Facial plethora is a condition characterized by facial erythema. It is often caused by an increase in blood flow to the area. Facial plethora can be a side effect of certain medications, such as birth control pills, beta-blockers, and angiotensin-converting enzyme inhibitors. It can also be caused by conditions that cause an increase in blood pressure, such as pregnancy, obesity, and sleep apnea. Facial plethora is typically a benign condition and does not cause any symptoms.
However, in rare cases, it can be a sign of a more serious condition such as Cushing’s syndrome. The clinical features, causes, underlying mechanisms, and treatment of facial plethora will be reviewed next.
Cushing’s syndrome
Clinical finding
Facial plethora is a common clinical finding in patients with hypercortisolism [1] and is highly predictive of Cushing’s syndrome (pituitary or adrenal gland as the cause of endogenous hypercortisolism). Of note, the other positive discriminatory findings of endogenous hypercortisolism include easy bruising, proximal myopathy, and purplish striae >1cm [2].

Mechanism
Investigators at the National Institutes of Health (NIH) quantified vascular flow rates in patients with Cushing’s syndrome, pre-, and post-surgery. Patients with a persistent facial plethora in the post-surgery period were noted to have cortisol levels above 3 mcg/dL, which was predictive of a lack of surgical cure. These subjects had a high facial blood volume fraction, measured by near-infrared multispectral imaging. Increased blood flow (average blood volume fraction) in the facial skin is the cause of plethora observed in the setting of endogenous hypercortisolism [3].
Thoracic Outlet Syndrome due to retrosternal goiter
Clinical finding
Facial plethora due to a goiter is eponymously named after Dr. Hugh Pemberton, who described this classic physical finding in a letter published in Lancet in 1946 titled “sign of a submerged goitre.” He explained the method of eliciting the sign, expected clinical findings, and also proposed a mechanism for the physical finding[4].
The sign is elicited by instructing the patient to lift their arms such that the arms touch both sides of the head. The patient is then instructed to hold their arms in that position until facial congestion or erythema is noticed[4].
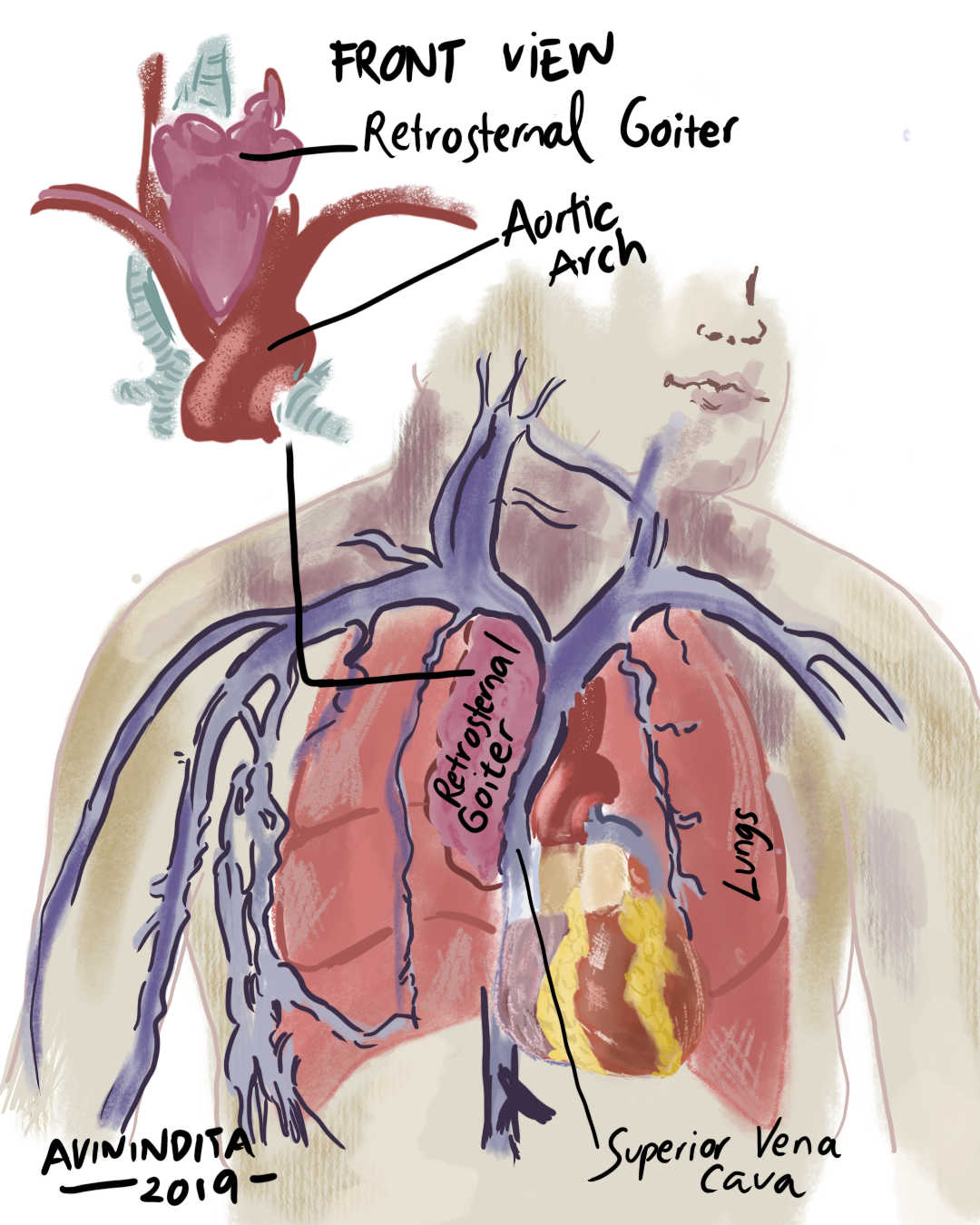
Superior Vena Cava syndrome
Clinical finding
Facial plethora can be caused by an obstruction in the superior vena cava, which is the large vein that carries blood from the head and arms back to the heart.
Mechanism
Superior vena cava syndrome (SVC) is a severe condition that can occur when the flow of blood through the superior vena cava is blocked. This can be caused by a variety of things, including retrosternal goiters (enlarged thyroids behind the breastbone), tumors (lung cancer), inflammation, or blood clot (venous thrombosis).
Increased venous pressure in the cervical vasculature predisposes patients to the cosmetic finding of facial plethora (vascular congestion) and, more importantly, soft-tissue edema and airway compromise[6].
Carcinoid syndrome
Clinical finding
Facial plethora due to carcinoid syndrome classically involves the face, neck, and upper chest[7] and is usually triggered by amine-rich foods, pharmacologic agents, or even emotional stress[8].
Repeated episodes of flushing, which tend to be transient (lasting 10-30 minutes) are characteristic of midgut carcinoids. A longer-lasting duration of flushing (up to several hours) is more characteristic of carcinoids located in the foregut[7].
Pathophysiology
Cutaneous flushing is caused by various vasoactive mediators, including, but not limited to, histamine, substance P, and prostaglandins. Interestingly, serotonin blockers do not improve the pathognomonic flushing associated with carcinoid syndrome. This rules out serotonin as the bioactive hormone involved in the cutaneous flushing of carcinoid syndrome(CS) [9]. The duration of flushing is dependent on the venous drainage of the involved organ. Foregut NETs bypass initial hepatic metabolism; as such, the vasoactive amines persist longer in circulation, resulting in a more prolonged period of flushing. Midgut carcinoids, on the other hand, tend to cause flushing in the setting of hepatic metastases[7].
Pheochromocytoma
Clinical finding
Episodic generalized flushing (including facial plethora) is a known clinical finding in patients with pheochromocytoma[10]. Pheochromocytomas are an unusual cause of isolated facial plethora. On the other hand, the triad of headaches, palpitations, and diaphoresis has a greater utility in patients with this condition[11].
Mechanism
Various vasoactive mediators have been implicated in the etiology of pheochromocytoma-induced facial plethora. Catecholamines (norepinephrine, epinephrine, and dopamine) play this role.
Other endocrine causes of facial plethora and flushing
| Endocrine Condition | Mediators of facial plethora |
| Medullary thyroid carcinoma of the thyroid gland | Calcitonin, prostaglandins, histamine and substance P. |
| Pancreatic neuroendocrine tumor | Vasoactive intestinal peptide, prostacyclin, Gastrin and Prostaglandins. |
| Male hypogonadism (pseudocarcinoid syndrome) | 5-hydroxy-indoleacetic acid (5-HIAA) |
Based on reference(s)[8]
A case series of three patients with male hypogonadism had flushing in the setting of elevated 24hour urine 5-HIAA levels.
Detailed screening for concomitant carcinoid syndrome was negative. Interestingly, both flushing and elevated 24hour urine 5-HIAA resolved with testosterone replacement therapy and recurred after testosterone withdrawal. The authors coined the term pseudocarcinoid syndrome of hypogonadism in their report published in the Mayo Clinic Proceedings [12].
There are a few non-endocrine causes of facial plethora. Their clinical features will be reviewed next.
Mastocytosis
Mastocytosis is a disorder of the skin in which mast cells accumulate in the skin and other tissues.
The facial erythema associated with mastocytosis is thought to be caused by an increase in mast cell numbers in the blood vessels of the face. Treatment for facial plethora typically involves addressing the underlying cause if present.
Rosacea
Rosacea is a chronic skin condition that primarily affects the face. It is characterized by facial flushing, redness, and often pimples.
The clinical findings of this condition are more pronounced in patients with lighter skin tones. Though rosacea can affect people of all ages, it is most common in adults between the ages of 30 and 50. The exact cause of rosacea is unknown, but it is thought to be a combination of genetic and environmental factors. Rosacea is not contagious, and there is no cure for the condition. However, there are treatments available that can help to control the symptoms.
These include topical creams, oral antibiotics, and laser therapy. With proper treatment, rosacea can be managed so that it does not have a significant impact on a person’s life.
Basophilic granulocytic leukemia
Basophilic granulocytic leukemia is a rare myeloproliferative disorder. Histamine, primarily released by basophils mediates facial plethora in this condition.
Other symptoms associated with this rare blood disorder include cold urticaria, generalized urticaria, and colicky abdominal pain.
Sun exposure
Sun exposure can cause facial flushing or blushing in some people. The sun’s ultraviolet (UV) rays cause the blood vessels in the skin to dilate, or expand. This increases blood flow to the skin and can cause the face to turn red. People with fair skin are more likely to experience this reaction than those with darker skin.
Facial flushing caused by sun exposure usually goes away on its own within a few minutes. However, extended sun exposure can lead to more serious effects, such as sunburn or skin cancer.
Emotional blushing
Emotional blushing (facial plethora) is a type of increased blood flow to the face that occurs in response to strong emotions, particularly anxiety.
While it can be embarrassing, emotional blushing is actually a healthy and normal response. In fact, research has shown that people who tend to blush easily are actually more honest and trustworthy than those who don’t. So, if you find yourself blushing often, there’s no need to worry – it’s just your body’s way of showing emotion.
Triggers of facial plethora
Facial plethora (blushing) is a common condition that can be triggered by several different factors. alcohol, spicy foods, and hot drinks can all cause the blood vessels in the face to dilate, resulting in a flushed appearance. Overheating, either from exercise or warm weather, can also lead to facial blushing. In some cases, certain drugs or food additives may cause the blood vessels to widen, resulting in temporary flushing.
Menopause can also cause facial blushing due to fluctuations in hormone levels. While facial plethora is generally harmless, it can be embarrassing and uncomfortable for those who experience it.
Treatment of facial plethora
For endocrine and non-endocrine causes of facial plethora, treatment is based on the underlying cause. For patients with self-limiting causes of facial plethora, treatment typically begins with lifestyle changes, such as avoiding triggers and protecting the skin from the sun.
If these measures are not effective, topical treatments such as corticosteroids or retinoids may be recommended. In some cases, laser therapy or surgery may be necessary to remove dilated blood vessels. With proper treatment, facial plethora can usually be controlled, resulting in a significant improvement in appearance.
References
1. Thiboutot DM. Clinical review 74: Dermatological manifestations of endocrine disorders. J Clin Endocrinol Metab. 1995;80(10):3082-3087. doi:10.1210/jcem.80.10.7559901
2. Nieman LK, Biller BMK, Findling JW, et al. The Diagnosis of Cushing’s Syndrome: An Endocrine Society Clinical Practice Guideline. J Clin Endocrinol Metab. 2008;93(5):1526-1540. doi:10.1210/jc.2008-0125
3. Afshari A, Ardeshirpour Y, Lodish MB, et al. Facial Plethora: Modern Technology for Quantifying an Ancient Clinical Sign and Its Use in Cushing Syndrome. J Clin Endocrinol Metab. 2015;100(10):3928-3933. doi:10.1210/jc.2015-2497
4. Pemberton HS. Sign of submerged goitre. The Lancet. 1946;248(6423):509. doi:10.1016/S0140-6736(46)91790-4
5. De Filippis EA, Sabet A, Sun MRM, Garber JR. Pemberton’s Sign: Explained Nearly 70 Years Later. J Clin Endocrinol Metab. 2014;99(6):1949-1954. doi:10.1210/jc.2013-4240
6. Ratnarathorn M, Craig E. Cutaneous findings leading to a diagnosis of superior vena cava syndrome: A case report and review of the literature. Dermatol Online J. 2011;17(6). doi:10.5070/D37kw6z5kj
7. Liu EH, Solorzano CC, Katznelson L, Vinik AI, Wong R, Randolph G. AACE/ACE Disease state clinical review: Diagnosis and management of midgut carcinoids. Endocr Pract Off J Am Coll Endocrinol Am Assoc Clin Endocrinol. 2015;21(5):534-545. doi:10.4158/EP14464.DSC
8. Hannah-Shmouni F, Stratakis CA, Koch CA. Flushing in (Neuro)endocrinology. Rev Endocr Metab Disord. 2016;17(3):373-380. doi:10.1007/s11154-016-9394-8
9. Ito T, Lee L, Jensen RT. Carcinoid-syndrome: recent advances, current status and controversies. Curr Opin Endocrinol Diabetes Obes. 2018;25(1):22. doi:10.1097/MED.0000000000000376
10. Shah NH, Ruan DT. Pheochromocytoma. Circulation. 2014;130(15):1295-1298. doi:10.1161/CIRCULATIONAHA.114.008544
11. Heymann WR. Flushing, pheochromocytoma, and the dermatologist. J Am Acad Dermatol. 2006;55(6):1075-1077. doi:10.1016/j.jaad.2006.07.008
12. Shakir KMM, Jasser MZ, Yoshihashi AK, Drake AJ, Eisold JF. Pseudocarcinoid Syndrome Associated With Hypogonadism and Response to Testosterone Therapy. Mayo Clin Proc. 1996;71(12):1145-1149. doi:10.4065/71.12.1145
Images(s) Courtesy
MyEndoConsult
Kindly Let Us Know If This Was helpful? Thank You!


