The Ferriman Gallwey score is a numerical scoring assessment used to evaluate the severity of hirsutism in women. The score ranges from 0 to 4, with 0 being no hair growth and 4 being severe hair growth.
A woman’s Ferriman Gallwey score is calculated by adding up the number of areas on her body where she has excess hair growth. The areas that are counted include the upper lip, chin, chest, back, abdomen, thighs, and arms.
Ferriman-Gallwey Score Calculator
This scoring system evaluates eleven different body parts, with scores ranging from zero (no excessive terminal hair growth visible) to four (extensive hair growth visible) for each body part evaluated.
The original Ferriman Gallwey scoring system, an objective means of assessing the degree of hirsutism at the bedside, was first published by D. Ferriman and Gallwey in an article published in the journal of clinical endocrinology and metabolism in 1961. It can be caused by an underlying medical condition, such as polycystic ovary syndrome (PCOS), or it can be a side effect of certain medications, such as testosterone replacement therapy. Hirsutism can also occur in healthy women with no known cause.
The modified Ferriman Gallway score
The original assessment of hirsutism using the Ferriman-Gallway score assigned a grade ranging from 0 to 4, depending on the presence and extent of terminal hair distribution involving 11 anatomic sites [1]. A score of 0 (no hair growth) to 4 (severe hair growth) at each anatomic site.
To calculate the Ferriman-Gallwey score, simply add up the scores for each of the 9 body areas. It is a quick and easy way to estimate the degree of hirsutism in women. The score ranges from 0-36, with a higher score indicating more severe hirsutism. A total score of 8 or more is generally considered to be indicative of hirsutism.
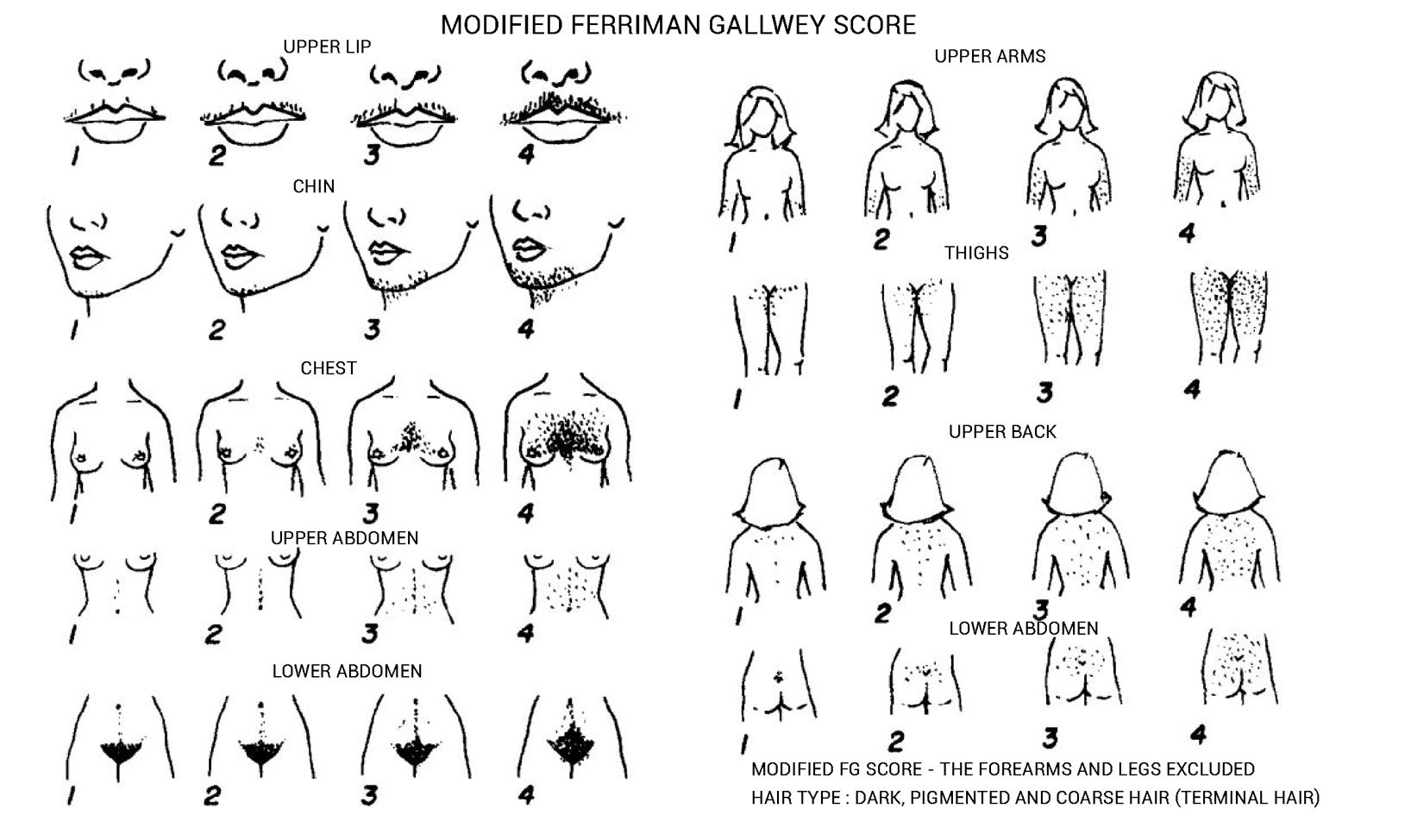
A chart for visually scoring hirsutism.
The Ferriman Gallwey score is based on the assessment of 9 body sites
- Upper lip
- Chin
- Chest
- Upper back
- Lower back
- Upper abdomen
- Lower abdomen
- Upper arms
- Forearms (not included in the modified Ferriman Gallwey score)
- Thighs
- Legs (not included in the modified Ferriman Gallwey score)
The forearm and lower leg have been excluded from the modified score since terminal hair growth in these areas is inconsistently associated with hyperandrogenemia. In certain Eastern ethnicities, hair in this area is also a normal variant. The modified Ferriman-Gallway score objectively assesses 9 anatomic regions for evidence of terminal hair growth [2]. A modified Ferriman-Gallway score of ≥8 is consistent with clinically significant hirsutism [3,4].
Goodman et al. proposed a hirsutism scoring system based on a further modification of this score in a paper published in 2001. This suggests scoring additional sites, including the sides of the face, neck, gluteal, inguinal, etc. This modification to the original score is barely utilized in routine clinical practice. A cardinal reason for its lack of adoption may be that applying it in a busy endocrine practice is cumbersome. Of note, it increases the sites of assessment from 11 to 19.
Types of hair growth in normal physiology
Classification based on androgen dependence
Most of the hair on the body is androgen-dependent (sexual hair) except hair present in the nostrils, lateral and occipital areas of the scalp, eyelashes, and nostrils (asexual hair). Pubic (perineal) and axillary hair, although androgen-dependent, is present in both sexes and is conventionally referred to as ambosexual hair.
Classification based on morphology
Terminal hair – This is thick, pigmented hair present in androgen-dependent regions of the body
Vellus hair – This is thin, unpigmented hair which is fairly distributed all over the body.
What is hirsutism?
Hirsutism is defined as the presence of terminal, pigmented hair in a male-pattern (androgen-dependent) distribution. Although axillary and perineal hair represents androgen-dependent areas, they are present in both sexes and thus do not fall under the “male pattern”.
It is a common dermatologic manifestation of polycystic ovary syndrome (PCOS) with a reported prevalence of 50-70% [5]. Conversely, hypertrichosis refers to the proliferation of light unpigmented hair in non-androgen dependent (non-sexual) regions of the body.
Endocrine causes of hirsutism or virilization
Every patient evaluated for new-onset hirsutism should have an assessment of serum testosterone. Testosterone levels >150 ng/dL suggest possible androgen producing tumors.
- Adrenal tumors
- Cushing’s syndrome
- Classic and non-classic congenital adrenal hyperplasia
- Hyperandrogenism, insulin resistance, acanthosis nigricans (HAIR-AN syndrome)
- Ovarian hyperthecosis
- Ovarian tumors
- The features of virilization include acne, male pattern baldness, deep male voice, and clitoral enlargement
- Idiopathic hirsutism
- Polycystic ovarian syndrome
- Other androgen excess states
Pathophysiology of hirsutism in excess androgen states
Circulating androgens are responsible for hirsutism, although the degree of hirsutism is not necessarily determined by the severity of hyperandrogenemia. This has been attributed to interindividual differences in the response of hair follicles to androgens [5]
Hirsutism, like acne, and male pattern alopecia is dependent on the local abundance of 5-α-reductase (which reduces testosterone to active dihydrotestosterone) in the pilosebaceous unit [6].
The local concentration of 5-α-reductase in the skin varies by ethnicity. For example, hirsutism tends to be more common in women of Mediterranean background and less frequent and milder in women of East Asian or Native-American background [7–9].
Reference
1. Ferriman D, Gallwey JD. Clinical assessment of body hair growth in women. J Clin Endocrinol Metab. 1961;21:1440-1447. doi:10.1210/jcem-21-11-1440
2. Cook H, Brennan K, Azziz R. Reanalyzing the modified ferriman-gallwey score: is there a simpler method for assessing the extent of hirsutism? Fertil Steril. 2011;96(5):1266-1270.e1. doi:10.1016/j.fertnstert.2011.08.022
3. Aswini R, Jayapalan S. Modified Ferriman–Gallwey Score in Hirsutism and its Association with Metabolic Syndrome. Int J Trichology. 2017;9(1):7-13. doi:10.4103/ijt.ijt_93_16
4. Hatch R, Rosenfield RL, Kim MH, Tredway D. Hirsutism: implications, etiology, and management. Am J Obstet Gynecol. 1981;140(7):815-830.
5. Feng JG, Guo Y, Ma LA, Xing J, Sun RF, Zhu W. Prevalence of dermatologic manifestations and metabolic biomarkers in women with polycystic ovary syndrome in north China. J Cosmet Dermatol. 2018;17(3):511-517. doi:10.1111/jocd.12387
6. Rosenfield RL. Clinical practice. Hirsutism. N Engl J Med. 2005;353(24):2578-2588. doi:10.1056/NEJMcp033496
7. Coskun A, Ercan O, Arikan DC, et al. Modified Ferriman–Gallwey hirsutism score and androgen levels in Turkish women. Eur J Obstet Gynecol Reprod Biol. 2011;154(2):167-171. doi:10.1016/j.ejogrb.2010.10.001
8. Escobar-Morreale HF, Carmina E, Dewailly D, et al. Epidemiology, diagnosis and management of hirsutism: a consensus statement by the Androgen Excess and Polycystic Ovary Syndrome Society. Hum Reprod Update. 2012;18(2):146-170. doi:10.1093/humupd/dmr042
9. Martin KA, Anderson RR, Chang RJ, et al. Evaluation and Treatment of Hirsutism in Premenopausal Women: An Endocrine Society Clinical Practice Guideline. J Clin Endocrinol Metab. 2018;103(4):1233-1257. doi:10.1210/jc.2018-00241
Kindly Let Us Know If This Was helpful? Thank You!


