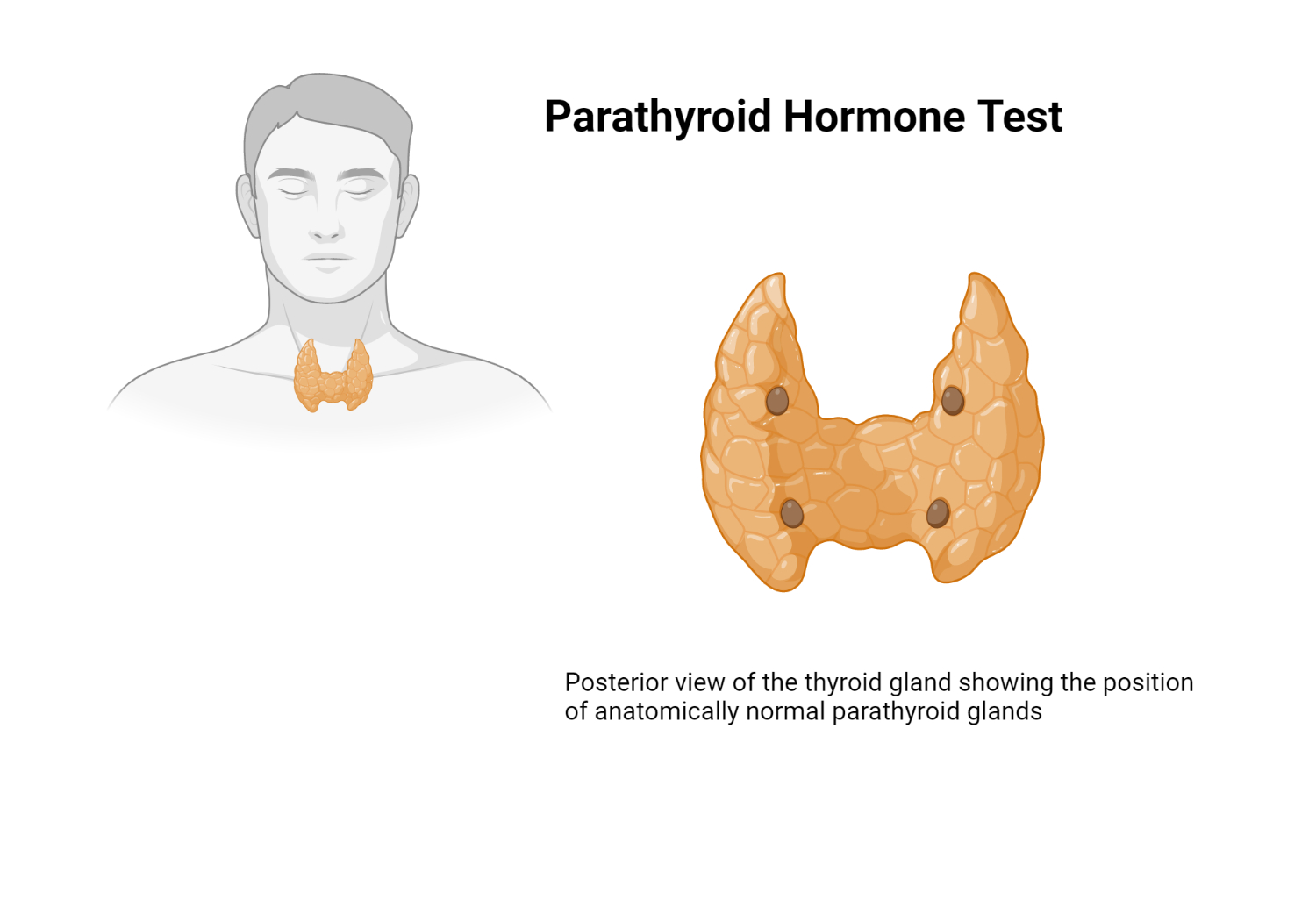
Parathyroid hormone (PTH) is a peptide hormone secreted by the parathyroid glands, which plays a pivotal role in maintaining calcium and phosphate homeostasis in the body. Consequently, PTH regulation is crucial for bone health and overall metabolic processes. This article aims to provide an in-depth understanding of PTH lab tests, their indications, and their clinical applications.
PTH Lab Test: Description and Reference Range
The PTH lab test quantifies PTH levels in serum or plasma samples. This assessment is instrumental in the evaluation and management of thyroid and kidney disorders, especially in patients with chronic renal failure (CRF). The reference range for PTH levels is dependent on the patient's age and the sample type (serum or plasma).
- Adults (serum):
- C-terminal : 50-330 pg/mL (50-330 ng/L)
- N-terminal: 8-24 pg/mL (8-24 ng/L)
- Intact molecule: 10-65 pg/mL (10-65 ng/L)
- Pediatrics:
- C-terminal (ages 1-16): 51-217 pg/mL (51-217 ng/L)
- N-terminal (ages 2-13): 14-21 pg/mL (14-21 ng/L)
- Intact molecule (ages 2-20): 9-52 pg/mL (9-52 ng/L)
Structure of the PTH molecule
Parathyroid hormone (PTH) is a peptide hormone comprising 84 amino acids, and it plays a significant role in regulating calcium and phosphate levels in the body. The PTH molecule can be divided into three main regions: the N-terminal, C-terminal, and the intact molecule.
The N-terminal region consists of the first 34 amino acids at the PTH molecule's amino (NH2) end. This portion is biologically active and responsible for the majority of PTH's physiological effects, such as stimulating bone resorption, increasing renal calcium reabsorption, and promoting renal phosphate excretion. Furthermore, the N-terminal fragment can be measured using specific immunoassays, helping assess PTH's functionality in various clinical settings.
The C-terminal region refers to the remaining 50 amino acids at the carboxyl (COOH) end of the PTH molecule. This portion is considered biologically inactive, meaning it does not contribute to PTH's physiological actions. However, the C-terminal fragment circulates in the bloodstream and can be measured using immunoassays. Elevated levels of the C-terminal fragment may indicate increased PTH secretion or impaired PTH metabolism.
The intact PTH molecule consists of the entire 84-amino acid peptide hormone, including both the N-terminal and C-terminal regions. Intact PTH is biologically active and can be measured using specific immunoassays that recognize the whole molecule. Intact PTH measurements are often preferred in clinical practice because they provide a more accurate representation of the hormone's activity in the body.
Methods of Assessing PTH levels
Current technologies for assessing parathyroid hormone (PTH) levels predominantly involve immunoassay techniques. Immunoassays are biochemical tests that leverage the specific binding properties of antibodies to target molecules, in this case, PTH. These tests offer high sensitivity and specificity for detecting and quantifying PTH levels in blood samples. The following are the most common immunoassay techniques employed for PTH assessment:
Radioimmunoassay (RIA): RIA is a classic immunoassay technique that uses radioactively labeled PTH molecules as tracers. The assay measures the amount of radioactive PTH bound to its specific antibody. By comparing the binding to a standard curve, the concentration of PTH in the sample can be determined. Although sensitive and specific, RIA has declined in popularity due to concerns over radioactive waste and the availability of alternative techniques.
Enzyme-Linked Immunosorbent Assay (ELISA): ELISA is a widely used immunoassay technique that employs enzyme-linked antibodies to detect PTH. In this assay, a color change occurs when an enzyme substrate is added, and the intensity of this color change is directly proportional to the amount of PTH present in the sample. ELISAs are relatively quick, sensitive, and easy to perform, making them a popular choice for PTH assessment.
Electrochemiluminescence Immunoassay (ECLIA): ECLIA is an advanced immunoassay technique that uses electrochemiluminescence, the production of light resulting from an electrochemical reaction, as a detection method. In ECLIA, the PTH molecules are labeled with a chemiluminescent compound, which emits light upon encountering an electrical current. The intensity of the emitted light is proportional to the amount of PTH present in the sample. ECLIA offers high sensitivity, specificity, and a broad dynamic range.
Chemiluminescent Immunoassay (CLIA): CLIA is another advanced immunoassay technique that utilizes chemiluminescence for detection. In CLIA, the PTH molecules are tagged with a chemiluminescent compound that emits light upon reaction with a specific substrate. The emitted light intensity is measured and is proportional to the PTH concentration in the sample. CLIAs are highly sensitive, specific, and rapid, making them a popular choice in many clinical laboratories.
These immunoassay techniques have revolutionized PTH assessment and contributed to improved diagnosis and management of various endocrine and metabolic disorders. Continuous advancements in assay technology promise further enhancements in PTH detection sensitivity, specificity, and overall efficiency.
Indications and Clinical Applications
Several clinical situations warrant PTH lab test utilization:
- Parathyroidectomy in patients presenting primary hyperparathyroidism.
- Hypocalcemia as a secondary outcome of thyroidectomy.
- Suspected hypercalcemia attributable to hyperparathyroidism.
- Chronic kidney disease.
- Hypocalcemia.
- Suspected or confirmed bone disease.
Related Tests
Additional tests which may be ordered alongside the PTH lab test:
- Parathyroid panel.
- Direct measurement of serum calcium levels.
- Direct measurement of serum inorganic phosphate levels.
- Test Procedure and Patient Preparation
The PTH lab test generally necessitates a fasting blood sample procured in the morning (8 AM). The patient should abstain from food overnight, consuming only water. It is essential for healthcare practitioners to be apprised of any medications the patient is currently taking, as particular drugs can influence PTH levels.
Sample Storage and Handling
PTH samples must adhere to laboratory guidelines regarding storage and handling, which typically involve immediate freezing and storage at designated temperatures. The sample may require transfer on dry ice to a central laboratory for analysis.
What To Tell the Patient Before and After the Test
Prior to the test, healthcare practitioners should discuss the reason for the PTH test and also inform the patient about fasting requirements. This is important since meal intake can cause spurious elevations in serum PTH.
Conclusion
The PTH lab test is critical in the evaluation and management of various thyroid and kidney disorders. A comprehensive understanding of this test's indications, procedures, and clinical applications allows healthcare providers to ensure accurate diagnosis and optimal patient care.
References
LaGow B et al., eds. PDR Lab Advisor. A Comprehensive Point-of-Care Guide for Over 600 Lab Tests. First ed. Montvale, NJ: Thomson PDR; 2007.
Kindly Let Us Know If This Was helpful? Thank You!


