Primary hyperparathyroidism is a condition in which one or more of the parathyroid glands become overactive and produce too much of the hormone parathormone.
This can lead to many unpleasant symptoms and complications if left untreated. It’s important for patients to be aware of this condition and its potential effects on their health. So let’s explore together what primary hyperparathyroidism is.
Symptoms of Primary Hyperparathyroidism
Common symptoms associated with this disorder include fatigue, bone pain, kidney stones, and increased thirst.
Fatigue: Fatigue is one of the most common symptoms of primary hyperparathyroidism. It can be caused by an increase in calcium levels that leads to muscle weakness and exhaustion. Patients may also experience difficulty sleeping due to frequent urination at night as well as feelings of restlessness during the day.
Bone Pain: Primary hyperparathyroidism can cause bone pain due to an imbalance between calcium and phosphorus levels in the body. This imbalance causes bones to become brittle and weak leading to fractures or joint pain. In addition, patients may experience tenderness around their joints or a feeling of heaviness in their limbs due to weakened muscles from high calcium levels.
Kidney Stones: Renal colic (pain due to kidney stones) is another symptom associated with primary hyperparathyroidism. This occurs because high PTH levels lead to increased amounts of calcium being excreted through urine resulting in crystal formation within the kidneys which can form into stones over time if not treated properly.
Increased thirst is another symptom related to primary hyperparathyroidism since higher blood calcium levels result in dehydration from excessive urination.
Primary Hyperparathyroidism can present with a wide range of symptoms, ranging from mild to severe. Diagnosis is the next step in understanding and managing this condition.
Diagnosis of Primary Hyperparathyroidism
Primary hyperparathyroidism (PHPT) is a condition in which one or more of the parathyroid glands produce too much parathyroid hormone (PTH). This can lead to an elevated level of calcium in the blood, known as hypercalcemia.
Parathyroid hormone levels may either be normal or high in the presence of high blood calcium levels. It is worth knowing that PTH can indeed be normal in people with primary hyperparathyroidism. This is because, under normal circumstances, the parathyroid glands reduce the production of PTH when calcium levels are high. Thus if parathyroid hormone levels continue to remain normal even in the presence of high blood calcium levels, this suggests an abnormality of the parathyroid glands. Endocrinologists refer to this state as “an inappropriately normal PTH in the presence of high blood calcium levels.” Diagnosing PHPT requires laboratory tests that measure levels of calcium and PTH in the blood.
Laboratory Tests: The most common test used to diagnose PHPT is a serum calcium test, which measures the amount of calcium circulating in your bloodstream. If this value is higher than normal, it could indicate PHPT. Other tests such as ionized calcium and phosphate are also used to confirm diagnosis. In addition, a serum PTH test may be ordered to measure levels of PTH in your body; if these values are higher than normal, it could indicate primary hyperparathyroidism.
Your physician will order a 24 hour urine calcium collection for evaluation of urine calcium. Do not skip this test, since on rare occasions some patients with a genetic condition known as Familial Hypocalciuric Hypercalcemia (FHH) can also have both high blood calcium and parathyroid hormone levels.
Imaging Studies: Imaging studies such as ultrasound, parathyroid sestamibi scan or CT scan may be performed if underlying causes for PHPT as part of testing before surgery. These imaging studies help doctors locate any abnormal growths of not only the parathyroid glands but also the thyroid gland that might affect the nature of your surgery.
The parathyroid glands have been called the last anatomic discovery for good reason. This is because the parathyroids are very small and were only discovered in humans in 1880. For this reason, slight enlargement of the parathyroids can be missed on imaging even when there is clinically significant disease.
As such, the absence of a clearly discernible parathyroid tumor on imaging does not preclude the need for surgery. Primary hyperparathyroidism is biochemical diagnosis (requires blood and urine testing) and not a radiologic (ultrasound or CT scanning) one.
Bone Density Test: A bone density test may also be done if there is concern about osteoporosis due to prolonged exposure to high levels of parathormone caused by PHPT. This test measures how strong your bones are and helps determine whether you have developed osteoporosis from long-term effects associated with primary hyperparathyroidism. Your endocrinologist will likely order a special 3 site DEXA scan. This will evaluate bone density in your non-dominant forearm, lumbar spine and hips.
Other Tests: Additional tests such as urine analysis and 24-hour urine collection may also be ordered depending on individual circumstances related to symptoms experienced by patients with primary hyperparathyroidism . These tests help identify any other medical conditions that might contribute or cause secondary forms of hyperparathyoidism such as exposure to thiazide diuretics, kidney disease or vitamin D deficiency .
Overall, diagnosing primary hyperparathyroidism requires careful evaluation through laboratory testing and imaging studies combined with relevant patient history information regarding signs and symptoms.
Early diagnosis of primary hyperparathyroidism is important in order to ensure timely treatment and improve outcomes. In the next section, we will discuss the various treatment options available for this condition.

Key Message
Diagnosing primary hyperparathyroidism requires laboratory tests (serum calcium, ionized calcium and phosphate, PTH), imaging studies (parathyroid ultrasound, sestamibi scan or CT scan) and other tests such as urine analysis or 24-hour urine collection. Bone density test may also be done to check for osteoporosis.
Treatment Options for Primary Hyperparathyroidism
Treatment options for PHPT are designed to reduce PTH levels and restore normal calcium balance.
Surgery: The most common treatment option for PHPT is surgery to remove the affected gland(s). This procedure, known as a parathyroidectomy, is usually performed on an outpatient basis. During the procedure, the surgeon will make a small incision in the neck and locate the enlarged glands. Once located, they can be removed with minimal risk of complications. After surgery, patients typically experience relief from symptoms within days or a few weeks.
In some cases where surgery is not possible or desirable, medications may be used to reduce PTH levels and help restore calcium balance. These medications include calcimimetics such as cinacalcet which work by blocking certain receptors that stimulate PTH production or bisphosphonates which inhibit bone resorption.
The treatment options for primary hyperparathyroidism range from watchful waiting to surgery, and it is important to understand the risks and benefits of each option. Now let’s look at the complications associated with this condition.
Complications Associated with Primary Hyperparathyroidism
If left untreated, this can lead to serious complications.
Osteoporosis: One of the most common complications associated with primary hyperparathyroidism is osteoporosis. This occurs when there is too much calcium being removed from the bones and not enough being replaced, leading to weakened bones that are prone to fractures and breaks.
Kidney Stones: Excess calcium levels caused by primary hyperparathyroidism can also increase the risk for developing kidney stones. These small stones form within the kidneys and can cause severe pain as they pass through the urinary tract system on their way out of your body.
Heart Disease: Primary hyperparathyroidism has been linked to an increased risk for heart disease (mainly hypertension).
Chronic kidney failure: Progressive decline in kidney function can lead to kidney failure.
It is important for those living with primary hyperparathyroidism to make lifestyle changes that will help manage their symptoms and reduce their risk of further complications. Eating a balanced diet rich in fruits and vegetables while limiting processed foods can help keep calcium levels regulated, while regular exercise helps maintain strong bones and muscles even if osteoporosis is already present due to this condition. Additionally, it is important to get regular checkups with your doctor so any potential issues can be caught early before they become more serious health concerns down the line.
Primary Hyperparathyroidism can cause serious complications if left untreated, but with proper care and management, the risks can be minimized. Moving forward, let’s look at how to live with Primary Hyperparathyroidism.
Living with Primary Hyperparathyroidism
Living with primary hyperparathyroidism requires regular monitoring by your doctor and adherence to a healthy lifestyle. Eating a balanced diet rich in calcium and vitamin D is important for those living with this condition. Calcium helps keep bones strong, while vitamin D aids in the absorption of calcium from food sources.
Calcium is typically restricted to less than 800mg/day in those with untreated disease. Vitamin D levels should be normal, in order to prevent further increases in the levels of PTH.
Foods such as dairy products, leafy greens, salmon, sardines, fortified cereals and juices are all good sources of both calcium and vitamin D. Exercise can also help maintain bone health by increasing muscle strength and balance. Regular physical activity has been shown to reduce pain associated with primary hyperparathyroidism as well as improve overall quality of life.
Smoking should be avoided due to its negative effects on bone health; smoking increases the risk of developing osteoporosis which can lead to fractures or breaks in bones weakened by primary hyperparathyroidism. Limiting alcohol consumption is also recommended since excessive drinking can interfere with proper nutrition needed for maintaining healthy bones.
Additionally, managing stress levels is essential for those living with this condition since high levels of stress hormones have been linked to decreased bone density over time.
Parathyroid disease then and Now
Parathyroid disease was largely a diagnosis made late in its clinical course up until the advent of routine blood calcium assessments in the 1970s. The period before the 1970s had patients developing kidney stones, kidney damage, severe fatigue and fractures long before a formal diagnosis could be made.
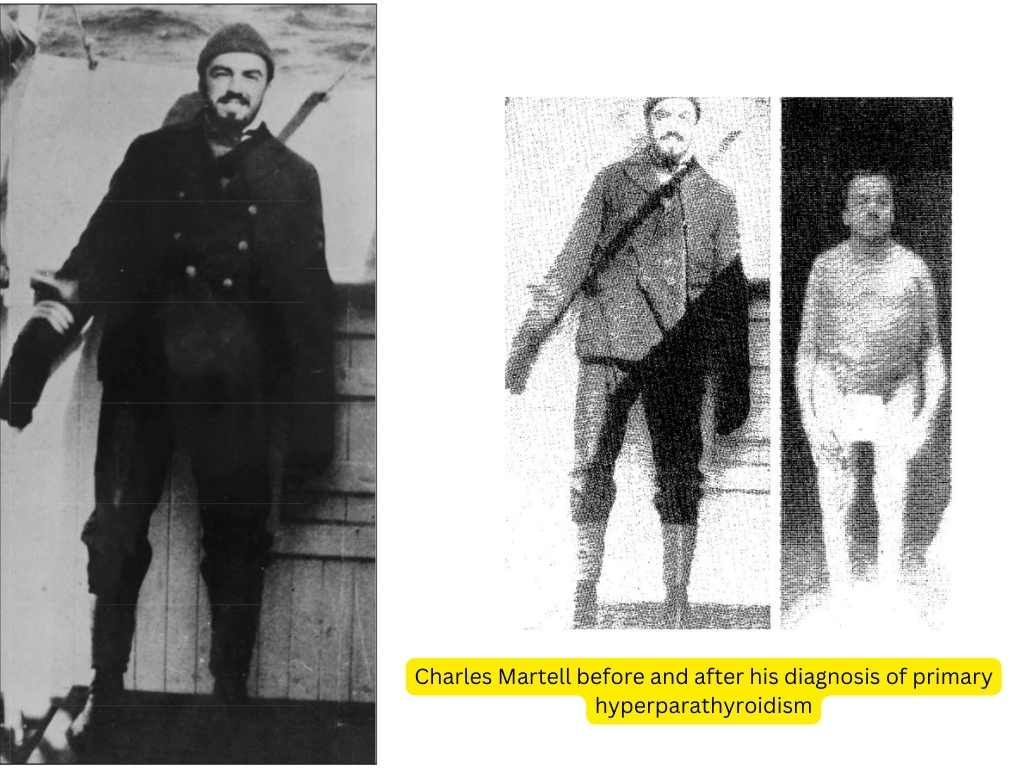
Charles Martell, a sea captain in the United States Merchant Marines was six feet tall at 22 years of age but shockingly was noted to be 7 inches shorter at 29 years of age due to a history of multiple fractures. He was eventually diagnosed with primary hyperparathyroidism and underwent a successful parathyroidectomy during his ninth parathyroid surgery in 1932. His parathyroid tumor was in an abnormal (ectopic) position in the chest, thus his previous unsuccesful surgeries.
Thankfully, doctors can now make a diagnosis of parathyroid disease long before it ravages the bones and kidneys. This is because blood calcium is evaluated on routine blood chemistry tests done as part of an annual physical. Thus the chances of developing the classic pentad of “bones, stones, groans, psychiatric moans, and fatigue overtones” is unlikely in these times.
FAQs in Relation to Primary Hyperparathyroidism
What is the most frequent cause of primary hyperparathyroidism?
The most frequent cause of primary hyperparathyroidism is an adenoma, which is a benign tumor of the parathyroid gland. This type of tumor causes the overproduction of parathyroid hormone, leading to elevated calcium levels in the blood and other symptoms associated with this condition. Other rarer causes include multiple adenomas, hyperplasia (an increase in number of cells), or carcinoma (cancer). Treatment typically involves surgical removal of the affected gland(s) to restore normal calcium levels and prevent further complications.
Should I take vitamin D if I have primary hyperparathyroidism?
Yes, it is recommended that people with primary hyperparathyroidism take vitamin D supplements. Vitamin D helps regulate calcium levels in the body and can help reduce symptoms of hyperparathyroidism such as bone pain or muscle weakness. It is important to talk to your doctor about what dose of vitamin D is right for you and how often you should take it. Additionally, make sure to monitor your calcium levels regularly when taking a supplement.
How serious is primary hyperparathyroidism?
Primary hyperparathyroidism is a serious medical condition that can lead to long-term health complications if left untreated. It occurs when one or more of the parathyroid glands produce too much parathyroid hormone, leading to an imbalance in calcium levels in the body. This can cause problems with bone density, kidney stones, and even heart failure. Early diagnosis and treatment are essential for preventing further complications from developing.
Conclusion
Primary hyperparathyroidism is a serious condition that can cause significant health issues if left untreated. It is important for patients to be aware of the symptoms, diagnosis, treatment options and potential complications associated with this condition in order to take proactive steps towards managing it.
With proper medical care and lifestyle changes, primary hyperparathyroidism can be managed effectively so that patients can live their lives as normally as possible. This comprehensive guide for patients provides an overview of primary hyperparathyroidism and serves as a valuable resource for those who are affected by this condition.
References
Casper S. Inexplicable patients: the case of Charles Martell and Ward 4 at the Massachusetts General Hospital. CMAJ. 2016 Dec 6;188(17-18):1263-1264.
The opinions expressed here represent the views of a practicing hormone specialist (endocrinologist) and must not substitute the advice of your health care provider. This blog post is written for a non-medical audience interested in learning more about hormonal disorders. The author has no commercial conflicts of interest to declare. Also, read our privacy policy.
Kindly Let Us Know If This Was helpful? Thank You!


