What are insulin pumps?
Insulin pumps are sophisticated devices designed to administer precise doses of insulin over a 24-hour period. They operate with a compact and portable electrochemical pump and have a reservoir that holds a certain volume of insulin (typically between 2 and 3 ml at a concentration of 100 units per milliliter), depending on the brand of insulin. This insulin is then gradually delivered to subcutaneous tissues through a flexible tube and a small cannula.
These pumps consistently distribute insulin in the form of microboluses every few minutes throughout a 24-hour cycle. Importantly, only rapid-acting insulin analogs are utilized by these pumps, delivered in two distinct patterns: one is a pre-set continuous flow that forms the basal (background) insulin rate, and the other is a larger amount released in response to immediate insulin requirements, such as during meals or when high blood sugar levels need to be corrected.
One of the principal advantages insulin pumps have over the regimen of multiple daily insulin injections (MDI) is their ability to administer minuscule and adjustable amounts of insulin that can be tailored to the individual’s needs during different parts of the day and night. This flexibility enables pre-planned and immediate adjustments to insulin delivery. For example, the pump can be programmed to increase the insulin delivery rate overnight to mitigate the “dawn phenomenon” (an early morning rise in blood sugar levels) or to reduce the insulin infusion rate after a period of physical activity.
Criteria for Candidate Selection
The ADA standards of care propose the option of a pump for both children and adults diagnosed with type 1 diabetes. Criteria include individuals who cannot achieve an optimal HbA1c target even with an intensified regimen of multiple daily injections (MDI) involving quick-acting and extended-release insulin analogs; those who have experienced intense hypoglycemia or persistent life-changing hypoglycemia; and pregnant women who cannot reach the desired blood sugar and HbA1c targets despite an intense MDI regime.
For children with type 1 diabetes, pump therapy may be considered if MDI proves to be unsuitable or unmanageable. AACE consensus suggests that pump therapy could be beneficial for patients with a HbA1c value greater than 7% (53 mmol/mol), when blood glucose levels fluctuate drastically before meals, or when they face the dawn phenomenon with fasting glucose levels exceeding 200 mg/dl (11 mmol/L) that cannot be controlled with an MDI regimen. Other potential indications could include repeated occurrences of ketoacidosis, ignorance of hypoglycemia, a refusal to administer multiple injections, or a personal preference for the pump.
Given the high costs associated with pump therapy, the benefits of this treatment must be weighed against its cost individually. Typically, a pump user can be proactive in managing his diabetes, adjusting the insulin according to the carbohydrate content in their meals, using an optimized MDI regimen, and performing regular self-monitoring of blood glucose levels, typically four times daily.
Choosing the Appropriate Pump
Insulin pumps vary in their features. They can be tethered pumps, which are linked via an external tube to a cannula, or patch pumps, which contain a short tube and cannula integrated into a small pump device operated by a handheld remote control. Tethered pumps are more commonly used, but patch pumps offer the advantage of being smaller and more discreet, allowing easier changes and presenting a lower risk of tube dysfunction. However, patch pumps are yet to provide the capability for continuous glucose sensor pairing.
Pumps also differ in size, reservoir capacity (2-3 ml), battery life, ability to download data wirelessly, compatibility with glucose meters, number of basal rates per day, duration and shape, bolus calculator feature, and compatibility with various types of cannula.
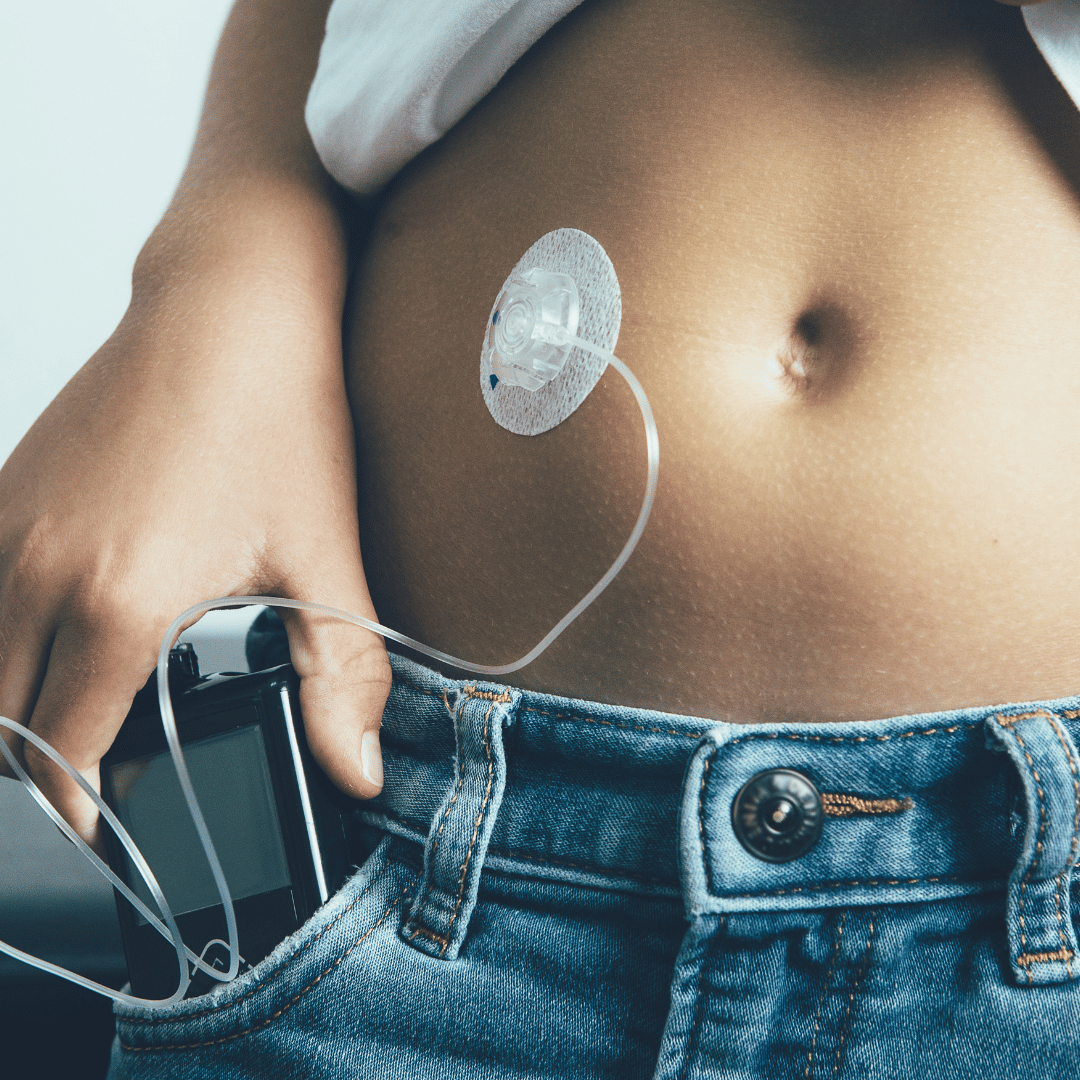
Selection and Management of the Infusion Set and Insulin Reservoir
An infusion set consists of tubing and a cannula. The length of the tubing, ranging from 24 to 42 inches, depends on the patient’s height and the location of the cannula and the pump during the day. This tubing features a disconnection mechanism that allows the pump to be temporarily removed for activities such as showering, swimming, or participating in sports.
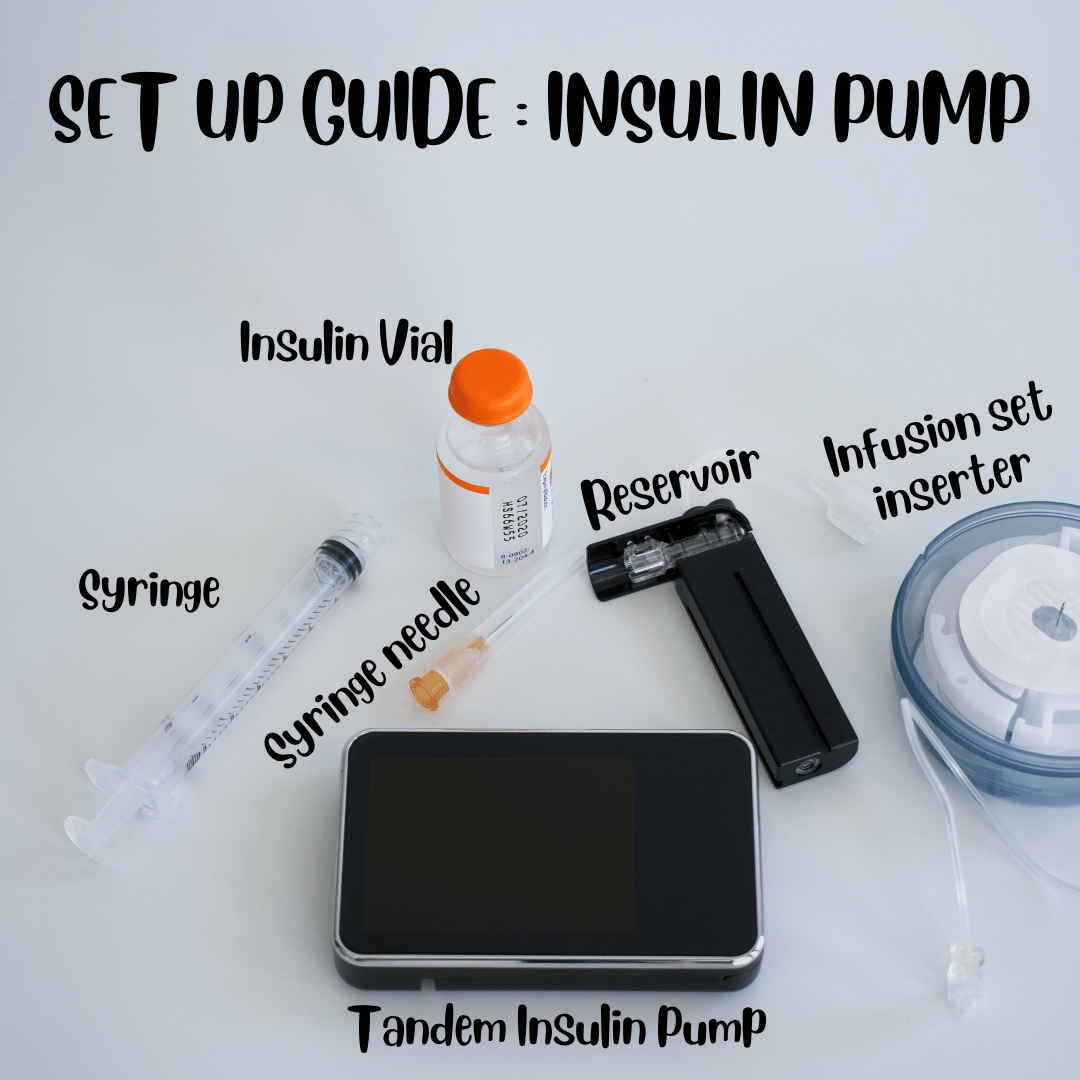
Cannulas, which are inserted into the subcutaneous tissue, come in various types: some are soft and flexible, made from Teflon, while others are made of steel. These are easier to insert and less likely to become twisted or bent. Angled cannulas (20–40°) are more suitable for thinner patients and are also less prone to kinking. However, perpendicular cannulas (90 °) are shorter and more suitable for insertion into the arm, hip, or buttock. The length of a perpendicular cannula ranges from 6-12 mm and an angled cannula is typically 17 mm. Longer cannulas are more suitable for patients with a higher BMI and those who require higher doses of insulin.
When choosing a pump, the size of the insulin reservoir should be considered, as it varies depending on daily insulin needs. For most people with type 1 diabetes, a reservoir of approximately 2 ml is adequate, while those with type 2 diabetes often need a reservoir of 3 ml to ensure sufficient insulin supply and avoid frequent refills. The infusion set should be replaced every 3 days to prevent infection at the site and insulin degradation. The site of insertion should also be alternated regularly between the abdomen, thigh, buttocks, and arm areas.
Meal planning with insulin pumps
The size of the boluses should be proportional to the amount of carbohydrates consumed at each meal. The dose is recommended based on an insulin-to-carbohydrate ratio (ICR) that is pre-programmed for a 24-hour period. This ratio may already be established in individuals previously using MDI and is typically customized to breakfast, lunch, and dinner times.
When such ratios are unknown, a rough estimation can be made using the “500 rule”, which involves dividing 500 by the total daily dose (TDD) in units. This gives the amount of carbohydrates that corresponds to a bolus of 1 unit of insulin. For children, the same calculation can be done using “300” instead of 500.
The dose of bolus can also account for the amount of insulin needed to correct for fasting hyperglycemia above the desired blood glucose target. Insulin sensitivity factor (ISF), which is the predicted decrease in blood glucose induced by 1 unit of insulin, is determined individually. The ISF can be determined by the “1800 rule”, which involves dividing 1800 by the TDD in units.
After these variables are determined – ICR, ISF, and the blood glucose target – they should be entered into the bolus calculator for a daytime period, along with the active insulin time. This is the duration of action of a quantity of insulin administered, and 3 hours is a typical average. With these data, the bolus calculator can calculate the amount of active insulin (“on board” insulin) required at any time of day. The use of a bolus calculator has been shown to help lower post-meal blood glucose levels in patients using pump therapy.
Engaging in Physical Activities while using an Insulin Pump
The rate of glucose use by muscles and insulin absorption increases during and after physical activities. This leads to a potential risk of hypoglycemia or low blood sugar levels. As a result, it is crucial to adjust the insulin supply of the pump and potentially load on carbohydrates when planning to exercise.
In practical terms, this can mean reducing the basal (continuous) rate of insulin delivery by the pump by approximately 30–50% about an hour before and during physical activity. Another approach is to reduce the premeal bolus (single, larger dose) by 25–75% of the usual dose if exercise is planned soon after eating.
For intense workouts or if blood sugar levels are already low normal, prior to starting the activity, it is advisable to consume fast-acting carbohydrates. A good rule of thumb is to have about 20 grams of these carbohydrates before and/or during exercise. These measures are designed to prevent hypoglycemia while maintaining adequate energy levels during physical activities.
There are potential complications that patients who use insulin pumps may experience. These can include tube damage or breakage, blockages in the tube or cannula, leakage at the infusion site, presence of air bubbles in the tube or reservoir, subcutaneous nodules forming at the catheter site, sensitivity to the adhesive on the skin, skin infections, and pump malfunctions of the pump itself.
Any interruption in insulin delivery, regardless of the cause, could increase the risk of diabetic ketoacidosis in patients with type 1 diabetes with insulin pumps.
To mitigate these potential issues, it is advised to regularly inspect the infusion site and tubing. The infusion site should be changed every 2 to 3 days, adhering to a rotation of sites to avoid skin irritation or infection. Additionally, the skin should be cleaned with each change in infusion set.
If unexplained high blood sugar levels are observed, it may indicate a malfunction of the device or the infusion set, which should be promptly addressed.
Understanding Insulin Pump Technology: Definition and Key Features
Insulin pumps are compact electronic devices designed to administer a pre-set quantity of insulin around the clock. These devices house a reservoir, typically carrying between 2 and 3 milliliters of insulin at a concentration of 100 units per milliliter. This insulin is then conveyed through a flexible plastic tube into a cannula (a small, thin tube) implanted into the subcutaneous tissue under the skin.
Throughout the day and night, the pump continually distributes small amounts of insulin in the form of microboluses every few minutes. Insulin used in these devices is limited to rapid-acting insulin analogs, delivered in two primary ways: first, as a constant flow that constitutes the basal (background) insulin rate, and second, as a larger burst, or bolus, to manage the immediate need for insulin during meals or when blood glucose levels rise.
One of the key advantages of insulin pumps over multiple daily insulin injections (MDI) is their ability to disdispense minuscule amounts of insulin, allowing for precise tailoring to the user’s specific requirements throughout different periods of the day and night. This capability enables both planned and immediate adjustments in insulin delivery to accommodate various situations. For example, the insulin delivery rate can be raised overnight to counteract the “dawn phenomenon” (a natural increase in blood sugar levels in the early morning) or decreased after a round of physical exercise.
Conclusion
In conclusion, insulin pumps provide an advanced, adaptable, and precision-based solution for managing blood glucose levels in patients with type 1 and type 2 diabetes. Their unique functionality enables the continuous delivery of insulin in pre-programmed amounts, adapting to varying daytime or nighttime requirements. This dynamic tool presents notable advantages over multiple daily injections (MDI) by offering more personalized control over insulin administration. Furthermore, it grants patients the flexibility to adjust their insulin delivery according to specific activities or conditions, such as physical exercise or the dawn phenomenon. However, careful consideration must be given to the potential for device-related adverse events, requiring diligent management and regular monitoring. As technology continues to evolve, the insulin pump’s capacity for improving the lives of those living with diabetes promises further enhancements and advancements.
References
- Grunberger, G., Bailey, T. S., Cohen, A. J., et al. (2010). Statement by the American Association of Clinical Endocrinologists Consensus Panel on insulin pump management. Endocrine Practice, 16(5), 746–762.
- Shashaj, B., Busetto, E., Sulli, N. (2008). Benefits of a bolus calculator in pre- and postprandial glycemic control and meal flexibility of pediatric patients using continuous subcutaneous insulin infusion (CSII). Diabetic Medicine, 25, 1036–1042.
- Bergenstal, R. M., Tamborlane, W. V., Ahmann, A., et al. (2010). Effectiveness of sensor-augmented insulin-pump therapy in type 1 diabetes. New England Journal of Medicine, 363(4), 311–320.
- Pickup, J. C. (2012). Management of diabetes mellitus: is the pump mightier than the pen? Nature Reviews Endocrinology, 8(7), 425–433.
Kindly Let Us Know If This Was helpful? Thank You!


