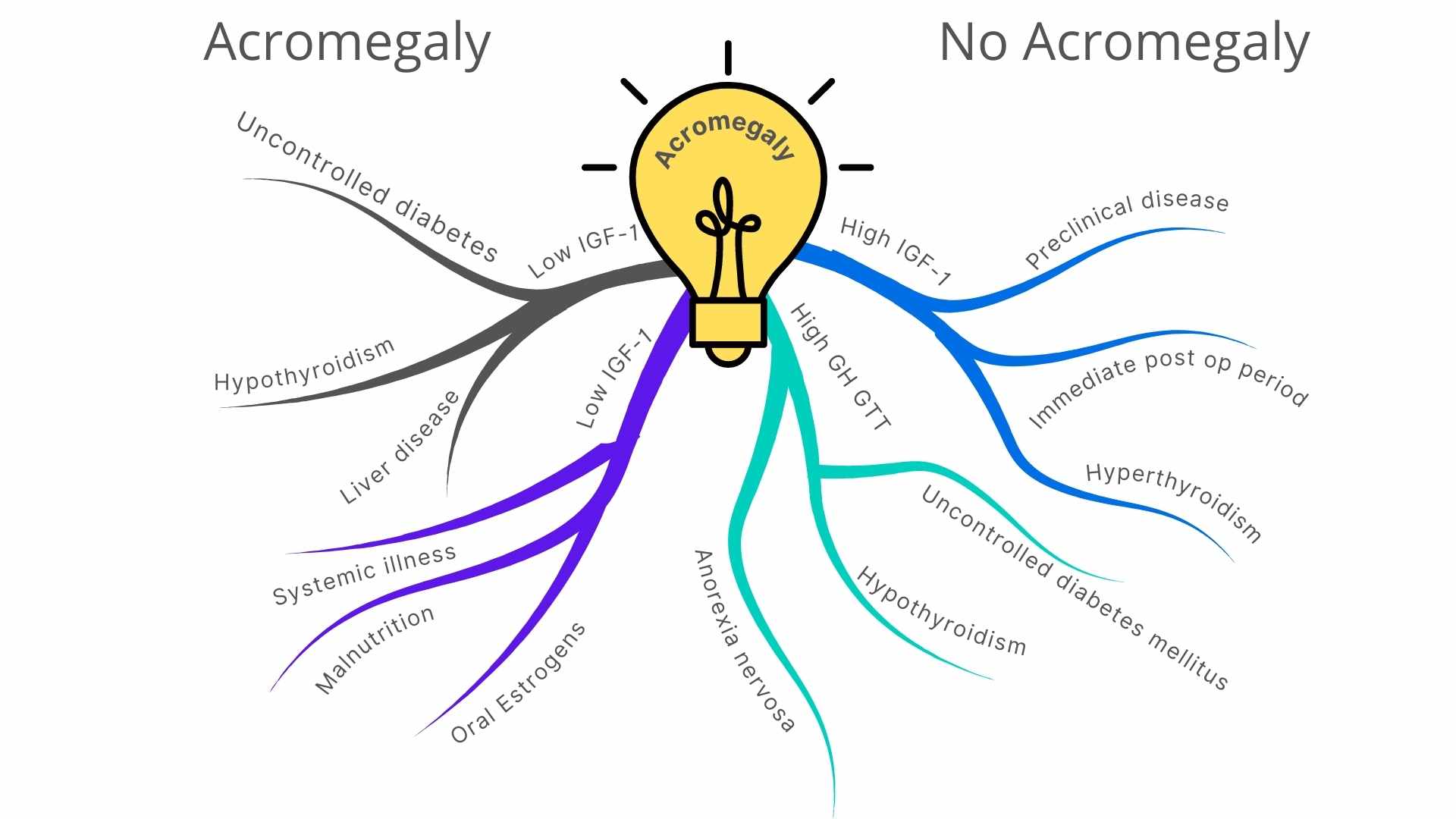
The role of IGF-1 and growth hormone assay in the evaluation of acromegaly. Various conditions may lead to spurious lowering of growth hormone and IGF-1, even in patients with acromegaly.
IGF-1 testing
The best screening test for acromegaly (growth hormone excess) is serum insulin-like growth factor 1 (IGF-1). IGF-1 has a sensitivity and specificity for acromegaly of 97% and 90%, respectively.
Causes of low IGF-1 in patients with acromegaly
In normal physiology, the production of IGF-1 (both hepatic and extra-hepatic) sites is facilitated by thyroxine, testosterone, insulin, and estrogen (low levels). Conversely, IGF-1 production is inhibited by inflammatory cytokines. When the clinical features do not match biochemical testing, these conditions should be considered and excluded.
- Uncontrolled diabetes mellitus
- Hypothyroidism (both primary and secondary hypothyroidism)
- Male Hypogonadism
- Chronic liver disease
- Chronic renal failure
- Malnutrition
- Systemic illness
- Oral estrogen therapy
Causes of elevated IGF-1 without acromegaly
- Preclinical disease (acromegaly)
- Hyperthyroidism
- Immediately after surgery (for acromegaly). Due to the long-circulating half-life of IGF-1 (12 to 15 hours)
- After surgery (for acromegaly)
Glucose suppression testing
The gold standard confirmatory test for acromegaly is the glucose suppression test. An inability to appropriately suppress serum growth hormone (GH) below 1ng/ml after a 75g oral glucose load.
These are causes of elevated (non-suppressible) GH after a glucose tolerance test
- Uncontrolled diabetes mellitus
- Hypothyroidism
- Pubertal growth spurt
- Pregnancy
- Depression
- Chronic liver disease
- Chronic kidney disease
- Anorexia nervosa.
Clinical Question
A patient with clinical features of acromegaly, elevated IGF-1, and a non-suppressed growth hormone (after an oral glucose load) has no demonstrable adenoma on pituitary imaging. What are the possible differential diagnoses?
- Silent apoplexy of a somatotroph tumor
- An ectopic source of Growth hormone-releasing hormone (GHRH) neuroendocrine tumor
- An ectopic source of Growth hormone (GH) neuroendocrine tumor
- McCune-Albright syndrome
- An ectopic pituitary adenoma (sphenoid sinus)
References
Laurence Katznelson, Edward R. Laws, Jr, Shlomo Melmed, Mark E. Molitch, Mohammad Hassan Murad, Andrea Utz, John A. H. Wass, Acromegaly: An Endocrine Society Clinical Practice Guideline, The Journal of Clinical Endocrinology & Metabolism, Volume 99, Issue 11, 1 November 2014, Pages 3933–3951
Images(s) Courtesy
MyEndoConsult
Kindly Let Us Know If This Was helpful? Thank You!


