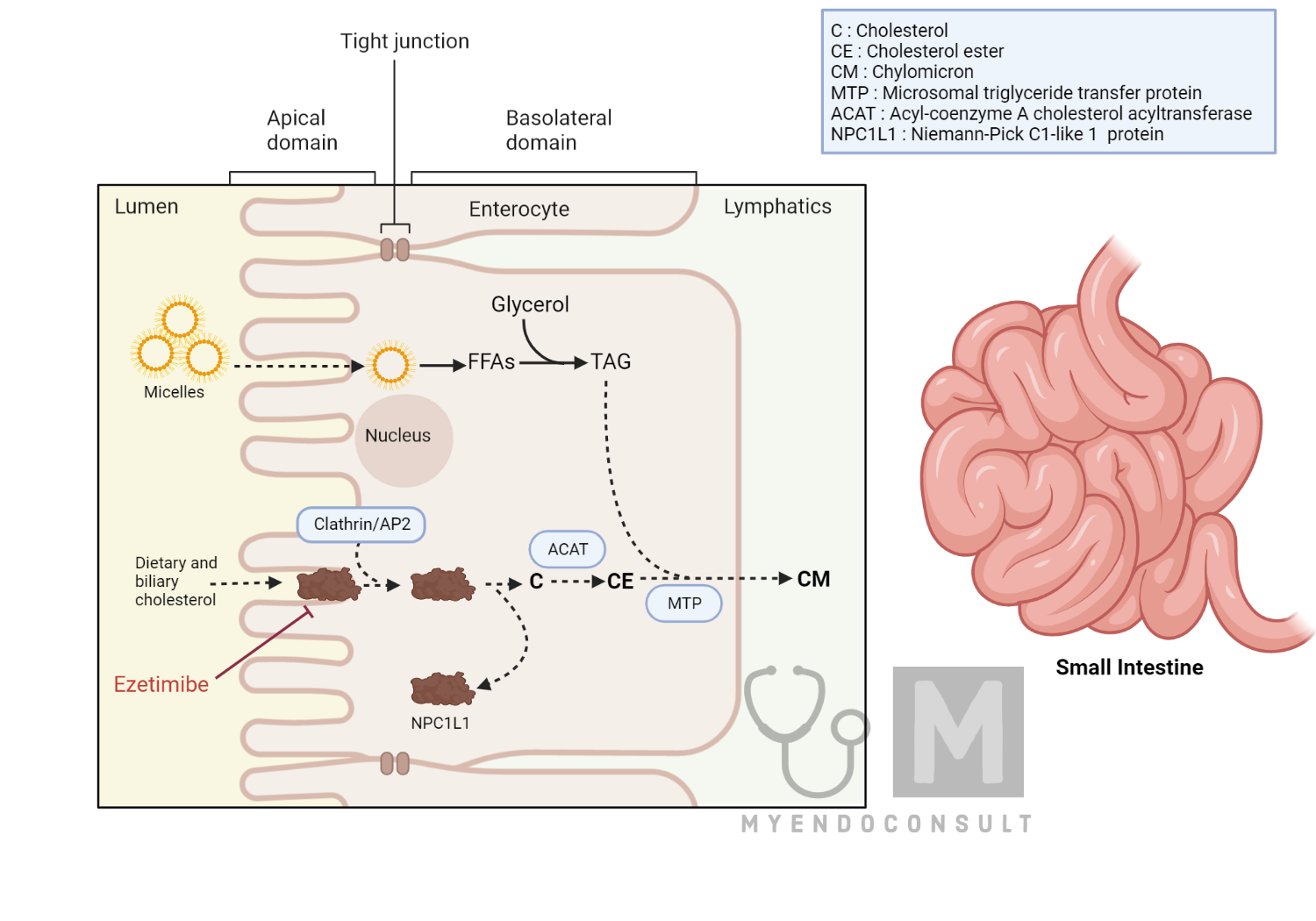
Ezetimibe and its primary metabolite, ezetimibe glucuronide, play a crucial role in limiting cholesterol absorption within the small intestine. They achieve this through direct binding to a transmembrane loop of the NPC1L1 protein, a key transporter facilitating cholesterol ingress into enterocytes, the cells lining the small intestine.
By attaching to NPC1L1, both Ezetimibe and Ezetimibe glucuronide obstruct the protein’s interaction with clathrin and AP2, essential elements for its internalization into the enterocyte. This interaction impedes the enterocyte’s capacity to uptake the cholesterol/NPC1L1 complex, resulting in a consequent reduction of dietary cholesterol absorption.
Pharmacotherapeutic properties of Ezetimibe
In terms of absorption, distribution, metabolism, and excretion (ADME), Ezetimibe is highly water-insoluble, making bioavailability studies infeasible. Upon ingestion, it undergoes glucuronidation in the intestinal epithelium before absorption and subsequently enters an enterohepatic recirculation. Pharmacokinetic analyses suggest that approximately 70% of the compound is excreted in feces and 10% in urine, predominantly as a glucuronide conjugate. Bile acid sequestrants can impair the absorption of Ezetimibe. Hence their co-administration is not recommended.
Practice Guide
Therapeutically, Ezetimibe is offered as a 10-mg tablet that can be ingested at any time and with or without food. While Ezetimibe can be used in combination with other dyslipidemia medications, it should not be co-administered with bile acid sequestrants. The utilization of Ezetimibe as a monotherapeutic strategy for patients with elevated LDL-C is generally reserved for a subset of patients who cannot tolerate statins. However, Ezetimibe’s actions are complementary to those of statins, with combination therapy leading to a synergistic reduction in LDL-C levels.
Precautions
Aside from infrequent instances of allergic reactions, there have been no documented specific adverse effects associated with ezetimibe use in patients. However, due to the known contraindications of all statins in pregnant and lactating women, combination therapies that encompass both Ezetimibe and a statin should be cautiously prescribed to women of reproductive age and only when adequate contraception measures are implemented.
References
Phan BA, Dayspring TD, Toth PP. Ezetimibe therapy: mechanism of action and clinical update. Vasc Health Risk Manag. 2012;8:415-27.
Kosoglou T, Statkevich P, Johnson-Levonas AO, Paolini JF, Bergman AJ, Alton KB. Ezetimibe: a review of its metabolism, pharmacokinetics and drug interactions. Clin Pharmacokinet. 2005;44(5):467-94.
Hammersley D, Signy M. Ezetimibe: an update on its clinical usefulness in specific patient groups. Ther Adv Chronic Dis. 2017 Jan;8(1):4-11.
Kindly Let Us Know If This Was helpful? Thank You!


