Pituitary apoplexy is a rare but serious endocrine emergency involving acute hemorrhage of the pituitary gland. Prompt diagnosis and treatment are crucial for patient outcomes.
Clinical presentation of pituitary apoplexy
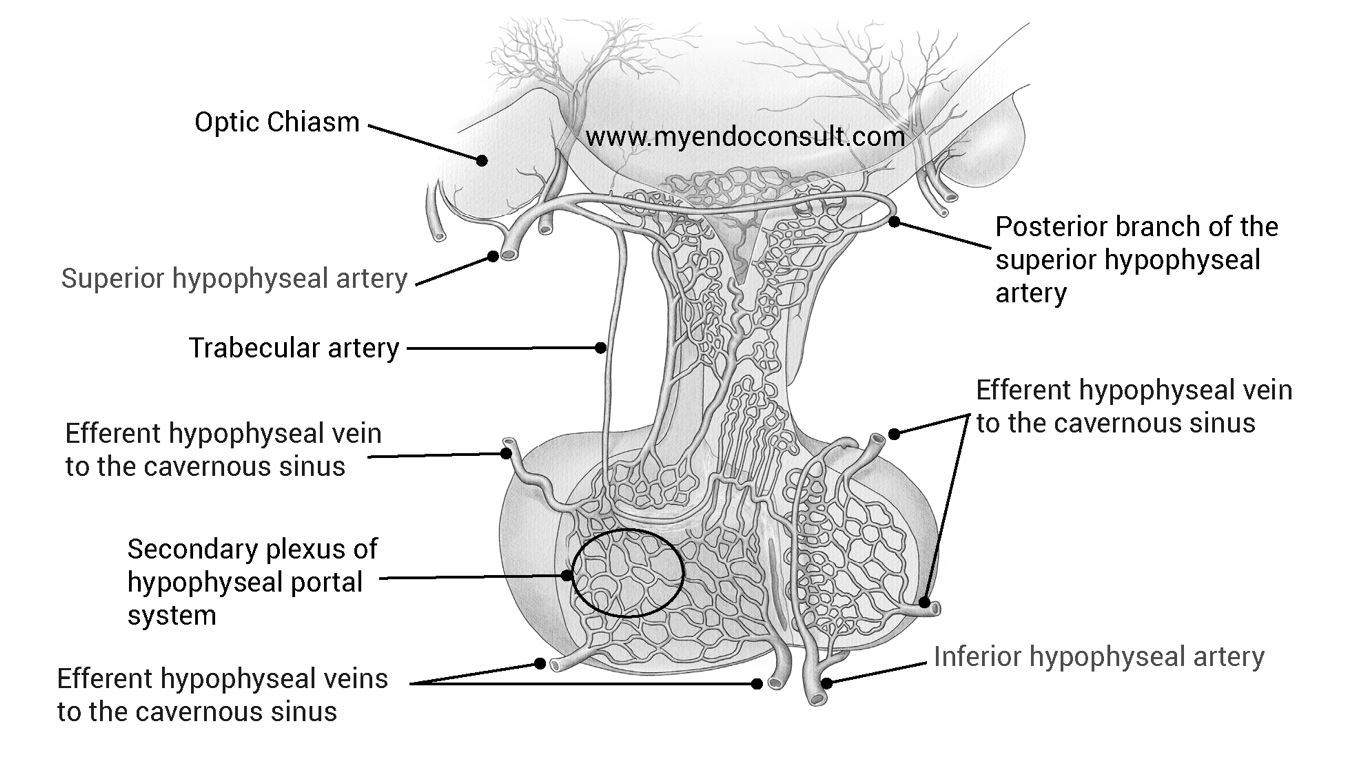
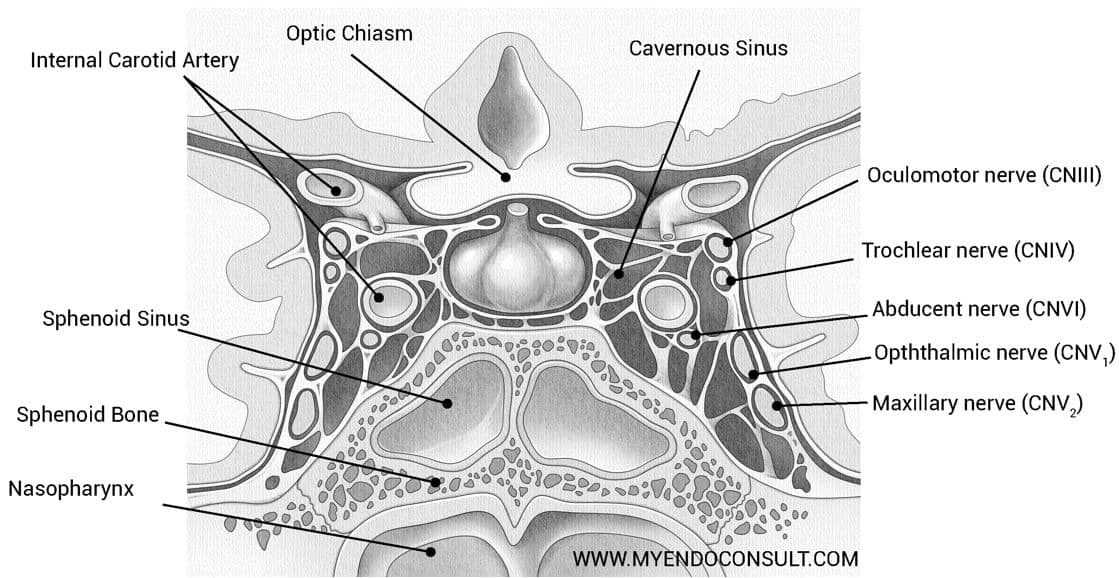
The typical symptoms include an acute onset of severe headache, often described as “the worst headache of my life,” vision loss (due to hemorrhagic expansion compressing the optic chiasm), facial pain, nausea, vomiting, and ocular nerve palsies (like ptosis and diplopia). These symptoms result from the compression of the third, fourth, and sixth cranial nerves in the cavernous sinuses.
Patients may also show signs of meningeal irritation, altered consciousness, and increased intracranial pressure, which can lead to drowsiness, stupor, and may require surgical intervention. Hypothalamic involvement can cause disorders in sympathetic autoregulation, leading to dysrhythmia and disordered breathing. The cerebrospinal fluid of many patients with pituitary apoplexy may show increased erythrocytes and protein concentration, which can be confusing in differentiating it from meningitis or subarachnoid hemorrhage.
The most immediate hormonal deficiency in pituitary apoplexy is secondary adrenal insufficiency, which can lead to hypotension and adrenal crisis. Pituitary apoplexy most commonly occurs in the context of a preexisting pituitary macroadenoma or cyst and can be spontaneous or triggered by various factors like head trauma, coagulation disorders, or anticoagulant administration. In rare cases, it can be induced by administration of hypothalamic-releasing hormones or agents used to treat pituitary tumors. The rapid expansion within the sellar region results in immediate mass-effect symptoms. Notably, in over 50% of cases, the apoplectic event is the first clinical indication of a pituitary tumor. The risk of pituitary apoplexy is not associated with age or gender.
Pituitary Apoplexy Imaging and Management
Magnetic Resonance Imaging (MRI) is essential for diagnosing pituitary apoplexy. MRI typically reveals signs of intrapituitary or intra-adenoma hemorrhage, fluid-fluid level, and compression of normal pituitary tissue. Hormonal evaluation usually indicates complete anterior pituitary failure, including prolactin deficiency. Due to the specific anatomy of pituitary circulation and sparing of the infundibular circulation, the posterior pituitary is rarely affected, making diabetes insipidus uncommon in pituitary apoplexy cases.
The clinical progression of pituitary apoplexy can vary greatly in both duration and severity, complicating the determination of appropriate treatment. The primary goal of intervention is to alleviate local compression on adjacent structures, such as the visual pathways. Treatment must also consider the patient’s endocrine status. The timing of therapy should be tailored based on the symptoms’ intensity and the apoplexy’s severity.
Neurosurgical intervention is often the most rapid and effective method for decompressing the sella turcica and surrounding structures. It is particularly indicated when there are mental status changes and other symptoms of increased intracranial pressure. Surgical decompression is also advisable when the visual pathways are at risk, even in the absence of symptoms, to prevent prolonged ischemia and irreversible nerve dysfunction.
While the timing of surgical intervention does not significantly impact the recovery of ocular palsies, performing surgery within one week of the apoplexy event can lead to a better recovery of visual acuity compared to delayed operations. Although hemorrhagic areas in the pituitary may be reabsorbed over time, relying solely on reabsorption may not be swift enough for the restoration of visual acuity.
Management of Pituitary Apoplexy and Long-term Considerations
In cases of pituitary apoplexy, waiting for a spontaneous resolution of a visual field defect in a stable patient might not be the best approach. However, for patients with normal visual fields and without cranial nerve palsies, observation is a reasonable treatment strategy. All patients with pituitary apoplexy should be started on stress dosages of glucocorticoids. It’s important to note that pituitary function may not fully recover, and many patients might require long-term pituitary target gland hormone replacement therapy.
It is also noteworthy that necrosis and hemorrhage within a pituitary tumor are more common occurrences than the full clinical syndrome of pituitary apoplexy. This is particularly true for silent corticotroph adenomas, where hemorrhage is seen in over 50% of cases. Overall, hemorrhage is found in about 10% to 15% of pituitary adenomas, but it often remains clinically silent.
Conclusion
In conclusion, pituitary apoplexy is a significant and potentially life-threatening condition characterized by the sudden hemorrhage or infarction of the pituitary gland. While it is an uncommon event, its recognition and timely management are critical due to the serious implications it has on a patient’s health. The typical presentation of pituitary apoplexy includes severe headaches, visual impairments, cranial nerve palsies, and occasionally, altered mental status and symptoms of increased intracranial pressure. These manifestations necessitate urgent medical and often surgical intervention.
Magnetic Resonance Imaging (MRI) plays a pivotal role in diagnosing pituitary apoplexy by revealing hemorrhagic changes within the gland. Treatment strategies vary depending on the severity of the symptoms. In cases with significant visual field defects or mental status changes, surgical decompression is often required to alleviate the pressure on adjacent structures. In contrast, patients without severe symptoms may be managed conservatively with careful observation.
A crucial aspect of managing pituitary apoplexy is addressing the hormonal deficiencies it causes. All patients should receive stress dosages of glucocorticoids to compensate for potential adrenal insufficiency. Furthermore, long-term management often involves hormone replacement therapy, as complete recovery of pituitary function is not always achievable.
It’s also noteworthy that while clinical pituitary apoplexy is rare, asymptomatic hemorrhage and necrosis within pituitary adenomas are relatively common, particularly in certain types of adenomas like the silent corticotroph adenomas.
In summary, pituitary apoplexy, though rare, is a medical emergency that requires prompt diagnosis and a tailored approach to management. Its complexity lies not only in the acute phase of the condition but also in the long-term hormonal and neurological implications it presents, underscoring the need for a comprehensive and multidisciplinary approach to care.
Quiz
Question 1:
What is the most common initial presentation of pituitary apoplexy?
A) Mild headache
B) Severe headache often described as “the worst headache of my life”
C) Sudden weight gain
D) High fever
Answer:
B) Severe headache often described as “the worst headache of my life”
Explanation:
The most common and characteristic initial symptom of pituitary apoplexy is a severe headache, which is frequently described by patients as “the worst headache of my life.” This symptom is due to the sudden hemorrhage or infarction in the pituitary gland, leading to increased intracranial pressure. Options A, C, and D are not typical initial presentations of pituitary apoplexy.
Question 2:
Which of the following is a critical step in the management of pituitary apoplexy?
A) Immediate chemotherapy
B) Administration of stress dosages of glucocorticoids
C) Immediate insulin therapy
D) Administration of high-dose antibiotics
Answer:
B) Administration of stress dosages of glucocorticoids
Explanation:
In the management of pituitary apoplexy, administering stress dosages of glucocorticoids is crucial. This is because pituitary apoplexy often leads to adrenal insufficiency due to impaired pituitary function. Glucocorticoids help manage this deficiency. Options A, C, and D are not standard treatments for pituitary apoplexy.
Question 3:
What is a common finding on MRI in a patient with pituitary apoplexy?
A) Enlarged liver
B) Signs of intrapituitary or intra-adenoma hemorrhage
C) Enlarged spleen
D) Calcification in the pituitary gland
Answer:
B) Signs of intrapituitary or intra-adenoma hemorrhage
Explanation:
Magnetic Resonance Imaging (MRI) in patients with pituitary apoplexy typically shows signs of intrapituitary or intra-adenoma hemorrhage. This finding aligns with the nature of pituitary apoplexy, which involves acute hemorrhage or infarction of the pituitary gland. Options A, C, and D are not typically associated with MRI findings in pituitary apoplexy.
Kindly Let Us Know If This Was helpful? Thank You!


