Levothyroxine Dosage Calculator
Doses of levothyroxine (convert the estimated dose of levothyroxine to the closest dose)
| Plan | Recommendations |
|---|---|
| Initial Dose | Low dose (25-50mcg once daily) especially in the elderly and those with significant heart disease. Standard Dosing : 1.6mcg per kilogram body weight (young, healthy patients). For subclinical Hypothyroidism (high TSH, normal free T4) start with 50% of the weight based estimate |
| Dose Adjustments | TSH should be checked every 6weeks until TSH is at goal. TSH goal <2.5 (not the typical reference range of 0.5-4.5) |
| Monitoring | After stabilization of thyroid function, check TSH every 6-12 months or if the clinical situation warrants it. |
| Conditions requiring escalating doses | Malabsorption (celiac disease), medications that impair LT4 absorption (divalent cations like iron, magnesium and calcium), Medications that increase thyroxine metabolism (phenytoin, carbamazepine, rifampicin), Obesity, Low protein states (nephrotic syndrome, severe chronic liver disease). |
| Conditions requiring lower doses | Recent significant weight loss |
Approximating the suggested dose of levothyroxine
- 25mcg : Orange
- 50mcg : White
- 75mcg : Violet
- 88mcg : Olive
- 100mcg : Yellow
- 112mcg : Red
- 125mcg : Brown
- 137mcg : Turquoise
- 150mcg : Blue
- 175mcg : Lilac
- 200mcg : Pink
- 300mcg : Green
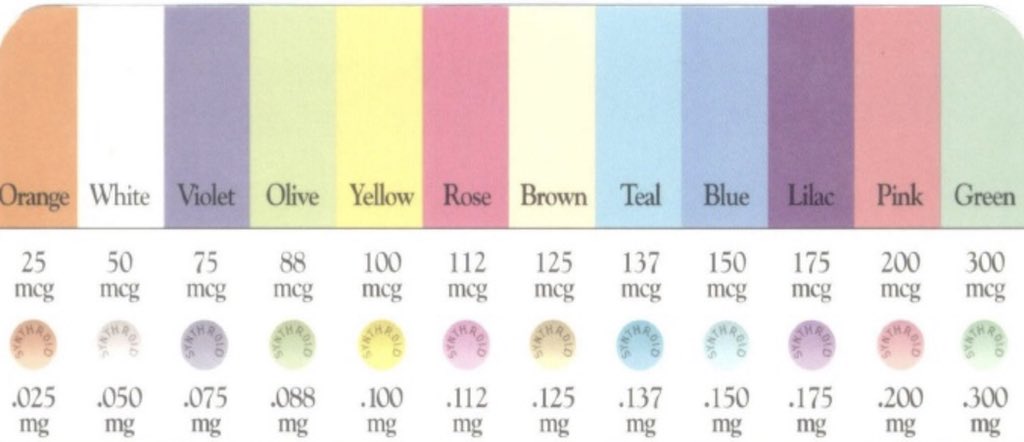
Image source @CaseyMcQuadeMD via twitter. Refer to this post for a simple memory aid to recall the colors and doses of levothyroxine
Starting dose of levothyroxine
What is the recommended dose of LT4 for replacement therapy in a patient with hypothyroidism?
In healthy, young patients, the recommended full replacement dose of levothyroxine is (1.6 mcg/kg/day). This dose is suggested in athyroidal patients (e.g. postsurgical hypothyroidism).
On the other hand, for elderly patients and subjects with known or suspected cardiovascular disease, “start low and go slow”. These patients should be started on levothyroxine (25–50 mcg/day). These can increased by 25 mcg/day every 4 to 6 weeks until the TSH reaches the expected goal.
Also, for patients with subclinical hypothyroidism, it is best to start 50% to 75% of the predicted full replacement dose of levothyroxine.
Interpretation of thyroid function tests
TSH levels are elevated in even very mild primary hypothyroidism and are suppressed to <0.1 μU/mL in mild hyperthyroidism. Consequently, a normal plasma TSH level effectively excludes hyperthyroidism and primary hypothyroidism.
Also, changes in plasma TSH tend to lag behind changes in plasma T4. For this reason TSH levels may be misleading when plasma T4 levels are changing rapidly, as may occur during treatment of hyperthyroidism, or in the first few weeks after changes in the dose of thyroxine.
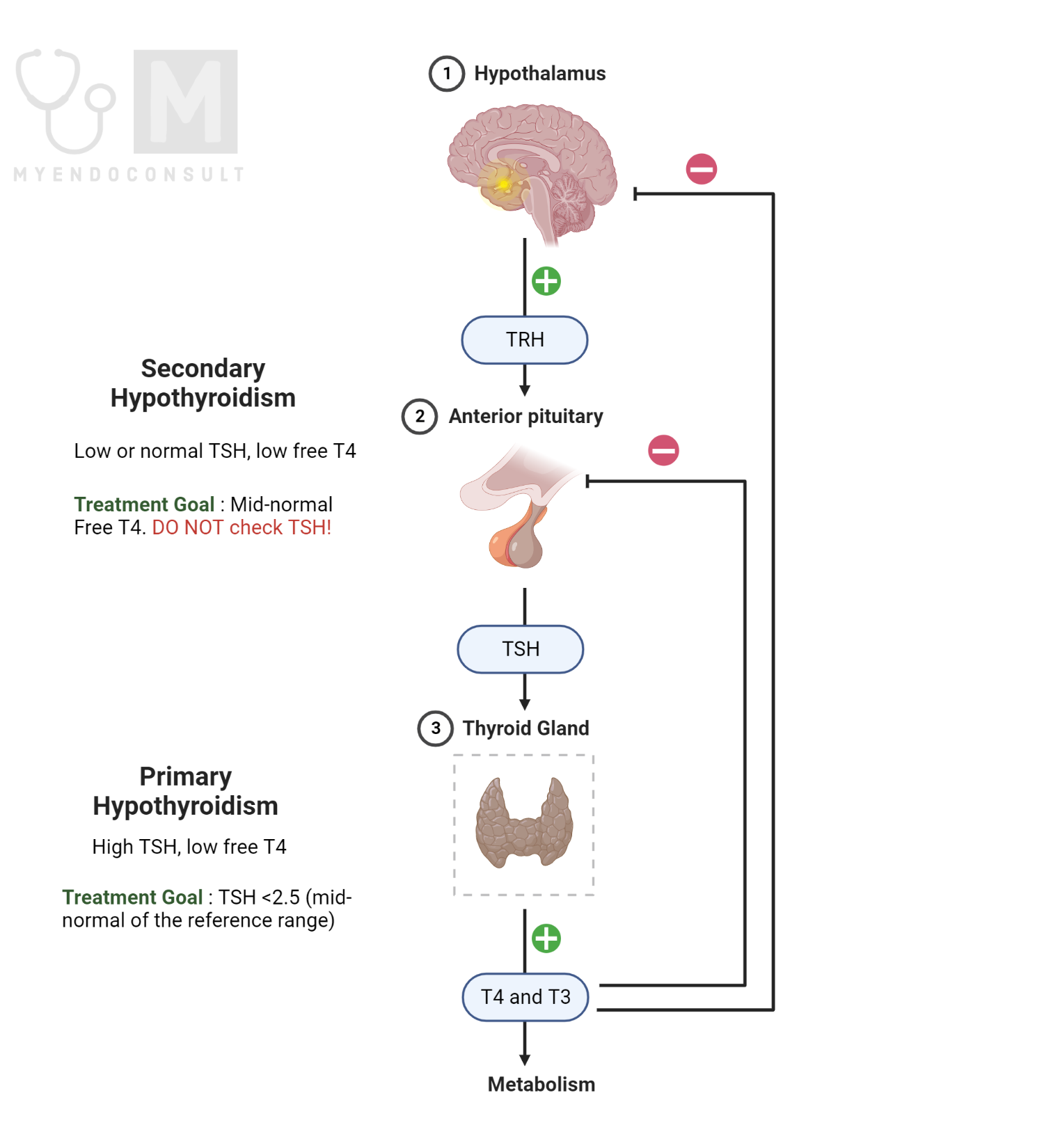
The goal TSH for the treatment of primary hypothyroidism
The treatment goal for patients with primary hypothyroidism is TSH range of 0.5 to 2.0 mU/L. Historically the conventional TSH range of 0.5-5 mU/L was based on a cohort of subjects that included those with antithyroid antibodies (occult autoimmune thyroid disease). For this reason, the “normal” range of TSH is thought to be skewed towards the higher TSH values. Indeed, when normal subjects with no thyroid autoimmunity were evaluated, most had TSH values below the mid normal point i.e., 2.5 mU/L.
Monitoring of levothyroxine therapy
Time interval | Plan |
Initial Dose adjustment | Monitor serum TSH every 4-6 weeks |
Maintenance therapy | Monitor TSH every 6-12 months |
Combination treatment of hypothyroidism
When should you consider combination T4/T3 therapy?
For patients who continue to report subjective hypothyroid symptoms, a brief trial of combination levothyroxine and liothyronine may be considered. It is generally recommended that other causes of fatigue such as anemia (due to B12 deficiency) and sleep apnea be ruled out before initiating dual T3+T4 therapy. A conversion factor of 25-50mcg (levothyroxine) to 5-10mcg (liothyronine) is reasonable approach. For example, the dose of levothyroxine can be reduced by 25mcg daily at the time of initiation of liothyronine (a dose of 5mcg administered in the morning).
For patients on dual therapy, the TSH nadir is approximately 10 hours after administration of T3. It is therefore best to monitor TSH in the early morning, prior to LT3 administration.
Clinical factors that can alter TSH
Numerous factors can potentially result in significant fluctuations in serum TSH of patients treated with thyroid hormone. Even more importantly, it should also be remembered that there is a ciracadian rhythm in serum TSH. For this reason, TSH can vary to the order of 2mIU/L during a 24 hour period of evaluation.
Causes of increased TSH (increased levothyroxine requirement)
- Weight increase
- Pregnancy
- Impaired absorption (calcium carbonate, phosphate binders, iron supplements, cholestyramine, sucralfate)
- Increased thyroxine binding globulin (estrogen)
- Increased metabolism of levothyroxine (antiepileptic agents, tyrosine kinase inhibitors)
- Gastritis
- Missed doses of levothyroxine
- Timing of levothyroxine intake close to meal intake
Causes of decreased TSH (decreased levothyroxine requirement)
- Weight decrease
- Decreased thyroxine-binding globulin (androgens)
- Additional levothyroxine doses by the patient
- Medications (Metformin, statins, high dose vitamin C, Glucocorticoids, Bexarotene)
For patients who remain persistently hypothyroid after multiple dose adjustments and ruling out obvious causes of malabsorption, consider a formal levothyroxine absorption test.
Kindly Let Us Know If This Was helpful? Thank You!


