Introduction
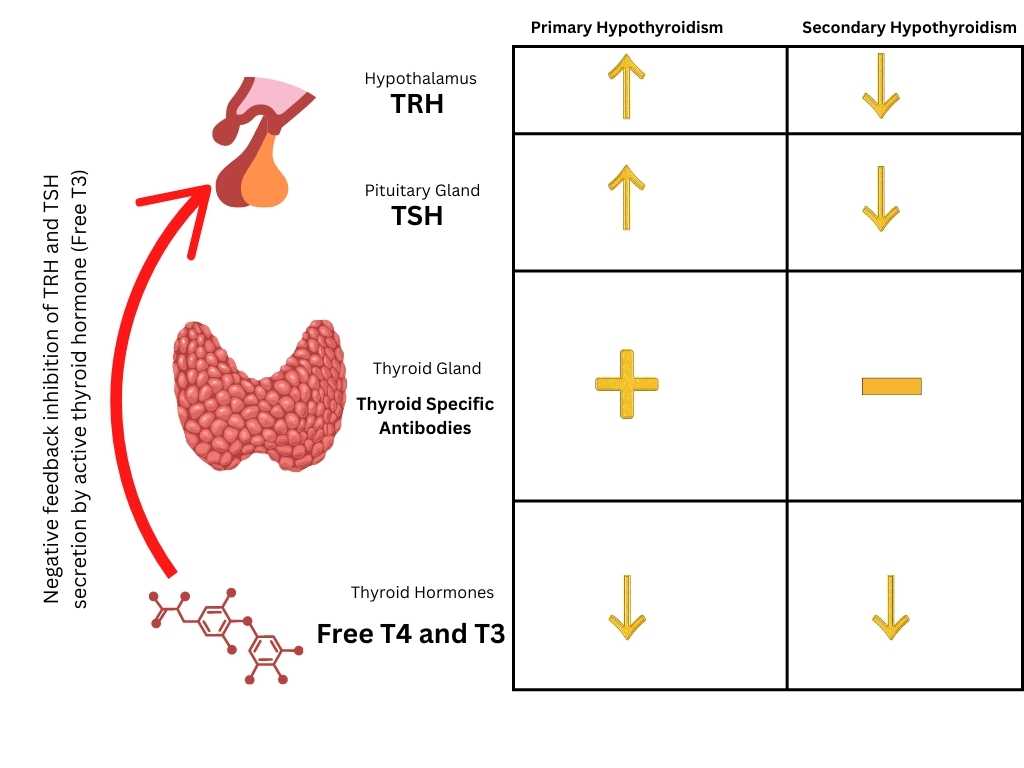
As with the other endocrine glands controlled by the anterior pituitary, hypofunction of the thyroid gland can be divided into a primary form due to failure of thyroid tissue itself and a secondary form due to a deficiency of TSH secretion. Plasma TSH is elevated in the former and low in the latter case. In primary hypothyroidism, the thyroid gland is already under intense stimulation by endogenous TSH, and injection of TSH has no further stimulatory effect. In secondary hypothyroidism the thyroid responds well to exogenous TSH.
Myxedema describes alterations in the skin that are often but not always found in hypothyroid patients. Some authors use the term interchangeably with hypothyroidism, others only for severe forms of the disease. Endemic cretinism occupies a special place in the classification. Hypothyroidism does not explain all its features and incidentally is not always present in endemic cretins
The difference between Primary and Secondary Hypothyroidism
| Primary hypothyroidism | Secondary Hypothyroidism |
|---|---|
| Elevated TSH | Low or inappropriately normal TSH |
| Low Free T4 | Low Free T4 |
| Failure of the thyroid gland | Pituitary Dysfunction leading to reduced TSH secretion |
| Coarse, thick, dry and yellowish skin of myxedema | Pale white, finely wrinkeled skin |
| less likely to have additional endocrine disorders at presentation | Additional endocrine disorders likely (hypogonadism, adrenal insufficiency) |
| Significant declined in basal metabolic rate (may be below 40%) | Reduction in basal metabolic rate is rarely below 30% |
| Presence of thyroid specific antibodies (thyroid peroxidase, Thyroglobulin antibody) | Absence of thyroid specific antibodies |
Secondary hypothyroidism occurs most frequently in the setting of panhypopituitarism, Occasionally, TSH deficiency is the predominant feature of a pituitary lesion, and gonadal and adrenal function are less compromised. In such cases, it may be difficult to differentiate secondary hypothyroidism from primary myxedema on clinical grounds.
The differentiation of secondary from primary hypothyroidism is of more than academic interest and influences the choice of treatment for the patient.
In secondary hypothyroidism, due to the frequent coexistence of adrenocortical insufficiency, thyroid hormone substitution may provoke a potentially fatal adrenal crisis if corticosteroids are not given simultaneously.
The clinical sign most useful in differentiation is the white, almost transparent, and finely wrinkled skin of secondary hypothyroidism, as opposed to the coarse, thick, dry, and slightly yellowish skin of primary myxedema.
Amenorrhea, atrophy of the testes, adrenal insufficiency, and tendency to hypoglycemia are all points indicative of secondary thyroid failure. Pubic and axillary hair is sparse in primary hypothyroidism, but their complete absence is additional support for diagnosing secondary hypothyroidism.
Urinary corticosteroid excretion is moderately diminished in primary myxedema but very low in panhypopituitarism. In hypopituitarism, the thyroid gland retains a certain degree of autonomic function so that thyroid failure is rarely as severe as it sometimes is in primary myxedema. In complete failure of the thyroid gland the basal metabolic rate may fall to 40 %, whereas in secondary failure it is rarely below 30 %.
The presence of serum antibodies to thyroid antigens provides strong support for the diagnosis of primary hypothyroidism. On average, serum cholesterol is less elevated in secondary than in primary hypothyroidism, but in the individual patient this sign is of little value for differentiation. The diagnosis of secondary hypothyroidism is established by the finding of a low or low normal serum TSH concentration. In primary hypothyroidism serum TSH is always elevated.
Where TSH measurements are not available, the TSH stimulation test will show a good response of the serum thyroxine and the radioiodine uptake to repeated injections of bovine TSH. It must be added that longstanding primary hypothyroidism may impair the function of the anterior pituitary and the term myxedema of the pituitary is sometimes used to describe this condition.
primary vs secondary hypothyroidism
Clinical Findings in Primary and Secondary Hypothyroidism
History and Mental Changes
The onset is insidious, and overt hypothyroidism does not develop until a large part of the thyroid tissue has been destroyed. The pathologic process in the gland precedes the appearance of overt hypothyroidism by the years. Hypothyroid patients rarely mention symptoms spontaneously. Since they are often over 60, they are simply considered senile or sometimes even insane by their relatives, and a high index of suspicion is needed to make the diagnosis in mild cases.
One of the earliest complaints is intolerance of cold. The patient feels more uncomfortable than previously and uses an extra blanket at night, and may also perspire less than before. The patient sometimes notices changes in mental function but often by his/her relatives. Also, the patients complain of fatigue (not a very specific symptom), and they sleep a lot, preferably in a well-heated room.
The mental changes are often quite similar to those in cerebral atherosclerosis. The functions of memory and critical judgment are impaired. In the early stages, the patient may be capable of good judgment and of making decisions, but his thought processes are slow. The sexual drive is diminished. In later stages, a state of mental dumbness with a loss of interest in the surroundings and of most previous personality traits prevails.
Occasionally the mental changes progress into acute delirium, which is clinically indistinguishable from delirium due to exogenous causes but can be differentiated by the presence of slow waves and low voltage in the EEG. The delirium may progress to stupor and coma. Other patients show changes identical to those in classic manic-depressive or acute schizophrenic psychosis. In some cases, this may be due to a true underlying psychosis which becomes manifest in thyroid failure.
In mild cases, mental processes may not be slowed down. Occasionally the symptoms are more similar to those of excitation and even suggest the diagnosis of hyperthyroidism at first.
General Appearance
It has been said that hypothyroid patients all look alike. Indeed full-blown cases can be unmistakably recognized at first glance from the typical facies.
The individuality of the in a well-heated room wearing more clothes facial features is diminished. Mimic movements are few and slow, although still present, in contrast to Parkinson’s disease. The patients look sleepy, but happy. No other endocrine disease changes the facies of a person so completely as myxedema.
The voice is characteristically low pitched and hoarse with a nasal undertone, and the speech is slow and monotonous, badly articulated like that of a person under the influence of alcohol. These changes are sometimes so characteristic that the experienced physician can make the diagnosis when speaking to the patient on the telephone.
Skin (Integument)
Cutaneous vasoconstriction and myxedema makes the skin waxy and pale. Sometimes it has a pink or yellowish undertone due to the deposition of carotene, the hepatic conversion of which to vitamin A is impaired. Carotene can also be the cause of a peculiar malar flush which looks rather like badly applied make-up. Swelling is particularly noticeable in the eyelids and produces narrowing of the palpebral fissures.
In addition, the upper eyelid is often slightly ptotic, an effect ascribed to a decreased tone of Mueller’s muscle, which is innervated by the sympathetic nervous system. The tongue is thickened and immobile, sometimes even protruding. Scalp hair becomes coarse and fragile, and loses its luster. It falls out easily and frontotemporal baldness ensues.
The eyebrows fall out completely or more often only on the lateral part. Myxedematous changes are often found diffusely in the entire skin but sometimes remain localized in a few well-demarcated areas, particularly over the anterior aspect of the legs. Myxedema is characteristically nonpitting, but in the lower extremities true interstitial pitting edema is observed, sometimes to a grotesque degree. The skin is cool, dry, rough, and scaly, with increased cornification on the elbows and knees.
The fingernails are thin and brittle and grow slowly. The body temperature falls to 35-36 Celsius (95.0-97.7 Fahrenheit), and in extreme cases potentially fatal hypothermia develops. Contrary to popular belief, generalized obesity is only rarely found in hypothyroidism, but localized accumulation of fat over the clavicles does occur. Beard and pubic hair growth is diminished, although not to the same degree as in hypopituitarism. Wound healing is delayed.
Thyroid Gland
In idiopathic hypothyroidism the thyroid gland is usually not palpable and goiter is only rarely recorded. Thus, the presence of a goiter does not exclude the possibility of hypothyroidism. The association of a large goiter and hypothyroidism is suggestive of an hereditary defect in hormone biosynthesis.
Cardiovascular System and Plasma Lipids
In severe myxedema the heart is diffusely enlarged due to myxedematous infiltration of the myocardium, loss of tone, and dilatation of all cavities. Thyroxine treatment alone may bring about a reduction in heart size. In advanced cases, pericardial or pleural effusions and sometimes ascites are present. The heart sounds are diminished. Classically there is bradycardia, but this sign is not always present.
Contrary to many textbook statements the blood pressure, in particular the diastolic pressure, is moderately elevated in 50 % of cases of hypothyroidism. The stroke volume and cardiac output are diminished, but in contrast to the situation in cardiac failure the arterio-veinous oxygen difference remains normal. Manifest heart failure is infrequent and, when it is present, is often due to additional factors.
In mild cases the electrocardiogram shows flattening, and occasionally inversion, of T waves. The QT interval remains normal, but the PQ interval and QRS complexes sometimes become wider. In advanced cases the characteristic low voltage appears. This cannot be attributed solely to increased electrical resistance of the myxedematous skin, as measurements with deep-needle electrodes have shown. The electrocardiographic changes are most probably related to the myxedematous changes in the myocardium.
Plasma cholesterol is usually elevated in hypothyroidism, but due to the wide normal range this laboratory sign is of little diagnostic value. The rate of cholesterol synthesis appears to be normal (or even slightly low) in hypothyroidism, and the cause of the high plasma level appears to be slower removal.
Triglycerides are also elevated, but frank hyperlipemia is rare. The cause of the hypertriglyceridemia is a low fractional triglyceride removal rate, possibly due to a low lipolytic activity.
A diet low in saturated fat may reduce the cholesterol, but not the triglyceride plasma level. Thyroid hormone treatment normalizes both values. The relationship of hypothyroidism and the concomitant hypercholesterolemia to coronary artery disease is complex.
One of the clinical consequences is that coronary insufficiency may become manifest when substitution therapy with thyroid hormone is instituted in a myxedematous patient.
Treatment should therefore begin with very low doses, and in the patient over 50 years of age it is often necessary to compromise over the final maintenance dose, which should be such that the patient remains borderline hypothyroid, because on full substitution many patients suffer from intractable angina pectoris (use this levothyroxine dosage calculator in hypothyroidism)
Alimentary Tract
The poor appetite is compensated by the diminished metabolism so that there is no loss in body weight. Difficulty in swallowing and the feeling of a lump in the throat are often early symptoms of hypothyroidism.
The submaxillary salivary glands are sometimes moderately enlarged. Obstinate constipation results from the reduced food intake, reduced metabolism and sluggish peristalsis. In 50 % of cases there is histamine-refractory achlorhydria. The number of parietal cells in the fundus of the stomach is reduced, and true pernicious anemia is frequently found. The intestinal atony leads to the disturbing symptoms of flatulence and meteorism, and abdominal pains can simulate an ileus. True ileus due to fecal impaction is a much-dreaded complication.
Respiratory System
The alveolar-arterial difference in partial oxygen pressure during respiration of 100 % oxygen is greatly elevated in myxedematous patients. Induction of hyperventilation decreases the alveolar-arterial p02 difference, and the abnormalities are reversible after thyroid hormone treatment. The most likely explanation for these findings is an increase in intra-pulmonary vascular shunts, which may be due to underventilation or atelectasis of small pulmonary segments.
Blood
Cutaneous vascoconstriction causes hypothyroid patients to look very pale. This may be why the early literature described anemia as a frequent complication of hypothyroidism. More recent studies have yielded completely normal hematological findings in two-thirds of patients with hypothyroidism, apart from the fact that most patients have a decreased total red-cell mass associated with the decreased blood volume.
Several forms of anemia have to be considered in connection with hypothyroidism. In so-called “uncomplicated” anemia of hypothyroidism the hemoglobin is moderately low. There is normocytosis or slight macrocytosis.
Plasma iron is moderately lowered and the plasma iron turnover rate is decreased. Incorporation of iron into erythrocytes is normal, as is the erythrocyte survival time. The bone marrow may be moderately hypoplastic. Thyroid hormone substitution therapy reverses all these hematological changes.
The pathogenesis of this type of anemia is not entirely clear. Most authors relate it to decreased oxygen requirements and a consequent drop in erythropoeitin levels. Recently it has also been shown that thyroid hormone stimulates hemoglobin biosynthesis in bone-marrow culture. The observation that thyroid hormone stimulates 2,3-diphosphoglyceric acid synthesis in red cells may also be relevant in this context.
Iron-deficiency anemia with all the associated hematological findings is present in 15 % of patients with hypothyroidism. In most cases it can be related to the severe menorrhagia which often accompanies hypothyroidism in women. These patients need iron therapy and hormonal substitution to completely normalize the blood findings.
Pernicious anemia is found in 8 % of patients with hypothyroidism, in comparison to 0.35 % of matched controls. The present view is that these patients suffer from true pernicious anemia and that idiopathic hypothyroidism is pathogenetically related to this disease. The fact that true pernicious anemia is also more frequent in patients with Graves’ disease may explain the above association between postsurgical or post-radioiodine hypothyroidism and pernicious anemia.
Antibodies to mucosa of the gastric fundus and intrinsic factor are prevalent in patients with idiopathic hypothyroidism, as they are in pernicious anemia. They are rare in control subjects. Patients with pernicious anemia do quite often have serum antibodies to thyroid tissue, however. Gastric mucosal biopsies in hypothyroid patients (in some studies) reveals a reduction in the number of parietal cells and lymphocytic infiltrates. Nearly 50 % of patients with hypothyroidism suffer from histamine-refractory achlorhydria.
Both pernicious anemia and idiopathic hypothyroidism are currently viewed as disorders of autoimmunity, possibly related to a generalized defect of immune tolerance. The two conditions are clinically similar and clinical differential diagnosis may be difficult at times.
It is advisable to assess the thyroid status of every patient suffering from pernicious anemia. In addition, whenever thyroid hormone and iron substitution do not cure anemia of hypothyroidism, intestinal vitamin B12 absorption or serum vitamin B12 levels should be measured. Leukocytes and platelets are normal in hypothyroidism. The erythrocyte sedimentation rate is usually accelerated.
Genital Organs and Gonads
Hypothyroid women often suffer from menorrhagia, but ammenorrhea is also encountered. Sterility in both sexes is common, but occasional pregnancies do occur in hypothyroid women. The sexual drive is usually reduced and impotence is not uncommon. Occasionally men suffer from coincident hypogonadism and hypothyroidism.
Muscles and Joints
The strength of the hypotonic and very often pseudohypertrophic musculature is reduced. Muscle pain and stiffness are common complaints. Tapping the muscle produces the typical pseudomyotonic reaction in the form of a slow contraction changing into a hard muscular ridge.
These contractions never outlast the voluntary innervation as they do in myotony. The tendon reflexes are characteristically very sluggish, and the recording of the ankle jerk shows a typical curve, which is useful in diagnosis.
Hypothyroidism can produce severe histological changes in muscle characterized by peculiar mucoid deposits between and within muscle cells. The serum creatine phosphokinase (CPK) is elevated, indicating muscular damage. Similar changes occur in smooth muscle. They may lead to degenerative changes in the media of large blood vessels and to rupture of the aorta. Hypothyroidism may be associated with myasthenia gravis.
Arthralgia, joint swelling, synovial thickening and joint effusions are sometimes the prominent features of hypothyroidism, and such patients are referred to rheumatology units before the diagnosis of hypothyroidism is established. Most of the symptoms disappear during thyroid hormone substitution therapy.
Nervous System
Cerebellar dysfunction with ataxia and intention tremor occur occasionally. Sensory disturbances are more common, and the patients often complain of numbness and paresthesias. Compression of the median nerve with carpal tunnel syndrome is often encountered.
The protein concentration in the cerebrospinal fluid, particularly that of gamma globulin, is frequently elevated. Partial deafness is a frequent finding in adult hypothyroidism. The pathogenesis is not quite clear. It appears to be due to a conductive defect associated with swelling in the eustachian tube. Sensorineural deafness has been ascribed to degenerative changes in the mucosa of the cochlea and sometimes to changes in the labyrinthine fluid composition.
Kidney, Electrolytes and Body Fluids
Morphologically the kidneys may show deposits of mucopolysaccharides in the intercapillary space and in the basal membranes of the tubuli. Electron microscopic examination reveals thickening of the glomerular and tubular basal membranes. Clinically, oliguria is sometimes observed and is attributed to a low fluid intake. Slight proteinuria is often present.
Laboratory examination of kidney function has revealed a decrease of glomerular filtration rate and renal plasma flow. These changes in kidney function rarely lead to overt electrolyte disturbances. Occasionally, however, particularly in severe myxedema and in myxedema coma, dangerous hyponatremia develops.
Superficially this form of hyponatremia resembles that seen in the syndrome of inappropriate secretion of antidiuretic hormone (ADH), since plasma osmolality is low and urine osmolality high. The disturbance was therefore initially ascribed to inappropriately high levels of antidiuretic hormone. Further studies however have shown that the pathogenesis of this electrolyte disturbance is far more complex and cannot yet be fully explained.
So far it is established that the hyponatremia is dilutional, i.e. total exchangeable body sodium is normal or slightly increased and total body water is definitely increased. Although resetting of the osmoreceptors to a lower level may play some role, and maintain the serum sodium at borderline low levels by the secretion of ADH, the control of ADH secretion is not lost.
When given a water load these patients are perfectly capable of diluting their urine to 60 mOsm/K/H2O, although the peak urine flow and the free water clearance are lower than in controls. The minimum urine osmolality reached is slightly higher than in normal persons.
The best explanation for the hyponatremia of hypothyroidism so for available is that it is due to a decreased volume and solute delivery to the distal diluting tubular segment. Decreased glomerular filtration and increased proximal sodium reabsorption may both contribute to this decreased volume delivery to the distal tubule. It must be added that a relative lack of corticosteroids may also be involved in the hyponatremia, but this is less well established.
Diagnostic Utility of clinical findings.
In summary, symptoms which are significant for the distinction between hypothyroidism and euthyroidism are diminished perspiration, preference for warm ambient temperatures, hoarseness of the voice, paresthesias, and dry skin. The most significant signs are slowness of the ankle jerk, slow movements on undressing, and dry rough skin on the forearms.
Contrary to popular belief, weight gain has practically no diagnostic value. This is contrary to what most patient’s believe. Ask any practicing endocrinologist if hypothyroid patients accept the fact that hypothyroidism seen in outpatient practice is highly unlikely to be the reason for significant weight gain.
Kindly Let Us Know If This Was helpful? Thank You!


